Respiratory tract infection. ARVI - causes, symptoms and treatment in adults, prevention of acute respiratory viral infections. Acute inflammation of the trachea
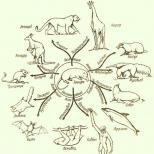
Diseases respiratory tract more common during the cold season. More often they affect people with weakened immune systems, children and elderly pensioners. These diseases are divided into two groups: diseases of the upper respiratory tract and lower. This classification depends on the location of the infection.
According to their shape, they distinguish between sharp and chronic diseases respiratory tract. The chronic form of the disease occurs with periodic exacerbations and periods of calm (remission). The symptoms of a particular pathology during periods of exacerbation are absolutely identical to those observed in the acute form of the same respiratory tract disease.
These pathologies can be infectious and allergic.
They are more often caused by pathological microorganisms, such as bacteria (ARI) or viruses (ARVI). As a rule, these diseases are transmitted by airborne droplets from sick people. The upper respiratory tract includes nasal cavity, pharynx and larynx. Infections that reach these sections respiratory system, cause diseases of the upper respiratory tract:
- Rhinitis.
- Sinusitis.
- Sore throat.
- Laryngitis.
- Adenoiditis.
- Pharyngitis.
- Tonsillitis.
All these ailments are diagnosed all year round, but in our country the increase in incidence occurs in mid-April and September. Such respiratory diseases are the most common in children.
Rhinitis
This disease is characterized by an inflammatory process of the nasal mucosa. Rhinitis occurs in acute or chronic form. Most often it is caused by an infection, viral or bacterial, but various allergens can also be the cause. Anyway characteristic symptom is swelling of the nasal mucosa and difficulty breathing.
For initial stage Rhinitis is characterized by dryness and itching in the nasal cavity and general malaise. The patient sneezes, the sense of smell is impaired, and sometimes rises low-grade fever. This condition can last from several hours to two days. Next comes clear nasal discharge, liquid and large quantities, then these discharges become mucopurulent in nature and gradually disappear. The patient feels better. Breathing through the nose is restored.

Rhinitis often does not manifest itself as an independent disease, but acts as an accompaniment to other infectious diseases, such as influenza, diphtheria, gonorrhea, scarlet fever. Depending on the cause of this respiratory tract disease, treatment is aimed at eliminating it.
Sinusitis
It often manifests itself as a complication of other infections (measles, rhinitis, influenza, scarlet fever), but can also act as an independent disease. There are acute and chronic forms of sinusitis. In the acute form, there is a catarrhal and purulent course, and in the chronic form - edematous-polyposis, purulent or mixed.
Characteristic symptoms for both acute and chronic forms of sinusitis are frequent headaches, general malaise, and hyperthermia (increased body temperature). As for nasal discharge, it is profuse and mucous in nature. They can be observed only on one side, this happens most often. This is due to the fact that only some of the paranasal sinuses become inflamed. And this, in turn, may indicate one or another disease, for example:
- Aerosinusitis.
- Sinusitis.
- Ethmoiditis.
- Sphenoiditis.
- Frontit.
Thus, sinusitis often does not manifest itself as an independent disease, but serves as an indicative symptom of another pathology. In this case, it is necessary to treat the root cause, i.e. those infectious diseases respiratory tract, which provoked the development of sinusitis.
If nasal discharge occurs on both sides, this pathology is called pansinusitis. Depending on the cause of this upper respiratory tract disease, treatment will be aimed at eliminating it. Antibacterial therapy is most often used.
If sinusitis is caused chronic sinusitis, during the transition of the acute phase of the disease to the chronic phase, punctures are often used to quickly eliminate undesirable consequences, followed by washing with the drug "Furacilin" or saline solution maxillary sinus. This method of treatment in a short period relieves the patient of the symptoms that torment him (severe headache, swelling of the face, increased body temperature).
Adenoids
This pathology appears due to hyperplasia of the tissue of the nasopharyngeal tonsil. This is a formation included in the lymphadenoid pharyngeal ring. This tonsil is located in the nasopharyngeal vault. As a rule, the inflammatory process of the adenoids (adenoiditis) occurs only in childhood (from 3 to 10 years). The symptoms of this pathology are:
- Difficulty breathing.
- Mucous discharge from the nose.
- During sleep, the child breathes through the mouth.
- Sleep may be disrupted.
- Nasality appears.
- Possible hearing impairment.
- In advanced cases, a so-called adenoid facial expression appears (smoothness of the nasolabial folds).
- Laryngospasms appear.
- Twitching of individual facial muscles may be observed.
- Deformation chest and the skull in the front part appears in particularly advanced cases.
All these symptoms are accompanied by shortness of breath, cough and, if severe course- development of anemia.
To treat this respiratory disease, in severe cases, surgical treatment is used - removal of the adenoids. In the initial stages, rinsing with disinfectant solutions and decoctions or infusions of medicinal herbs is used. For example, you can use the following fee:

All ingredients of the collection are taken in equal parts. If some component is missing, then you can get by with the composition that is available. The prepared collection (15 g) is poured into 250 ml of hot water and boiled over very low heat for 10 minutes, after which it is infused for another 2 hours. The medicine prepared in this way is filtered and used warm to rinse the nose or instill 10-15 drops into each nostril.
