What does heavy bleeding mean? The first symptoms and causes of uterine bleeding in women. If there is bleeding, how to stop the bleeding
Uterine bleeding is the release of blood from uterus. Unlike menstruation, with uterine bleeding, either the duration of discharge and the volume of blood released changes, or their regularity is disrupted.Causes of uterine bleeding
 Causes of uterine bleeding may be different. They are often caused by diseases of the uterus and appendages, such as fibroids, endometriosis, adenomyosis), benign and malignant tumors. Bleeding can also occur as a complication of pregnancy and childbirth. In addition, there are dysfunctional uterine bleeding - when, without visible pathology of the genital organs, their function is disrupted. They are associated with a violation of the production of hormones that affect the genital organs (disorders in the hypothalamus-pituitary-ovarian system).
Causes of uterine bleeding may be different. They are often caused by diseases of the uterus and appendages, such as fibroids, endometriosis, adenomyosis), benign and malignant tumors. Bleeding can also occur as a complication of pregnancy and childbirth. In addition, there are dysfunctional uterine bleeding - when, without visible pathology of the genital organs, their function is disrupted. They are associated with a violation of the production of hormones that affect the genital organs (disorders in the hypothalamus-pituitary-ovarian system). Much less often, the cause of this pathology can be so-called extragenital diseases (not related to the genital organs). Uterine bleeding can occur with liver damage, with diseases associated with blood clotting disorders (for example, von Willebrand's disease). In this case, in addition to the uterine, patients are also worried about nosebleeds, bleeding gums, the appearance of bruises with minor injuries, prolonged bleeding for cuts and others symptoms.
Symptoms of uterine bleeding
The main symptom of this pathology is bleeding from the vagina.Unlike normal menstruation, uterine bleeding is characterized by the following features:
1.
Increased blood volume. Normally, during menstruation, 40 to 80 ml of blood is released. With uterine bleeding, the volume of blood lost increases, amounting to more than 80 ml. This can be determined if there is a need to change hygiene products too often (every 0.5 - 2 hours).
2.
Increased duration of bleeding. Normally, during menstruation, discharge lasts from 3 to 7 days. In case of uterine bleeding, the duration of bleeding exceeds 7 days.
3.
Irregularity of discharge - on average, the menstrual cycle is 21-35 days. An increase or decrease in this interval indicates bleeding.
4.
Bleeding after sexual intercourse.
5.
Bleeding in postmenopause - at an age when menstruation has already stopped.
Thus, we can distinguish following symptoms uterine bleeding:
- Menorrhagia (hypermenorrhea)- excessive (more than 80 ml) and long periods(more than 7 days), their regularity remains the same (occurs after 21-35 days).
- Metrorrhagia– irregular bloody issues. They occur more often in the middle of the cycle, and are not very intense.
- Menometrorrhagia– prolonged and irregular bleeding.
- Polymenorrhea– menstruation occurring more frequently than every 21 days.
Types of uterine bleeding
Depending on the time of occurrence, uterine bleeding can be divided into the following types:1. Uterine bleeding during the newborn period is scanty bloody discharge from the vagina, occurring most often in the first week of life. They are connected with what happens during this period abrupt change hormonal background. They go away on their own and do not require treatment.
2. Uterine bleeding in the first decade (before the onset of puberty) is rare and is associated with ovarian tumors that can secrete increased amount sex hormones (hormonally active tumors). Thus, so-called false puberty occurs.
3. Juvenile uterine bleeding - occurs at the age of 12-18 years (puberty).
4. Bleeding during the reproductive period (ages 18 to 45) can be dysfunctional, organic, or associated with pregnancy and childbirth.
5. Uterine bleeding in menopause– caused by impaired hormone production or diseases of the genital organs.
Depending on the cause of occurrence, uterine bleeding is divided into:
- Dysfunctional bleeding(can be ovulatory or anovulatory).
- Organic bleeding- associated with pathology of the genital organs or systemic diseases (for example, diseases of the blood, liver, etc.).
- Iatrogenic bleeding– arise as a result of taking non-hormonal and hormonal contraceptives, blood thinning drugs, due to the installation of intrauterine devices.
Juvenile uterine bleeding
 Juvenile uterine bleeding develops during puberty (age 12 to 18 years). Most often, the cause of bleeding in this period is ovarian dysfunction - the proper production of hormones is adversely affected by chronic infections, frequent acute respiratory viral infections, psychological trauma, physical exercise, unhealthy diet. Their occurrence is characterized by seasonality - winter and spring months. Bleeding in most cases is anovulatory – i.e. due to disruption of hormone production, ovulation does not occur. Sometimes the cause of bleeding can be bleeding disorders, tumors of the ovaries, body and cervix, tuberculosis of the genital organs.
Juvenile uterine bleeding develops during puberty (age 12 to 18 years). Most often, the cause of bleeding in this period is ovarian dysfunction - the proper production of hormones is adversely affected by chronic infections, frequent acute respiratory viral infections, psychological trauma, physical exercise, unhealthy diet. Their occurrence is characterized by seasonality - winter and spring months. Bleeding in most cases is anovulatory – i.e. due to disruption of hormone production, ovulation does not occur. Sometimes the cause of bleeding can be bleeding disorders, tumors of the ovaries, body and cervix, tuberculosis of the genital organs. The duration and intensity of juvenile bleeding may vary. Heavy and prolonged bleeding leads to anemia, which is manifested by weakness, shortness of breath, pallor and other symptoms. In any case of bleeding in adolescence treatment and observation should take place in a hospital setting. If bleeding occurs at home, you can ensure rest and bed rest, give 1-2 tablets of Vikasol, put a cold heating pad on the lower abdomen and call an ambulance.
Treatment, depending on the condition, can be symptomatic - the following remedies are used:
- hemostatic drugs: dicinone, vikasol, aminocaproic acid;
- uterine contractants (oxytocin);
- iron supplements;
- physiotherapeutic procedures.
To prevent recurrent bleeding, courses of vitamins, physiotherapy, and acupuncture are prescribed. After stopping the bleeding, estrogen-progestin agents are prescribed to restore normal menstrual cycle. Great value in recovery period has hardening and physical exercise, proper nutrition, treatment of chronic infections.
Uterine bleeding during the reproductive period
During the reproductive period, there are quite a few reasons that cause uterine bleeding. Basically, these are dysfunctional factors - when a violation of the correct production of hormones occurs after abortion, against the background of endocrine, infectious diseases, stress, intoxication, taking certain medicines.During pregnancy, in the early stages, uterine bleeding can be a manifestation of miscarriage or ectopic pregnancy. On later bleeding is caused by placenta previa, hydatidiform mole. During childbirth, uterine bleeding is especially dangerous; the amount of blood loss can be large. A common cause of bleeding during childbirth is placental abruption, atony or hypotension of the uterus. IN postpartum period Bleeding occurs due to parts of the membranes remaining in the uterus, uterine hypotension or bleeding disorders.
Often the causes of uterine bleeding in childbearing period Various diseases of the uterus can cause:
- myoma;
- endometriosis of the uterine body;
- benign and malignant tumors of the body and cervix;
- chronic endometritis (inflammation of the uterus);
- hormonally active ovarian tumors.
Bleeding associated with pregnancy and childbirth
 In the first half of pregnancy, uterine bleeding occurs when there is a threat of interruption of a normal or ectopic pregnancy. These conditions are characterized by pain in the lower abdomen, delayed menstruation, as well as subjective signs of pregnancy. In any case, if there is bleeding after pregnancy is established, you should urgently seek medical help. In the initial stages of spontaneous miscarriage when started on time and active treatment pregnancy can be maintained. On later stages there is a need for curettage.
In the first half of pregnancy, uterine bleeding occurs when there is a threat of interruption of a normal or ectopic pregnancy. These conditions are characterized by pain in the lower abdomen, delayed menstruation, as well as subjective signs of pregnancy. In any case, if there is bleeding after pregnancy is established, you should urgently seek medical help. In the initial stages of spontaneous miscarriage when started on time and active treatment pregnancy can be maintained. On later stages there is a need for curettage. An ectopic pregnancy can develop in the fallopian tubes and cervix. At the first signs of bleeding, accompanied by subjective symptoms of pregnancy against the background of even a slight delay in menstruation, it is necessary to urgently seek medical help.
In the second half of pregnancy, bleeding poses a great danger to the life of the mother and fetus, so it requires urgent medical attention. Bleeding occurs when placenta previa (when the placenta does not form along the back wall of the uterus, but partially or completely blocks the entrance to the uterus), abruption of a normally located placenta, or uterine rupture. In such cases, the bleeding may be internal or external, and requires an emergency caesarean section. Women at risk of such conditions should be under close medical supervision.
During childbirth, bleeding is also associated with placental previa or placental abruption. In the postpartum period, common causes of bleeding are:
- decreased uterine tone and ability to contract;
- parts of the placenta remaining in the uterus;
- bleeding disorders.
Uterine bleeding during menopause
During menopause, hormonal changes in the body occur, and uterine bleeding occurs quite often. Despite this, they can become a manifestation of more serious illnesses, such as benign (fibroids, polyps) or malignant neoplasms. You should be especially wary of the appearance of bleeding in postmenopause, when menstruation has already completely stopped. It is extremely important to see a doctor at the first sign of bleeding because... In the early stages, tumor processes are more treatable. For diagnostic purposes, separate diagnostic curettage canal of the cervix and body of the uterus. Then a histological examination of the scraping is carried out to determine the cause of the bleeding. In case of dysfunctional uterine bleeding it is necessary to select the optimal hormonal therapy.Dysfunctional uterine bleeding
Dysfunctional bleeding is one of the most common types of uterine bleeding. They can occur at any age - from puberty to menopause. The reason for their occurrence is a disruption in the production of hormones by the endocrine system - a malfunction of the hypothalamus, pituitary gland, ovaries or adrenal glands. This a complex system regulates the production of hormones that determine the regularity and duration of menstrual bleeding. Dysfunction of this system can be caused by the following pathologies:- spicy and chronic inflammation genital organs (ovaries, appendages, uterus);
- endocrine diseases (thyroid dysfunction, diabetes, obesity);
- stress;
- physical and mental fatigue;
- climate change.
Very often, dysfunctional bleeding is a consequence of artificial or spontaneous abortion.
Dysfunctional uterine bleeding can be:
1.
Ovulatory – associated with menstruation.
2.
Anovulatory – occurs between menstruation.
At ovulatory bleeding There are deviations in the duration and volume of blood released during menstruation. Anovulatory bleeding is not associated with the menstrual cycle and most often occurs after a missed period, or less than 21 days after the last menstrual period.
Ovarian dysfunction can cause infertility and miscarriage, so it is extremely important to consult a doctor promptly if any menstrual irregularities occur.
Breakthrough uterine bleeding
 Uterine bleeding that occurs while taking hormonal contraceptives is called breakthrough bleeding. Such bleeding may be minor, which is a sign of a period of adaptation to the drug.
Uterine bleeding that occurs while taking hormonal contraceptives is called breakthrough bleeding. Such bleeding may be minor, which is a sign of a period of adaptation to the drug. In such cases, you should consult a doctor to review the dose of the drug used. Most often, if breakthrough bleeding occurs, it is recommended to temporarily increase the dose of the drug taken. If the bleeding does not stop or becomes more profuse, additional examination should be carried out, since the cause may be various diseases of the reproductive system. Bleeding can also occur if the walls of the uterus are damaged by the intrauterine device. In this case, it is necessary to remove the spiral as soon as possible.
Which doctor should I contact if I have uterine bleeding?
If uterine bleeding occurs, regardless of the age of the woman or girl, you should contact gynecologist (make an appointment). If uterine bleeding begins in a girl or young girl, it is advisable to contact a pediatric gynecologist. But if for some reason it is impossible to get to one, then you should contact a regular gynecologist antenatal clinic or a private clinic.Unfortunately, uterine bleeding can be a sign not only of long-term chronic disease internal genital organs of a woman, which requires routine examination and treatment, but also symptoms emergency. Emergency conditions mean acute diseases, in which a woman needs urgent qualified medical care to save her life. And if such help emergency bleeding will not be provided, the woman will die.
Accordingly, you need to contact a gynecologist at the clinic for uterine bleeding when there are no signs of an emergency. If uterine bleeding is combined with signs of an emergency condition, then you should immediately call an ambulance or use your own transport to as soon as possible get to the nearest hospital with gynecological department. Let's consider in what cases uterine bleeding should be considered as an emergency.
First of all, all women should know that uterine bleeding at any stage of pregnancy (even if the pregnancy is not confirmed, but there is a delay of at least a week) should be considered an emergency condition, since the release of blood, as a rule, is provoked by threats to the life of the fetus and future mothers with conditions such as placental abruption, miscarriage, etc. And in such conditions, a woman should be provided with qualified assistance to save her life and, if possible, preserve the life of the gestating fetus.