Chronic tonsillitis
This pathology occurs as a result of the inflammatory process of the palatine tonsils, which has become chronic. Chronic tonsillitis often affects children; it practically does not occur in old age. This pathology is caused by fungal and bacterial infections. Other infectious diseases of the respiratory tract, such as hypertrophic rhinitis, purulent sinusitis, and adenoiditis, can provoke the development of chronic tonsillitis. Even untreated caries can cause this disease. Depending on the specific cause that provoked this upper respiratory tract disease, treatment should be aimed at eliminating primary focus infections.
In case of development chronic process The following happens in the palatine tonsils:
- Overgrowth of connective tissue.
- Dense plugs form in the gaps.
- Lymphoid tissue softens.
- Cornification of the epithelium may begin.
- Lymphatic drainage from the tonsils becomes difficult.
- Nearby lymph nodes become inflamed.
Chronic tonsillitis can occur in a compensated or decompensated form.

In the treatment of this disease good effect They give physiotherapeutic procedures (UV irradiation), rinses with disinfectant solutions ("Furacilin", "Lugol's", 1-3% iodine, "Iodglycerin", etc.) are applied topically. After rinsing, it is necessary to irrigate the tonsils with disinfectant sprays, for example, the drug "Strepsils Plus" is used. Some experts recommend vacuum suction, after which the tonsils are also treated with similar sprays.
In the case of a pronounced toxic-allergic form of this disease and the absence of a positive effect from conservative treatment, surgical removal of the tonsils is performed.
Angina
The scientific name of this disease is acute tonsillitis. There are 4 types of sore throat:
- Catarrhal.
- Follicular.
- Lakunnaya.
- Phlegmous.
IN pure version These types of sore throat are practically never found. Always present at least symptoms of two types of this disease. So, for example, with lacunae, white-yellow spots are visible at the mouths of some lacunae. purulent formations, and with follicular, festering follicles are visible through the mucous membrane. But in both cases, catarrhal phenomena, redness and enlargement of the tonsils are observed.
With any type of sore throat, body temperature rises and worsens general state, chills appear and an increase in regional lymph nodes is observed.
Regardless of the type of sore throat, rinsing with disinfectant solutions and physiotherapy are used. In the presence of purulent processes, antibacterial therapy is used.
Pharyngitis
This pathology is associated with the inflammatory process of the pharyngeal mucosa. Pharyngitis can develop as an independent disease or a concomitant one, for example, with ARVI. This pathology can be provoked by eating too hot or cold food, as well as inhaling polluted air. Highlight acute course pharyngitis and chronic. The symptoms that are observed with acute pharyngitis are:
- Feeling of dryness in the throat (pharynx area).
- Pain when swallowing.
- Upon examination (pharyngoscopy), signs of inflammation of the palate and its posterior wall are revealed.
The symptoms of pharyngitis are very similar to those of catarrhal tonsillitis, but, unlike it, the patient’s general condition remains normal, and there is no increase in body temperature. With this pathology, as a rule, the inflammatory process does not affect tonsils, and with catarrhal tonsillitis, on the contrary, signs of inflammation are present exclusively on them.
Chronic pharyngitis develops when untreated acute process. Other inflammatory diseases of the respiratory tract, such as rhinitis, sinusitis, as well as smoking and alcohol abuse, can also provoke a chronic course.
Laryngitis
With this disease, the inflammatory process spreads to the larynx. It can affect individual parts of it or capture it completely. Often the cause of this disease is vocal overstrain, severe hypothermia or other independent diseases (measles, whooping cough, influenza, etc.).
Depending on the location of the process in the larynx, individual areas of the lesion may be identified, which become bright red and swell. Sometimes the inflammatory process also affects the trachea, then we're talking about about a disease such as laryngotracheitis.

There is no clear boundary between the upper and lower respiratory tract. The symbolic boundary between them passes at the intersection of the respiratory and digestive systems. Thus, the lower respiratory tract includes the larynx, trachea, bronchi and lungs. Lower respiratory tract diseases are associated with infections of these parts of the respiratory system, namely:
- Tracheitis.
- Bronchitis.
- Pneumonia.
- Alveolitis.
Tracheitis
This is an inflammatory process of the mucous membrane of the trachea (it connects the larynx to the bronchi). Tracheitis can exist as an independent disease or serve as a symptom of influenza or other bacterial disease. The patient is bothered by symptoms general intoxication(headache, fatigue, fever). In addition, there is a raw pain behind the sternum, which intensifies when talking, inhaling cold air and coughing. In the mornings and at night, the patient is bothered by a dry cough. When combined with laryngitis (laryngotracheitis), the patient's voice becomes hoarse. If tracheitis occurs in combination with bronchitis (tracheobronchitis), sputum appears when coughing. If the disease is viral, it will be transparent. In the event of a bacterial infection, the sputum has gray-green color. In this case, antibiotic therapy must be used for treatment.
Bronchitis
This pathology manifests itself as inflammation of the bronchial mucosa. Acute diseases respiratory tract of any location is very often accompanied by bronchitis. Thus, in case of inflammatory processes of the upper respiratory tract, in case of untimely treatment, the infection goes down and bronchitis occurs. This disease is accompanied by a cough. At the initial stage of the process, it is a dry cough with sputum that is difficult to separate. During treatment and the use of mucolytic drugs, the sputum is liquefied and coughed up. If bronchitis is bacterial in nature, antibiotics are used for treatment.
Pneumonia
This is an inflammatory process lung tissue. This disease is mainly caused by pneumococcal infection, but sometimes another pathogen can be the cause. The disease is accompanied high temperature, chills, weakness. Often the patient experiences pain in the affected area when breathing. During auscultation, the doctor can listen for wheezing on the affected side. The diagnosis is confirmed by an x-ray. This disease requires hospitalization. Treatment is carried out using antibacterial therapy.

Alveolitis
This is an inflammatory process of the terminal parts of the respiratory system - the alveoli. As a rule, alveolitis is not an independent disease, but a concomitant one with another pathology. The reason for this may be:
- Candidiasis.
- Aspergillosis.
- Legionellosis.
- Cryptococcosis.
- Q fever.
Symptoms of this disease include a characteristic cough, fever, severe cyanosis, and general weakness. A complication may be fibrosis of the alveoli.
Antibacterial therapy
Antibiotics for respiratory tract diseases are prescribed only in the case of a bacterial infection. If the nature of the pathology is viral, then antibacterial therapy is not used.
Most often, penicillin drugs, such as Amoxicillin, Ampicillin, Amoxiclav, Augmentin, etc., are used to treat diseases of the respiratory system of an infectious nature.
If the chosen drug does not give the desired effect, the doctor prescribes another group of antibiotics, for example, fluoroquinolones. This group includes the drugs Moxifloxacin and Levofloxacin. These drugs successfully cope with bacterial infections, which are resistant to penicillins.
Antibiotics of the cephalosparin group are most often used to treat respiratory diseases. For this purpose, drugs such as "Cefixime" (its other name is "Suprax") or "Cefuroxime Axetil" are used (analogues of this drug are the drugs "Zinnat", "Axetin" and "Cefuroxime").
For treatment atypical pneumonia caused by chlamydia or mycoplasma, macrolide antibiotics are used. These include the drug "Azithromycin" or its analogues - the drugs "Hemomycin" and "Sumamed".
Prevention
Prevention of respiratory tract diseases comes down to the following:
- Try not to be in places with a polluted atmospheric environment (near highways, hazardous industries, etc.).
- Regularly ventilate your home and workplace.
- During the cold season, when there is a surge in respiratory diseases, try not to be in crowded places.
- Good results are achieved by hardening procedures and systematic physical exercise, morning or evening jogging.
- If you feel the first signs of illness, you should not expect everything to go away on its own; you need to seek medical help.

By observing these simple rules prevention of diseases of the respiratory system, you can maintain your health even during seasonal outbreaks of respiratory diseases.
BENEFITS OF INHALATION THERAPY
Inhalation (nebulizer) therapy is one of the main types of treatment for inflammatory diseases of the respiratory tract.
Inhalation has a number of advantages over other methods of drug delivery:
- the possibility of direct and rapid impact on the area of inflammation in the mucous membranes;
- the inhaled substance is practically not absorbed into the blood and has no effect side effects on other organs and systems, as happens when taking pills or injections;
- this is a cheaper way to achieve rapid relief of symptoms and recovery;
- inhalation through a nebulizer is the only possible method of aerosol therapy in children under 5 years of age, as well as in many elderly patients;
- the nebulizer produces an aerosol, 70% of the particles of which have a size of less than 5 microns (up to 0.8 microns);
- Freon is not used in nebulizer therapy;
- there is the possibility of combining medications;
- simultaneous oxygen inhalation is possible.
WHAT DISEASES ARE TREATED WITH INHALATIONS?
- First of all, acute respiratory diseases, accompanied by symptoms such as cough, dryness, sore or sore throat, and sputum production.
Everyone knows that it is quite easy to suppress the temperature by taking paracetamol or aspirin, but the remaining “tail” of the listed catarrhal phenomena will drag on for a long time, causing inconvenience to the patient and his environment. If you use inhalations, then, according to a number of data, recovery will occur 1.5 - 2 times faster. - Another group of diseases for which inhalations are simply irreplaceable are chronic inflammatory processes of the respiratory tract (such as chronic bronchitis, bronchial asthma, chronic pharyngitis, laryngitis). In countries with high level developments in medicine, most patients with asthma and bronchitis have home inhalers and constantly use them. There are medications that allow such patients to relieve an attack of shortness of breath or suffocation without resorting to the services of an ambulance.
TYPES OF INHALERS
Currently in medical practice Three main types of inhalers are used: steam, ultrasonic and compressor (jet). The last two are united by the term “nebulizers” from the Latin word “nebula” - “fog”, “cloud”. They do not generate vapor, but an aerosol cloud consisting of microparticles of the inhaled solution.
Action of steam inhalers based on the evaporation effect medicinal substance. It is clear that only volatile solutions with a boiling point below 100 degrees, most often essential oils, can be used in them. This significantly narrows the spectrum possible components for inhalation. But the biggest drawback of steam inhalers is the low concentration of the inhaled substance. As a rule, it is less than the threshold for therapeutic effect.
Ultrasonic nebulizers spray the solution with ultrasonic vibrations. They are compact, silent and reliable, but a number of drugs (such as antibiotics and sputum thinners) are destroyed in the ultrasonic environment and cannot be used in this type of inhaler.