Secondly, uterine bleeding that begins during or some time after sexual intercourse should be considered a sign of an emergency. Such bleeding may be due to pregnancy pathology or severe injuries genitals during previous intercourse. In such a situation, help for a woman is vital, since in her absence the bleeding will not stop, and the woman will die from blood loss incompatible with life. To stop bleeding in such a situation, it is necessary to sutured all ruptures and injuries to the internal genital organs or terminate the pregnancy.
Thirdly, uterine bleeding, which turns out to be profuse, does not decrease over time, and is combined with severe pain in the lower abdomen or lower back, causes a sharp deterioration in health, paleness, decreased blood pressure, palpitations, increased sweating, and possibly fainting. General characteristics emergency condition due to uterine bleeding is a fact sharp deterioration a woman’s well-being when she cannot perform simple household and everyday actions (she cannot stand up, turn her head, it is difficult for her to speak, if she tries to sit up in bed, she immediately falls, etc.), but literally lies flat or is even unconscious.
What tests and examinations can a doctor prescribe for uterine bleeding?
Although uterine bleeding can be caused by various diseases, when they appear, the same examination methods are used (tests and instrumental diagnostics). This is due to the fact that the pathological process during uterine bleeding is localized in the same organs - the uterus or ovaries.Moreover, at the first stage, various examinations are carried out to assess the condition of the uterus, since most often uterine bleeding is caused by the pathology of this particular organ. And only if, after the examination, the pathology of the uterus was not detected, methods of examining the functioning of the ovaries are used, since in such a situation the bleeding is caused by a disorder of the regulatory function of the ovaries. That is, the ovaries do not produce required amount hormones in different periods menstrual cycle, causing bleeding as a response to hormonal imbalance.
So, in case of uterine bleeding, first of all the doctor prescribes the following tests and examinations:
- General blood analysis ;
- Coagulogram (indicators of the blood coagulation system) (sign up);
- Gynecological examination (make an appointment) and inspection in mirrors;
- Ultrasound of the pelvic organs (sign up).
A coagulogram allows you to evaluate the functioning of the blood coagulation system. And if the coagulogram parameters are not normal, then the woman should consult and undergo necessary treatment at hematologist (make an appointment).
Gynecological examination allow the doctor to feel with his hands various neoplasms in the uterus and ovaries, to determine the presence of an inflammatory process by changes in the consistency of the organs. And examination in the mirrors allows you to see the cervix and vagina, identify neoplasms in the cervical canal or suspect cervical cancer.
Ultrasound is highly informative method, allowing to identify inflammatory processes, tumors, cysts, polyps in the uterus and ovaries, endometrial hyperplasia, as well as endometriosis. That is, in fact, ultrasound allows you to identify almost all diseases that can cause uterine bleeding. But, unfortunately, the information content of ultrasound is not sufficient for final diagnosis, since this method only provides guidance in the diagnosis - for example, ultrasound can identify uterine fibroids or endometriosis, but it is impossible to establish the exact location of the tumor or ectopic foci, determine their type and assess the condition of the organ and surrounding tissues. Thus, ultrasound allows one to determine the type of existing pathology, but to clarify its various parameters and determine the causes of this disease it is necessary to use other examination methods.
When a gynecological examination, speculum examination, ultrasound, and a general blood test and coagulogram will be performed, it depends on what pathological process was identified in the genital organs. Based on these examinations, the doctor may prescribe the following diagnostic procedures:
- Separate diagnostic curettage (sign up);
- Hysteroscopy (sign up);
- Magnetic resonance imaging (sign up).
If fibroids or other uterine tumors are detected, the doctor prescribes hysteroscopy in order to examine the organ cavity and see the tumor with the eye.
If endometriosis has been identified, the doctor may prescribe magnetic resonance imaging in order to clarify the location of ectopic foci. In addition, if endometriosis is detected, the doctor may prescribe a blood test for the content of follicle-stimulating, luteinizing hormones, and testosterone in order to clarify the causes of the disease.
If cysts, tumors or inflammation have been identified in the ovaries, additional examinations are not carried out, as they are not needed. The only thing the doctor can prescribe in this case is laparoscopic surgery (make an appointment) for removal of tumors and conservative treatment for the inflammatory process.
In the case when, according to the results Ultrasound (sign up), gynecological examination and speculum examination did not reveal any pathology of the uterus or ovaries; dysfunctional bleeding is assumed due to a hormonal imbalance in the body. In such a situation, the doctor prescribes the following tests to determine the concentration of hormones that can affect the menstrual cycle and the appearance of uterine bleeding:
- Blood test for cortisol (hydrocortisone) levels;
- Blood test for the level of thyroid-stimulating hormone (TSH, thyrotropin);
- Blood test for triiodothyronine (T3) level;
- Blood test for thyroxine (T4) level;
- Blood test for the presence of antibodies to thyroid peroxidase (AT-TPO);
- Blood test for the presence of antibodies to thyroglobulin (AT-TG);
- Blood test for follicle-stimulating hormone (FSH) levels;
- Blood test for luteinizing hormone (LH) levels;
- Blood test for prolactin level (sign up);
- Blood test for estradiol levels;
- Blood test for dehydroepiandrosterone sulfate (DEA-S04);
- Blood test for testosterone levels;
- Blood test for sex hormone binding globulin (SHBG) levels;
- Blood test for the level of 17-OH progesterone (17-OP) (sign up).
Treatment of uterine bleeding
Treatment of uterine bleeding is aimed primarily at stopping bleeding, replenishing blood loss, as well as eliminating the cause and preventing it. All bleeding is treated in a hospital setting, because first of all it is necessary to carry out diagnostic measures to find out their cause.Methods to stop bleeding depend on age, its cause, and the severity of the condition. One of the main methods surgical stop bleeding is a separate diagnostic curettage - it also helps to identify the cause this symptom. To do this, a scraping of the endometrium (mucous membrane) is sent for histological examination. Curettage is not performed for juvenile bleeding (only if heavy bleeding does not stop under the influence of hormones, and threatens life). Another way to stop bleeding is hormonal hemostasis (use of large doses of hormones - estrogen or combined oral contraceptives Mirena). When revealed inside uterine pathology– carry out treatment chronic endometritis, endometrial polyps, uterine fibroids, adenomyosis, endometrial hyperplasia.