Compressor nebulizers They form an aerosol cloud by forcing a powerful air stream pumped by a compressor through a narrow hole in a chamber containing a medicinal solution. The size of the particles formed in this case is on average 5 microns, which allows them to penetrate into all parts of the bronchial tree, including the smallest bronchi, and deposit on the mucous membranes, creating high therapeutic concentrations there. All standard solutions for inhalation, produced by pharmaceutical companies in finished form, can be used in compressor (aka jet) nebulizers.
DRUGS USED FOR INHALATION THROUGH NEBULIZERS
- Bronchial dilators(Berotec, salbutamol, Berodual, Atrovent, magnesium sulfate).
- Mucus thinners(lazolvan, fluimucil, physiological sodium chloride solution (0.9%), degassed Borjomi, Narzan, hypertonic solution sodium chloride (3 - 4%).
- Antibacterial agents(fluimucil antibiotic, gentamicin, dioxidin).
- Anti-inflammatory drugs (hormonal drugs- dexamethasone, budesonide, pulmicort and herbal medicines - rotokan).
- Antitussives(lidocaine 2%).
1. Bronchial dilators:
a) b-2 agonists
FENOTEROL
In the form of a ready-made solution trade name Berotek(Boehringer Ingelheim, Austria) in 20 ml bottles at a dose of 1 mg/ml.
Indications for use of Berotek are: bronchial asthma and chronic obstructive bronchitis, especially in the acute stage, as well as acute bronchitis, accompanied by bronchospasm. The dose per inhalation is 1-2 mg Berotek (1-2 ml), peak action - 30 minutes, duration of action - 2-3 hours. The number of inhalations per day depends on the severity of bronchospasm. During an exacerbation, as a rule, the patient inhales the medicine 3-4 times a day, during a period of remission - 1-2 times a day or as needed. For severe asthma attacks, it is recommended frequent inhalations Beroteka - every 20 minutes in the first hour, then at intervals of 1 hour until the condition improves, and then every 4 hours.
In terms of bronchodilating effect, Berotec is approximately 4 times superior to Salbutamol. Advantage of nebulized b-2 agonist before the usual one, dosed in aerosol cans, in that the first creates significantly higher concentrations in the small bronchi, while the main dose of the second settles in the oral cavity and, being absorbed into the blood, causes palpitations, interruptions in heart function, hand tremors and increases arterial pressure.
In addition, for effective action balloon inhaler, you must hold your breath after inhalation for 10 seconds, which is almost impossible during an attack. When using a nebulizer, this is no longer necessary due to the creation of a continuous flow of aerosol with an inhalation duration of 5-7 minutes.
This property of nebulizers is especially important in the treatment of childhood asthma, when it is impossible to force a child to correctly perform the technique of inhaling a metered aerosol.
For children, compressor nebulizers come with masks.
SALBUTAMOL
In the form of a ready-made solution under trade names Steri-Neb Salamol or Gene-salbutamol in ampoules of 2.5 ml.
Indications for the use of liquid Salbutamol are the same as for Berotec. The dose for 1 inhalation is usually 2.5 mg of Salbutamol (1 ampoule), but can vary: from 1/2 ampoule in mild cases to 2 ampoules (5 mg) for severe attacks of shortness of breath (peak action 30-60 minutes, duration of action - 4-6 hours). The number of inhalations per day depends on the severity of the symptoms of the disease.
During an exacerbation, as a rule, the patient inhales the medicine 3-4 times a day, during a period of remission - 1-2 times a day or as needed. In case of severe exacerbations of bronchial asthma, frequent inhalations of Salbutamol are recommended - every 20 minutes in the first hour (up to constant nebulization), then at intervals of 1 hour until the attack resolves against the background basic treatment underlying disease.
b) Combination drugs
FENOTEROL
Fenoterol combined with ipratropium bromide - trade name Berodual(Boehringer Ingelheim, Austria). Available in 20 ml bottles, 1 ml of solution contains 250 mcg of ipratropium bromide and 500 mcg of fenoterol.
Many studies have proven the benefits combination therapy compared with monotherapy with sympathomimetics, especially in individuals with very severe bronchial obstruction suffering from chronic obstructive bronchitis in combination with bronchial asthma. For inhalation, take 2-4 ml of Berodual solution, to which 1-1.5 ml of 0.9% sodium chloride solution is added.
The frequency of use is the same as for Salbutamol.
c) M-anticholinergics
IPRATROPIUM BROMIDE
Ready solution for inhalation, trade name - Atrovent(Boehringer Ingelheim, Austria), in 20 ml bottles, 1 ml of solution contains 250 mcg of ipratropium bromide. A single dose via a nebulizer is 500-1000 mcg, peak action is 60-90 minutes.
The bronchodilator effect lasts up to 5-6 hours. The main indication for prescribing Atrovent is chronic obstructive bronchitis. In terms of bronchodilator effect, it is somewhat inferior to Berotek and Salbutamol, but the main advantage of Atro-Vent therapy is the safety of use. Prescription of Atrovent does not lead to hypoxemia, hypokalemia, practically absent side effects from the outside of cardio-vascular system, which is especially relevant in patients suffering from COPD in combination with heart and vascular diseases.
d) Magnesium sulfate
It is inferior in bronchodilator effect to the above-mentioned drugs, but is more accessible and cheaper. Indications for use are the same as for Salbutamol.