Hemostatic agents used for uterine
bleeding
Hemostatic agents are used for uterine bleeding as part of symptomatic treatment. Most often prescribed:
- dicinone;
- ethamsylate;
- vikasol;
- calcium preparations;
- aminocaproic acid.
Dicinone for uterine bleeding
 Dicynone (etamsylate) is one of the most common drugs used for uterine bleeding. Belongs to the group of hemostatic (hemostatic) drugs. Dicynone acts directly on the walls of capillaries (the most small vessels), reduces their permeability and fragility, improves microcirculation (blood flow in capillaries), and also improves blood clotting in areas of damage to small vessels. However, it does not cause hypercoagulation (increased blood clot formation) and does not constrict blood vessels.
Dicynone (etamsylate) is one of the most common drugs used for uterine bleeding. Belongs to the group of hemostatic (hemostatic) drugs. Dicynone acts directly on the walls of capillaries (the most small vessels), reduces their permeability and fragility, improves microcirculation (blood flow in capillaries), and also improves blood clotting in areas of damage to small vessels. However, it does not cause hypercoagulation (increased blood clot formation) and does not constrict blood vessels. The drug begins to act within 5-15 minutes after intravenous administration. Its effect lasts 4-6 hours.
Dicinone is contraindicated in the following cases:
- thrombosis and thromboembolism;
- malignant blood diseases;
- hypersensitivity to the drug.
What to do with prolonged uterine bleeding?
With prolonged uterine bleeding, it is important to seek medical help as soon as possible. If signs of severe anemia appear, it is necessary to call an ambulance to stop the bleeding and further observation in the hospital.Main signs of anemia:
- severe weakness;
- dizziness;
- decreased blood pressure;
- increased heart rate;
- pale skin;
Folk remedies
 As folk remedies for the treatment of uterine bleeding, decoctions and extracts of yarrow, water pepper, shepherd's purse, nettle, raspberry leaves, burnet and other medicinal plants are used. Here are some simple recipes:
As folk remedies for the treatment of uterine bleeding, decoctions and extracts of yarrow, water pepper, shepherd's purse, nettle, raspberry leaves, burnet and other medicinal plants are used. Here are some simple recipes: 1. Infusion of yarrow herb: 2 teaspoons of dry herb are poured with a glass of boiling water, left for 1 hour and filtered. Take 4 times a day, 1/4 cup of infusion before meals.
2. Infusion of shepherd's purse herb: 1 tablespoon of dry herb is poured with a glass of boiling water, left for 1 hour, pre-wrapped, then filtered. Take 1 tablespoon, 3-4 times a day before meals.
3.
Acute pathological uterine bleeding is a common problem faced by practicing gynecologists. Even one-time similar cases sometimes require immediate medical intervention. The causes of this pathology are numerous. To solve the problem and understand how to stop uterine bleeding, it is necessary to take into account the woman’s age, her menstrual function and medical history, risk factors for endometrial pathology and blood coagulation system.
Etiology of acute abnormal uterine bleeding
The etiology of uterine bleeding can be multifactorial. This pathology is classified as associated with structural abnormalities of the uterus and disorders of the blood coagulation system. This happens for reasons:
- polyp;
- hyperplasia;
- adenomyosis;
- leiomyomas;
- cancer processes of the body and cervix;
- coagulopathies;
- ovulatory dysfunction;
- endometriosis;
- pregnancy;
- iatrogenic factors.
Determining the most likely etiology has important in choosing the most suitable and effective way stopping bleeding for a specific patient and is achieved by collecting anamnesis, physical and gynecological examination and blood tests.
Clinical evaluation of hemostatic disorders in a woman with excessive menstrual bleeding
Initial screening for an underlying hemostatic disorder in these women should be based on their medical history. Positive result The study includes the following circumstances:
- heavy menstrual bleeding starting at menarche;
- postpartum hemorrhage;
- operations accompanied by blood loss;
- disruption of the coagulation system during dental treatment.
In this case, the following conditions must be taken into account:
- hematomas once or twice a month;
- frequent nosebleeds;
- constant bleeding from the gums;
- symptoms of coagulopathy in close relatives.
History or anamnesis
Obtaining a thorough medical history is necessary to determine the circumstances surrounding the occurrence of bleeding. This takes into account accompanying symptoms and past causes of menstrual irregularities, details of gynecological and medical history and data from relevant laboratory and radiological tests.

Up to 13% of women with heavy menstrual bleeding have variant von Willebrand disease, and up to 20% of patients may have bleeding disorders. Other causes of coagulopathies, such as decreased coagulation factors, hemophilia, and platelet dysfunction, may occur in any age group. In addition, systemic diseases such as leukemia and liver failure, as well as medications such as anticoagulants or chemotherapy agents, may reduce clotting and cause bleeding. All this is taken into account in developing tactics for solving the upcoming issue: how to stop uterine bleeding.
Physical examination
The physical examination of a patient with uterine bleeding should begin with an assessment acute blood loss and the main symptoms, which are hypovolemia, anemia, and results that suggest the etiology of the disease. The woman's condition should be assessed so that the doctor can determine that she is having uterine bleeding and not bleeding from other areas of the genital tract. Therefore, a gynecological examination, including speculum examination of the cervix and bimanual palpation, should be performed by a gynecologist to identify any injuries to the genitals, vagina or cervix. All this allows us to draw conclusions about what caused the vaginal bleeding. A gynecological examination will also determine the volume, intensity of bleeding, the condition of the uterus, internal genital organs or structural lesions reproductive organ(leiomyoma).
Laboratory research
Laboratory evaluation of patients with this disease is necessary. All adolescents and women are carefully examined for the presence of hemostatic disorders. Taking into account the clinical picture, it is necessary to take into account the pathology thyroid gland, liver function disorders, sepsis, leukemia, etc. Endometrial tissue sampling should be performed in all women. This is especially true for patients over 45 years of age. Endometrial biopsy should also be performed in women younger than 45 years of age with a history of exposure to unconjugated estrogens (eg, seen in patients with obesity or polycystic ovary syndrome), a primary bleeding episode, or persistent similar manifestations. The decision as to whether a pelvic ultrasound should be performed should be based on clinical assessment data.

Initial laboratory testing requires:
- determination of group and Rh factor;
- pregnancy test;
- registration of activated partial thromboplastin time;
- prothrombin time;
- determining the amount of fibrinogen;
- initial testing for von Willebrand disease;
- determining the level of thyroid-stimulating hormone;
- identifying serum iron, total iron-binding capacity and ferritin;
- liver function tests;
- detection of chlamydia trachomatis.
Stopping acute abnormal uterine bleeding in non-pregnant women of reproductive age
The initial assessment of a patient with acute abnormal uterine bleeding should include testing for signs of hypovolemia and potential hemodynamic instability. Measures to stop bleeding include: intravenous administration conjugated estrogens, the prescription of combined oral contraceptives, oral progestins and tranexamic acid. Decisions should be based on the patient's medical history and the presence of contraindications to therapy. Surgery should be considered for those women who are not clinically stable. The choice of surgical intervention should be based on the patient’s presence of concomitant diseases underlying the pathology and the woman’s desire to have children in the future. Once the acute bleeding episode has resolved, transition to long-term maintenance therapy is recommended.

Uterine bleeding is defined as bleeding from the body of the uterus when it is abnormal in regularity, volume, frequency or duration and occurs in the absence of pregnancy. This pathology can be acute or chronic. Acute bleeding is a situation that requires immediate intervention to prevent further blood loss. The acute process can occur spontaneously or in conditions of chronic hemorrhage or bleeding. Overall rating a patient who has this pathology, must take place in three stages:
- determination of the amount of blood loss;
- determining the most likely etiology;
- choosing the appropriate treatment.
Treatment
Limited evidence, expert opinion and guidelines address the question of how to quickly stop uterine bleeding. The choice of treatment method depends on the clinic and etiology, taking into account the underlying medical problems. The two main goals of management are control of bleeding and monitoring to reduce menstrual blood loss in subsequent cycles. Drug therapy is considered the preferred primary treatment option. However, certain situations may require surgical intervention.
Basic drugs
How to stop uterine bleeding? The drugs that are used for this purpose are hormonal agents. They are considered the first line drug therapy for patients with acute bleeding. Treatment options include combination oral contraceptives and oral progestins.
Antifibrinolytic drugs, such as tranexamic acid, are used to prevent fibrin degradation and are effective in treating patients with any form of bleeding. Tranexamic acid effectively reduces the rate of intraoperative blood loss and removes indications for blood transfusion in surgical patients.

Patients with bleeding disorders or those suspected of having excessive bleeding may develop unpredictable reactions to hormonal and non-hormonal methods treatment. For such patients, consultation with a hematologist is recommended, especially if the bleeding is quite difficult to control or the gynecologist cannot independently cope with this pathology. Desmopressin may help treat patients with von Willebrand disease if the woman is known to respond to the drug. It can be administered by intranasal inhalation, intravenously, or subcutaneously. This medication should be used with caution due to the risk of fluid retention and hyponatremia. It should not be given to patients with massive bleeding receiving intravenous resuscitation. Recombinant factor VIII and von Willebrand factor are also available and may be necessary to control major bleeding. Other deficiency factors may require factor-specific replacements.
Patients with bleeding disorders or platelet function disorders should avoid nonsteroidal anti-inflammatory drugs due to their effects on platelet aggregation and their interactions with substances that may affect liver function and the production of clotting factors.
Surgery
How to stop uterine bleeding with endometrial hyperplasia or fibroids? Necessity surgical treatment based on the patient’s clinical stability, severity of bleeding, presence of contraindications for therapeutic treatment, lack of response to medical supplies And concomitant pathology. Surgical options include endometrial dilation and curettage, endometrial ablation, uterine artery embolization, and hysterectomy. The choice of surgical intervention method is made based on the above factors plus the patient’s desire to preserve fertility in the future.

Specific procedures, such as hysteroscopy, polypectomy, myomectomy, may be required if structural abnormalities are suspected as the cause of the identified pathology. And therefore, the question of how to stop uterine bleeding with fibroids or polyposis is being resolved in favor of surgical methods. Dilation and curettage alone (without hysteroscopy) is an inadequate means of assessing uterine distress and may provide only a temporary reduction in bleeding. If they are performed with concomitant hysteroscopy, then this may be important for those patients in whom intrauterine pathology is suspected, or it is desirable to obtain a tissue sample to identify certain processes. Case reports of uterine artery embolization and endometrial ablation have shown that these procedures are successful in treating bleeding. Endometrial ablation, although readily available in most centers, should only be considered if other treatments have failed or are contraindicated. This procedure should only be performed when the woman has no plans for future childbearing and uterine cancer has been reliably excluded as a cause. Hysterectomy is used as final method treatment to combat heavy bleeding, which may be necessary for patients who do not respond to drug therapy.
Thus, it was listed in what ways and how uterine bleeding is stopped in the hospital.
Special cases
In most cases, a woman does not know why she has bleeding and does not suspect that she has certain predisposing factors for the development of this uterine pathology. But sometimes there are diseases that the patient knows about, and it is her information, as well as additional methods examinations help in clarifying the diagnosis and choosing specific treatment tactics.
Bleeding during pregnancy
During perimenopause, the most common cause abnormal bleeding is a change in hormonal levels that prevents ovulation. Regular but much heavier periods are very common in the years leading up to menopause. For women over 40 years of age, low doses of birth control pills will help control heavy uterine bleeding. How to stop it and address other perimenopause symptoms, including hot flashes, night sweats, premenstrual syndrome and headaches? The use of tablet contraceptives will help with this when used on an ongoing basis. After 50 years of age, with replacement hormone therapy(which consists of more low doses estrogen and progesterone than in tablets) you can eventually wean the patient off hormones altogether if menopausal symptoms gradually decrease.

During perimenopause, some people choose not to take birth control pills, so they can be used in in this case other conservative methods stop bleeding. The Progesterone IUD is one such option, and it offers an excellent option for birth control that can last for five years. The device releases progesterone hormone, which works in the lining of the uterus, resulting in menstruation without complications. IUD is preferred option for women who need reversible methods of contraception.
How to stop uterine bleeding surgically? Endometrial ablation is a minimally invasive procedure that has a proven track record of treating heavy perimenopausal bleeding and may even help some patients avoid a hysterectomy. Ablation procedures have been used quite successfully to reduce the amount of bleeding, in some cases leading to a complete stop of the menstrual cycle. This procedure is not a birth control method and is only used for women who have completed childbearing.
For patients who have not responded to medications and less invasive options, this perimenopausal surgery may be the best option to decide how to stop uterine bleeding. For endometriosis, fibroids, hyperplasias, polyps, hysterectomy is the most preferred method for women with such changes. In this case, amputation of the uterus is possible using various options. The doctor should know the concomitant diseases of such a woman.