To prepare a solution for inhalation, take 1 ml of a 25% magnesium sulfate solution and add 2 ml to it saline solution.
2. Drugs that thin sputum
LAZOLVAN (Boehringer Ingelheim, Austria)
Solution for inhalation in 100 ml bottles. Is an inhalation analogue Bromhexine. By acting directly on the goblet cells of the bronchial mucosa, it increases their secretion of the liquid component of sputum, as a result of which the viscosity of sputum decreases, making it easier to cough up and remove by cilia epithelial cells. The drug is indicated for any processes in the bronchi when there is viscous, difficult to separate sputum - pneumonia, bronchitis, bronchial asthma, cystic fibrosis. In the first stage of ARVI - when inflammation of the mucous membranes is not yet accompanied by secretion with a feeling of dryness, burning in the trachea and bronchi, dry cough - the use of Lazolvan helps to quickly overcome these symptoms. Dose for inhalation: 2-3 ml of Lazolvan solution 2-4 times a day.
FLUIMUCIL
Active beginning - acetylcysteine. It destroys the polymer bonds in the components of sputum, reducing its viscosity.
Most effective remedy with bronchitis and cystic fibrosis with copious secretion of difficult-to-discharge sputum, including purulent sputum. This drug does not make sense to use for “dry” bronchitis and tracheitis with a meager amount of secretion. The standard dose for inhalation is 3 ml of fluimucil solution (1 ampoule) 2 times a day.
Physiological 0.9% solution sodium chloride or slightly alkaline mineral waters such as "Borjomi", "Narzan".
Good remedies for any colds and mild forms of bronchitis and asthma. They moisturize the mucous membrane along its entire length from the oropharynx to the small bronchi, softening catarrhal symptoms, and increase the liquid part of the bronchial secretion. Take 3 ml of solution for inhalation ( mineral water must be left to degas). Apply 3-4 times a day.
Hypertonic solution NaCl(3 or 4%).
The main indication for use is viscous sputum in the bronchi with the inability to cough effectively. Has a mild disinfectant effect. Can be used when there is a small amount of secretion to obtain sputum for analysis, the so-called “induced sputum”. Use with caution in patients with bronchial asthma, since bronchospasm is often provoked. For inhalation, 4-5 ml of solution is used 1-2 times a day.
3. Antibacterial agents
FLUIMUCIL ANTIBIOTIC
A combined preparation of acetylcysteine and thiamphenicol, an antibiotic wide range action to which the main pathogens of respiratory diseases are sensitive.
Recommended for tonsillitis, pharyngitis, bronchitis of bacterial origin, pneumonia, suppurative lung diseases - abscesses, bronchiectasis, cystic fibrosis. Can be used to prevent postoperative pneumonia in patients with bed rest. For cooking medicinal solution 5 ml of solvent is added to the bottle with dry powder of the drug. For 1 inhalation, take half of the resulting solution. IN medicinal purposes the drug is inhaled 2 times a day, in prophylactic - 1 time a day.
GENTAMICIN 4%
The solution is available in 2 ml injection ampoules. It can also be used for inhalation. It is active against a large group of microorganisms. Particularly effective in exacerbation of chronic purulent bronchitis in weakened patients, smokers, and diabetics. Inhale 2 ml of ready-made Gentamicin solution 2 times a day.
DIOXIDINE 0.5% solution
Broad-spectrum disinfectant. It should be used in patients with purulent lung diseases: bronchiectasis, abscesses. Dose: 3-4 ml of solution twice a day.
FURACILLIN
Has moderate disinfectant properties. The most appropriate inhalations with for preventive purposes in patients with ARVI, to prevent the spread of infection deep into the bronchial tree. It is preferable to use a ready-made 0.02% solution, 4 ml per inhalation 2 times a day. You can prepare the solution yourself. To do this, 1 tablet of Furacillin is dissolved in 100 ml of a sterile solution of 0.9% NaCl.
4. Anti-inflammatory drugs
a) Glucocorticosteroids
BUDESONIDE
Suspension for inhalation via nebulizer, available under the trade name Pulmicort in plastic containers of 2 ml in three dosages - 0.125 mg/ml, 0.25 mg/ml, 0.5 mg/ml. The main indication for use is bronchial asthma. Daily dose ranges from 1 to 20 mg depending on the phase and severity of the disease.
b) Herbal medicine
It is an extract from plants that have anti-inflammatory properties and are traditionally used in herbal medicine - chamomile, calendula and yarrow. Indicated for the treatment of acute inflammatory diseases of the upper and middle respiratory tract. A solution for inhalation is prepared by diluting 1/2 teaspoon of rotokan in 100 ml of physiological sodium chloride solution. Therapeutic dose: 3-4 ml 2-3 times a day.
5. Antitussives
LIDOCAINE
In cases of obsessive dry cough, such as symptomatic remedy You can use lidocaine inhalation through a nebulizer. Lidocaine, having local anesthetic properties, reduces the sensitivity of cough receptors and effectively suppresses the cough reflex. The most common indications for lidocaine inhalation are viral tracheitis, laryngitis, and lung cancer. You can inhale a 2% solution of Lidocaine, available in ampoules of 2 ml twice a day. When prescribing several drugs simultaneously, the order should be observed. The first to be inhaled is a bronchodilator, after 10-15 minutes - an expectorant, then, after sputum is discharged, an anti-inflammatory or disinfectant.
- All solutions containing oils.
- Suspensions and solutions containing suspended particles, including decoctions and infusions of herbs.
- Eufillin, papaverine, platifillin, diphenhydramine and similar drugs as having no substrate effect on the mucous membrane.
PREPARATION OF SOLUTIONS
When preparing solutions, you must follow a number of rules.
Solutions for inhalation must be prepared under sterile conditions using 0.9% sodium chloride as a solvent. Do not use tap water (even boiled water). The containers in which the solution is prepared are pre-disinfected by boiling.
The prepared solution should be stored in the refrigerator for no more than a day. Before use, be sure to heat it in a water bath to a temperature of at least 20°C.
- these are ailments, usually referred to by the people as “a sore throat” and “a runny nose.” However, in reality everything is not so simple, because there is a whole series various diseases with seemingly similar symptoms, but they are completely different in terms of their course and approaches to their treatment.
Types and symptoms of upper respiratory tract diseases
TO inflammatory diseases upper respiratory include: sore throat, rhinitis, laryngitis, sinusitis, pharyngitis, adenoiditis And tonsillitis.
These diseases are among the most common, periodically affecting every fourth inhabitant of our planet. They are diagnosed all year round, but in Russia their peak falls in mid-September, mid-April. During this period, they are usually associated with acute respiratory viral infections. Let's look at each disease in more detail.
Rhinitis is an inflammation of the mucous membrane lining the nasal cavity. Appears in two forms: acute And chronic form.

The cause of acute rhinitis is a harmful effect on the nasal mucosa of infections of a bacterial or viral nature. This form of rhinitis is often a faithful companion to many infectious diseases akin to influenza, gonorrhea, diphtheria, scarlet fever, etc. With its development, swelling of the tissues of the nasal cavity is observed (the swelling area extends to both halves of the nose). In most cases, acute rhinitis occurs in three stages. At the first stage, lasting from 1–2 hours to 1–2 days, the patient feels severe itching and dryness in the nasal cavity, accompanied by frequent sneezing. All this is additionally accompanied by headache, general malaise, deterioration of sense of smell, increased body temperature, and watery eyes. The second stage will mark its arrival by the appearance (usually in large quantities) clear discharge from the nose, difficulty breathing and nasal sound when speaking. Well, during the third stage, the previously transparent and liquid nasal discharge becomes purulent-mucous, after which it gradually disappears. Breathing also gradually becomes easier.
Sinusitis. This disease consists of inflammation of the paranasal sinuses and in most cases is also a complication of corresponding infectious diseases. For example, these could be: scarlet fever, same acute rhinitis, flu, measles, etc. Like the previous disease, sinusitis has two forms: acute And chronic. The acute form, in turn, is divided into catarrhal And purulent sinusitis, and chronic – on purulent, edematous polyposis And mixed sinusitis.
If we talk about the symptoms of acute and chronic forms of sinusitis, which appear during periods of exacerbation, they are almost identical. To the most typical symptoms may include increased body temperature, malaise, frequent headaches, copious mucous discharge from the nose, nasal congestion (most often only on one side). One, several or all of the paranasal sinuses become inflamed, and other associated diseases occur. If only some of the paranasal sinuses become inflamed, then there is ethmoiditis, aerosinusitis, sphenoiditis, sinusitis or frontal sinusitis. If inflammatory processes affect all the nasal sinuses (on one or both sides), then this disease is called pansinusitis.
Adenoids. This is an increase in the size of the nasopharyngeal tonsil, which occurs due to hyperplasia of its tissue. Let us remind you that nasopharyngeal tonsil is a formation located in the vault of the nasopharynx and is part of the lymphadenoid pharyngeal ring. As a rule, children aged 3 to 10 years are susceptible to adenoiditis, and it is a consequence of infectious diseases such as scarlet fever, flu, measles etc.

One of the first symptoms of adenoiditis is difficulty breathing and copious mucous discharge from the nasal cavity. In turn, difficulty breathing causes poor sleep, fatigue, hearing impairment, lethargy and memory problems, decreased performance at school, nasal tone and systematic headaches.
If the disease is critically advanced, the patient’s nasolabial folds may smooth out, provoking the appearance of the so-called “adenoid” facial expression. In addition, laryngospasms form, twitching of the facial muscles begins to appear, and in particularly advanced cases, deformation of the chest and facial part of the skull occurs. All this happens in the background persistent cough and shortness of breath, sometimes anemia develops.
Chronic tonsillitis. The disease occurs due to inflammation of the palatine tonsils, which has become chronic. Chronic tonsillitis It most often occurs in children, and it practically does not threaten people of retirement age.

Pathogens chronic tonsillitis– bacterial and fungal infections, which affect the palatine tonsils, the harmful activity of which is aggravated adverse effects environment(air pollution, cold), gross violation of diet, as well as other independent diseases (caries, purulent sinusitis, adenoiditis or hypertrophic rhinitis). Prolonged contact of pathogenic microflora with the palatine tonsils, aggravated by the general weakness of the body, often becomes the cause of chronic tonsillitis. If it develops, some noticeable changes occur in the palatine tonsils: keratinization of the epithelium begins, the formation of dense plugs in the lacunae, proliferation of connective tissues, softening of lymphoid tissue, impaired lymphatic drainage from the tonsils, inflammation of regional lymph nodes. In addition, there is a violation of the receptor functions of the tonsils. Chronic tonsillitis divided into two forms: compensated And decompensated.