How to stop uterine bleeding at home
Bleeding in any case requires contacting a doctor to determine the cause and prescribe adequate treatment. Before the ambulance arrives, you must take horizontal position and raise your legs. You can place a heating pad with ice on your lower abdomen. Compresses and warming procedures are strictly contraindicated. How to stop uterine bleeding at home, what decoctions and preparations can be used? This is well known to older women. “Vikasol”, “Ditsinon”, “Oxytocin”, “Tranexamic acid” - these are the drugs that every woman should have in her first aid kit. These medicines help in deciding how to stop uterine bleeding at home.
Folk remedies
Recipes traditional medicine are used in the treatment of many diseases. How to stop uterine bleeding with folk remedies? This question interests both young girls and older women. Most often in this case, a decoction of nettle leaves, yarrow, shepherd's purse, and tincture of water pepper is used. Decoctions are also prepared from cucumber vines, jasmine, and peppermint. However, such treatment can only be used as helper method and only after consulting a doctor.
Monthly uterine bleeding - normal phenomenon for women of reproductive age. However, vaginal bleeding can also be pathological.
Heavy bleeding during menstruation indicates the development of pathological processes in the female body. In such situations, it is important to know how to stop bleeding at home.
Heavy bleeding during menstruation can be easily distinguished from normal menstrual flow. In the pathological process, bleeding is prolonged and is accompanied by the following symptoms:
- heavy discharge does not stop for a week;
- necessity frequent changes hygiene products – up to 8-10 times a day;
- presence of blood clots;
- severe pain in the lower abdomen, which is nagging in nature;
- headache and dizziness.
Blood loss during menstruation healthy woman on average is 60 ml for the entire menstrual cycle. The first days of discharge are accompanied by mild aching pain in the lower abdomen caused by contractions of the uterus. Heavy menstrual bleeding is defined as bleeding from the uterus of more than 80 ml per cycle.
Causes of severe bleeding
Heavy menstrual bleeding may have the following causes:
- abortions and medical termination of pregnancy;
- inflammatory processes of the pelvic organs;
- tumors and neoplasms in the uterus and ovaries;
- infectious diseases;
- endometriosis;
- use of intrauterine contraceptives;
- thyroid diseases.
Such processes causing disturbance menstrual cycle and quantity uterine discharge, require compulsory treatment. However, it is important to know how to stop heavy periods at home in order to provide first aid before contacting a specialist.
As soon as a woman realizes that she has severe uterine bleeding, and there is a deterioration in her condition, she should call an ambulance. Before arrival medical workers You can try to reduce the intensity of uterine bleeding on your own.

- It is necessary to take a horizontal position so that your legs are higher in relation to your body. To do this, you can put a pillow under them.
- Apply a cold object to the lower abdomen for 15 minutes. An ice pack will do. Cold constricts blood vessels and can reduce blood loss.
- You need to drink plenty of fluids to replenish water balance. You can drink water, juices, sweet tea.
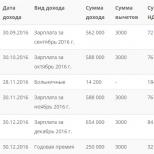
This table presents the main hemostatic drugs used for severe uterine bleeding.
| Drug name | Pharmacological properties | Mode of application |
| Calcium glucanate | Available in the form of an injection solution and tablets, it increases blood clotting | The woman is administered intravenously from 5 to 15 ml of calcium glucanate, after which tablets are prescribed - up to 6 pieces per day after meals. |
| Askorutin | Has a strengthening effect on the walls of blood vessels, reduces capillary fragility | Take up to 2 tablets several times a day |
| Oxytocin | Has a contractile effect on the uterus, increases the excitability of muscle fibers | It is administered into a woman’s body intravenously or intramuscularly. With the intravenous method of administering oxytocin, the effect of the drug occurs instantly |
| Aminocaproic acid | Removes increased activity blood | Can only be used in a hospital setting, available in the form of powder and sterile 5% solution. Powders are prescribed 2-3 g up to 5 times a day, 100 ml of solution is administered intravenously every 4 hours |
| Vikasol | Normalizes blood clotting processes. This synthetic drug is designed as a replacement for vitamin K. | Available in the form of ampoules of 1 ml solution and tablets. Tablets are taken 4 pieces per day, solution - up to 2 ampoules. The effect occurs 12-14 hours after administration of the drug |

All these medications may only be used under specialist supervision.
It is important to know how to stop bleeding during menstruation at home. In gynecology, two drugs are widely used for these purposes - Dicynon and Tranexam.
Action and use of Dicynon
Dicinone activates blood clotting and has a vasoconstrictor effect. Therapeutic effect occurs approximately 3 hours after administration of the drug into the body. When administered intravenously, the effect occurs after 20 minutes.
At severe blood loss a single dose can consist of 3 tablets, or can be prescribed for a course of up to 10 days. In gynecology, Dicinon is also used for prophylaxis against a tendency to uterine bleeding.

There may be such side effects Dicinona:
- nausea;
- heartburn;
- dizziness;
- general weakness and malaise;
- hypotension;
- allergic reactions - itching and rashes on the skin.
Dicinon is not suitable for all women for menstrual bleeding. The drug has the following contraindications:
- glucose-lactose deficiency;
- blood diseases;
- liver and kidney diseases;
- increased blood clotting.
Tranexam for bleeding
Tranexam has hemostatic, anti-inflammatory, antitumor effects. The duration of taking the drug should not exceed 4 days. Daily dose – 6 tablets in 2-3 doses. Tranexam is administered intravenously every 8 hours.

Tranexam has the following contraindications:
- thrombosis;
- color vision impairment;
- individual intolerance;
- kidney diseases.
When using Tranexam, the following side effects are possible:
- vomiting, dizziness, nausea;
- weakness, drowsiness;
- tachycardia;
- chest pain;
- allergy.
In addition to Dicinon and Tranexam, you can reduce menstrual flow using such means as:
- Lagochilus tincture – dissolve in water 1:5, take 3 times a day;
- water pepper tincture - take 3 times a day, 30 drops.

IN home medicine cabinet Every woman should have at least one of the drugs that have a hemostatic effect.
It is also possible that menstruation ends, but bleeding soon begins after menstruation. A specialist will tell you how to stop blood loss after full examination patients. Bleeding that begins after menstruation and is not associated with it is referred to in gynecology as “metrorrhagia.”