Angina ( scientific name: acute tonsillitis). It is an acute inflammation, in most cases affecting the palatine tonsils, as well as the lingual and pharyngeal tonsils, larynx or lateral ridges. This is "traditional" childhood disease, however, it also affects adults under the age of 35–40 years. The main causative agents of sore throat include microorganisms such as fungi of the genus Candida, staphylococci, streptococci, and so on.
Factors contributing to the development of sore throat are hypothermia and overheating, mechanical damage tonsils, decrease protective forces body, smoke and dust in the environment, etc. There are two main routes of infection with this disease: exogenous (most often) and endogenous. Infection by exogenous route is carried out by airborne droplets, as well as alimentary route, as for endogenous infection, it occurs as a result of the presence in the oral cavity or in the nasopharynx of one or another source of inflammation (diseases of teeth and gums, chronic tonsillitis etc.).
There are four types of sore throat:catarrhal, follicular, phlegmous And lacunar.
Symptoms catarrhal sore throat, manifested on the first day of the disease, are dry mouth and sore throat, accompanied by pain when swallowing. After this, the patient experiences an increase in temperature and a deterioration in general health, weakness and headaches. An initial examination of the pharynx reveals a slight swelling of the palatine tonsils (with changes in the posterior pharynx and soft palate are not observed). In addition to the described symptoms, patients with catarrhal tonsillitis experience an increase in lymph nodes and a slight change in blood composition.
As for follicular And lacunar forms of sore throat, then their manifestation occurs more acutely. The first symptoms include chills, a sharp increase in temperature, sweating, headache, general weakness, loss of appetite, aching joints, enlarged lymph nodes and the appearance of painful sensations in them. In addition, severe swelling of the palatine tonsils is also observed. In the case of the follicular form, festering follicles are clearly visible through the mucous membrane of the tonsils.
With lacunar tonsillitis, a yellow-white coating forms at the mouths of the lacunae, which over time completely covers the tonsils. It should be noted that in its pure form, any of these forms of angina is extremely rare; in the vast majority of cases, they occur “as a couple.”
It is highly advisable, if possible, for those suffering from a sore throat of any form to be protected from any contact with other people (in particular, children), since this disease is acutely infectious.
Lech tion In most cases, tonsillitis is treated at home. For this purpose, antibiotic drugs, local antimicrobial agents, antipyretic and tonic drugs are used.
Pharyngitis. This disease is an inflammation of the mucous membrane covering the surface of the pharynx. There are two forms of this disease:spicy And chronic pharyngitis.
Acute form can be found both as an independent disease and as one of the concomitant phenomena of ARVI. To the unfavorable factors that provoke the occurrence acute pharyngitis , can be attributed to: receiving too cold or too hot food and drinks, inhalation of cold or excessively polluted air.
Basic symptoms acute pharyngitis the following: pain when swallowing, dryness in the throat and mouth. In most cases, there is no general deterioration in health, as well as an increase in body temperature. During pharyngoscopy, inflammation of the posterior wall of the pharynx and palate can be detected. In its symptoms, acute pharyngitis is somewhat similar to catarrhal sore throat(however, in the latter case, the inflammation extends only to the palatine tonsils).
Treatment acute pharyngitis carried out by gargling with warm herbal decoctions And alkaline solutions having an anti-inflammatory effect.
As for chronic pharyngitis , then it is often a consequence of ignoring the treatment of acute pharyngitis. This unpleasant transformation is largely facilitated by smoking, alcohol abuse, sinusitis, rhinitis, diseases digestive tract. To general symptoms chronic pharyngitis common to all patients are dryness and painful sensations in the throat, feeling of a lump in the throat.
Laryngitis. A disease consisting of inflammation of the mucous membrane of the surface of the larynx. There are two forms of this disease:spicy And chronic laryngitis.
To the causes acute laryngitis in most cases, it can be attributed to excessive voice strain, severe hypothermia of the respiratory tract and individual independent diseases(whooping cough, flu, measles, etc.).

In case of illness acute laryngitis inflammation is observed both of the entire mucous surface of the larynx and of its individual sections. In areas affected by inflammation, the mucous membrane swells and becomes bright red. IN in some cases the inflammatory process can spread to the tracheal mucosa, causing the development of another disease - laryngotracheitis.
Ltreatment of upper respiratory tract diseases
- elimination or maximum possible reduction in the size of edema of the mucous membrane, as well as restoration of airway patency, for this purpose vasoconstrictors or decongestants are used;
- usage antimicrobials local action(ointments, sprays, etc.); such treatments are most effective in the early stages of the disease; for more late stages they complement and enhance (and sometimes replace) antibiotic therapy;
- destruction of pathogenic bacterial microflora;
- elimination of the accumulation of mucous masses in the upper respiratory tract: resort to the help of mucolytics containing carbocysteine or acetylcysteine, or herbal preparations.
It is also important to remember that the traditional treatment of inflammatory diseases of the upper respiratory tract is based on antibacterial drugs, most often taken orally.