This pathology may have the following reasons:
- ectopic pregnancy;
- miscarriage;
- hormonal disorders;
- chronic infections pelvic organs;
- rupture of a cyst or ovary;
- presence of erosion, polyps;
- taking oral contraceptives.

The exact cause of pathological bleeding from the vagina, a specialist will be able to determine it after an examination. Before contacting a specialist, a woman can take hemostatic drugs or traditional medicine.
Folk remedies for severe bleeding
Traditional medicine will also help stop bleeding.
Heavy bleeding during menstruation can be stopped using the following means:
- Lemon. At heavy menstruation can you eat lemon in pure form or with sugar. You need to eat two lemons a day.
- Water pepper. This remedy increases blood clotting, relieves pain and has a wound healing effect. To prepare the medicine, 2 tbsp. l. dry herbs pour 400 ml of boiling water. Infuse water pepper for half an hour and take 1 tbsp. l. every two hours.
- Cuff. The plant has an effect on female body astringent, wound-healing, hemostatic and analgesic effect, widely used in pharmacology. To prepare tea, pour 30 g of dry herb into 1/2 liter of boiling water. Infuse the drink for an hour and take it three times a day until the unpleasant symptoms disappear.
- Shepherd's Purse. This medicinal plant has a hemostatic effect on the body. You can use baths prepared from the plant or drink it as tea. To prepare medicinal tea, pour 20 g of herb into two glasses of boiling water, leave for an hour, divide into 3 doses and take before meals. To prepare a sitz bath for 1 liter of boiling water you will need 2 tbsp. plants. The duration of the procedure is 15 minutes, the course is 5 days.
- Nettle. The plant is good remedy to maintain uterine tone. 1 tbsp. l. Nettle leaves pour ½ liter of water, strain after 20 minutes, and take 100 ml at a time.
- Cinnamon. The spice will help reduce the intensity of bleeding during heavy menstruation. In a glass of warm water, stir 3 tbsp. l. ground cinnamon. This remedy should be taken every half hour until the heavy bleeding stops.
If heavy menstrual bleeding occurs, measures should be taken to reduce blood loss. To determine the cause of the pathology, you should seek help from a specialist.
If it is not normal menstruation, are always a bad sign and become a reason for an immediate visit to the gynecologist. As for the causes of bleeding in women, they are very different, associated with both age-related changes in the body, and with a number of pathologies and diseases of the female genital area.
It should be noted that experts distinguish between genital and uterine bleeding, since the nature of their origin is different in most cases. Thus, vaginal bleeding is usually caused by mechanical damage or some kind of infectious disease. Sexual bleeding occurs for various reasons and varies in intensity.
The cause of bleeding from the uterus may be ovulation, some gynecological diseases and diseases circulatory system. But most often such bleeding occurs due to hormonal imbalance. This can happen at any time age period, in connection with which uterine bleeding is usually classified according to the woman’s age:
- Puberty and juvenile periods (12-18 years).
- Reproductive age (18-45 years).
- Menopause (45-55 years).
Bleeding can be suspected by pathologically heavy periods, increased duration of menstruation, acyclicity of menstruation (menstruation does not occur for 6-8 weeks, and then heavy bleeding occurs).
Let's take a closer look at the causes of bleeding in women.
Common reasons
Most probable cause bleeding from the uterus young girls and women menopausal age there is a failure in general hormonal background. In a normal state, when the hormones estrogen and progesterone are produced in optimal quantities, menstrual blood loss does not exceed the permissible volume. When this balance is disturbed, pathological dysfunctional bleeding from the uterus occurs.
Thyroid diseases (hypothyroidism, hyperthyroidism) increase the risk of bleeding. In addition, pathological blood loss can be caused by diseases of the circulatory system, leading to a decrease in the number of platelets in the blood.
As a rule, the following causes of bleeding in women are considered:
- Fibroids (with internal uterine fibroids, blood loss is very intense).
- Adenomyosis (characterized by long, very heavy, excruciatingly painful menstruation).
- Polyps ( benign neoplasms leading to heavy periods with severe pain and uterine bleeding).
- Ectopic pregnancy.
- Placental abruption, threatened miscarriage, other pregnancy complications.
- Malignant tumors. This is the most dangerous reason bleeding in women, regardless of the location of the tumor (ovaries, uterus, cervix, etc.). Requires immediate medical intervention.
In recent years, women of reproductive age have increasingly observed the phenomenon of breakthrough bleeding from the uterus. The reason is their use intrauterine devices, other types of contraceptives, taking hormonal contraceptives. Moreover, the risk of uterine bleeding increases with simultaneous administration contraception and anticoagulants.
At certain periods of a woman’s life, bleeding can occur for various reasons. Therefore, they need to be considered separately.
Yes, the bulk gynecological pathologies in girls and women aged 12-18 years is associated with a violation of the process of hormone regulation. The provoking factors for this condition are very different:
- Physical and mental injuries.
- Poor nutrition.
- Thyroid dysfunction, pathology of the adrenal cortex.
- Children's infectious diseases(flu, mumps, measles, chickenpox, chronic tonsillitis and etc.).
- Complicated pregnancy and difficult birth for the mother.
- Tuberculosis of the genital organs.
- Blood clotting disorders.
IN childbearing age Uterine bleeding in women is mainly associated with dysfunction of the ovaries. The cause of ovarian dysfunction may be:
- General overwork of the body, stress, constant neuropsychic tension.
- Unfavorable living conditions (regions with developed metallurgical, mining, chemical industries).
- Occupational hazard.
- Climate change.
- Various infectious and inflammatory diseases female genital area.
- Uterine fibroids.
- Ovarian tumors.
- Malignant and benign neoplasms on the cervix and in the uterus itself.
- Ectopic pregnancy.
- Miscarriage.
- Medication or surgical abortion, scraping.
- Taking medications that lead to dysfunction of the pituitary gland and hypothalamus.
As a percentage of others gynecological diseases Uterine bleeding is the most common pathology in women of premenopausal and menopausal age.
 This is due to the decline of the functions of the pituitary gland. There is a gradual decrease in the production of gonadotropins by the pituitary gland, the release of hormones, accordingly, becomes irregular, as a result of which the cyclicity of ovulation is disrupted, folliculogenesis develops, and the corpus luteum increases.
This is due to the decline of the functions of the pituitary gland. There is a gradual decrease in the production of gonadotropins by the pituitary gland, the release of hormones, accordingly, becomes irregular, as a result of which the cyclicity of ovulation is disrupted, folliculogenesis develops, and the corpus luteum increases.
Uterine bleeding is especially common when climacteric syndrome when the symptoms of menopause in women are most intense. This is explained by the fact that during this period the deficiency of the hormone progesterone is especially acute, resulting in the growth of the endometrium and hyperestrogenism.
At the slightest suspicion of bleeding during menstruation, in the middle of the cycle, during pregnancy, or during menopause, a woman must immediately consult a gynecologist.
Only timely detection of any pathology, accurate identification of their causes and adequate treatment will help to avoid serious problems with health.
Popular articles
Success of a specific plastic surgery largely depends on how...
Lasers in cosmetology are used quite widely for hair removal, so...
The danger of uterine bleeding is great; it quickly intensifies and may not stop for a long time. The family gets into difficult situation, if you are far from the city, in the country, and the question of how to stop uterine bleeding at home needs to be resolved here and now.
It’s good if there are elderly women in the village who have knowledge of herbal medicine, they can help brew necessary herbs, which are usually collected in the summer and stored in the house, in the right conditions drying so that the herbs retain all their healing power.
Often dried herbs work better than freshly picked ones, but when you have no choice, any plants suitable for hemostatic action are used, because it is urgent to stop the bleeding before it leads to serious complications.
The consequences of uterine bleeding are severe:
- Anemia develops if more than 80 ml of blood is lost. There is no threat to health yet, but the situation cannot be left without attention;
- when a lot of blood is lost and the bleeding becomes severe, it is difficult to stop it, it is required surgery, followed by a blood transfusion to replenish lost volume to normal;
- if the bleeding is severe, the underlying disease may worsen. If a woman is unable to see a doctor, even a small loss of blood causes profuse bleeding, and the disease becomes chronic;
- bleeding in pregnant women is dangerous, it can cause premature birth; Bleeding in women in the postpartum stage is dangerous - in both cases it often leads to shock. Its severity is due to the inability to fully reduce and independently stop blood loss.
The first and main aid is to urgently call an ambulance. In the meantime, doctors are traveling to a distant village, we urgently need to find out from older women how to stop uterine bleeding at home traditional methods, and use village medicine recipes.
Uterine bleeding of any cause seriously threatens a woman’s health, so the treatment that is available according to the situation must be prompt.
 Regardless of the reasons for the bleeding, the woman should be placed on her back, on a hard bed, with her legs raised so that they are on some kind of elevation - pillows, bolsters made of blankets.
Regardless of the reasons for the bleeding, the woman should be placed on her back, on a hard bed, with her legs raised so that they are on some kind of elevation - pillows, bolsters made of blankets.
In this position, a person’s consciousness is preserved, especially when the blood loss is large. You need to put something cold on your stomach.
Frozen water in plastic bottle, just frozen food works well. They need to be wrapped in a towel, kept on their stomach for 15 minutes, then take a 5-minute break. Cold causes blood vessels to constrict and blood flows significantly less.
A woman should be given plenty of water, weakly brewed sweet black or green tea. This will become an analogue of a hospital IV. You can drink plain water, herbal decoctions and tinctures. This will replenish fluid loss, and the glucose from their sugar will nourish nerve cells brain. Usually a woman knows what to do in such situations, she knows the cause of the bleeding, and most often in her travel first aid kit or cosmetic bag she will find necessary pills. But they should be taken only as prescribed by the doctor if the woman has regular bleeding.
After 50 years, women know how to stop uterine bleeding at home during menopause. For this, medications prescribed by a doctor and herbal decoctions are used. However, you need to drink medicine and herbal tea together with great caution: herbs sometimes have greater healing power than medications, and in order not to enhance the effects of the pills, you need to take one thing.
During menopause, a woman should know the symptoms of bleeding, the properties of discharge, and be able to dose the same Vikasol.
Many women drink Ascorbic acid, if the gastrointestinal tract allows, calcium gluconate. But medications must be prescribed by a doctor in suitable dosages.
Bleeding during menopause indicates:
- about a malfunction in the production and functions of hormones;
- about the growth of fibroids;
- about endocrine disorders;
- about ovarian tumors;
- about the presence of polyps;
- about other serious diseases.
 Therefore, women of Balzac age are usually savvy in matters of their gynecological health, and know how to stop uterine bleeding at home with endometriosis, if they have such a chronic disease.
Therefore, women of Balzac age are usually savvy in matters of their gynecological health, and know how to stop uterine bleeding at home with endometriosis, if they have such a chronic disease.
What grows everywhere in the village and is constantly trampled underfoot is valuable medicinal plant. These are Knotweed, Shepherd's purse, Yarrow, Nettle.
Plants known to everyone, in their own way medicinal effects constituting the “female” group of herbs. Wash the top leaves of the plants well, not a lot, 2-3 at a time will be enough, take the white inflorescences from the Shepherd's Purse and pour boiling water in a half-liter jar. After half an hour the medicine is ready. This is a complex herbal tea that you should drink if you don’t have medicine at hand.
Yarrow and Knotweed relieve inflammation, Nettle and Shepherd's Purse stop bleeding. With this tea, which a woman will drink 2-3 sips every hour, you can calmly wait for the ambulance to arrive, or drive to the nearest hospital in your car, lying in the back seat. And behind the wheel is a caring husband.
 When a woman is registered with a gynecologist for uterine fibroids, she also knows how to stop uterine bleeding at home with fibroids. Among the herbs for making tea using the same recipe, you can take Water Pepper, Cat's Paws, Knotweed, Nettle. Their hemostatic properties will help you wait medical care, without which, in principle, it is unlikely that at least one uterine bleeding will occur.
When a woman is registered with a gynecologist for uterine fibroids, she also knows how to stop uterine bleeding at home with fibroids. Among the herbs for making tea using the same recipe, you can take Water Pepper, Cat's Paws, Knotweed, Nettle. Their hemostatic properties will help you wait medical care, without which, in principle, it is unlikely that at least one uterine bleeding will occur.
The set of components contained in herbs strengthens the walls of blood vessels, makes the blood more viscous, and as a result, blood loss may decrease slightly. arterial pressure, already reduced, not only due to uterine, but also possibly due to. This point must also be carefully monitored, and the woman must be given warm coffee with milk or a caffeine tablet in a timely manner.
It turns out that a woman should know how to behave if uterine bleeding occurs somewhere far from home, on a trip, in nature, in the countryside. And how to stop uterine bleeding at home, there are reviews on many resources where women share their own sad experience, and where you can find unexpected interesting recipes from grandma's old notebooks.