It just so happens that respiratory tract infections cause maximum discomfort to patients and knock them out of their normal rhythm for several days. Most people do not tolerate infectious diseases well. But the sooner treatment begins for any illness caused by harmful microbes, the faster the infection can be dealt with. To do this, you need to know your enemies by sight.
The most common infections of the upper and lower respiratory tract
Almost all diseases become the consequences of penetration into the body and active reproduction of bacteria and fungi. The latter live in the bodies of most people, but strong immunity does not allow them to develop. Bacteria cannot miss their chance, and as soon as they manage to find a gap in immune system, microorganisms begin to act.
The most common viral respiratory tract infections include the following diseases:
- Sinusitis characterized by inflammation of the nasal mucosa. The disease is very often confused with bacterial rhinosinusitis, which usually becomes a complication of viral infections. Because of him bad feeling the patient remains for more than a week.
- Acute bronchitis - An equally common upper respiratory tract infection. When the disease occurs, the main impact falls on the lungs.
- Co streptococcal tonsillitis Probably everyone has encountered this in their life. The disease affects the palatine tonsils. Against its background, many people wheeze and temporarily lose their voice.
- At pharyngitis An acute inflammatory process develops on the mucous membrane in the pharynx area.
- Pneumonia- one of the most dangerous infections respiratory tract. People still die from it today. Characterized by complex lung damage. The disease can be one- or two-sided.
- No less dangerous flu. The disease is almost always very severe with high fever.
- Epiglottitis It is not so common and is accompanied by inflammation of the tissue in the epiglottis area.


Description:
Upper respiratory tract infections are infections of the mucous membrane of the respiratory tract from the nasal cavity to the tracheobronchial tree, with the exception of the terminal bronchioles and alveoli. Upper respiratory tract infections include viral, bacterial, fungal, and protozoal infections.
Causes:
In most cases, damage to the upper respiratory tract is of viral origin.
The etiological agents causing damage to the upper respiratory tract are different. There is a close dependence of the role of pathogens on the course of the disease: in acute rhinosinusitis and exacerbation of chronic rhinosinusitis, the main role is played by Streptococcus (Str.) pneumoniae (20–35%) and Haemophilus influenzae (H.) influenzae (nontypeable strains, 6–26% ). More severe cases of the disease are more often associated with Str. pneumoniae Much less common causes of rhinosinusitis are Moraxella (M.) catarrhalis (and other gram-negative bacilli, 0–24%), Str. pyogenes (1–3%; up to 20% in children), Staphylococcus (S.) аureus (0–8%), anaerobes (0–10%). The role of gram-negative bacteria (Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli, Proteus spp., Enterobacter spp., Citrobacter) in acute sinusitis is minimal, but increases with nosocomial infection, as well as in persons with immunosuppression (neutropenia, AIDS) and persons receiving repeated courses of antibacterial therapy. The causative agents of odontogenic (5–10% of all cases of sinusitis) maxillary sinusitis are: H. influenzae, less commonly Str. pneumoniae, enterobacteria and non-spore-forming anaerobes.
Symptoms:
Upper respiratory tract infections can occur in the following clinical forms: sinusitis, rhinitis, pharyngitis, laryngitis, tracheitis.
Viral nasopharyngitis.
The incubation period lasts 2-3 days. Symptoms of viral nasopharyngitis last up to 2 weeks. If symptoms last longer than two weeks, alternative diagnoses such as allergies or allergies should be considered.
Nasal symptoms. At the onset of the disease, rhinorrhea, nasal congestion, difficulty in nasal breathing, etc. occur. Clinically significant rhinorrhea is more typical of a viral infection. But with viral nasopharyngitis, within 2 - 3 days after the onset of symptoms, nasal discharge often becomes viscous, cloudy, white to yellow-green in color (activation of the saprophytic substance living on the mucous membrane, in normal conditions non-pathogenic flora). Thus, the color and transparency of the discharge cannot help clearly differentiate bacterial and viral infections.
In the throat there is pain and soreness, soreness and difficulty swallowing. Sore throat, as a rule, is present already in the first days of illness and lasts only a few days. If you complain of a feeling of a lump in the throat, you should pay attention to the back wall of the pharynx and the uvula - they may be involved in the inflammatory process. Mouth breathing due to nasal congestion can lead to dry mouth, especially after sleep.
The occurrence of a cough may indicate involvement of the larynx, or as a result of irritation of the pharyngeal wall by nasal discharge (postnasal drip). usually develops on the fourth or fifth day after the onset of nasal and pharyngeal symptoms.
Viral nasopharyngitis can also be accompanied by symptoms such as:
* Unpleasant smell from the mouth, which arises as a result of the release of waste products of pathogenic flora and products of the inflammatory process itself. Bad breath can also occur with allergic rhinitis.
* - loss of smell is secondary to inflammation in the nasal cavity.
* . Observed in most cases.
* Sinus symptoms. They include nasal congestion, a feeling of fullness and distension in the sinus area (usually symmetrically). Quite typical for viral nasopharyngitis.
* Photophobia and are characteristic of adenovirus and other viral infections. may be accompanied by pain in the depths of the orbit, pain with eye movement, or conjunctivitis. Itchy, watery, watery eyes are more common in allergic conditions.
* Fever. The fever is usually mild or absent, but in newborns and infants the temperature can reach 39.4°C (103°F). The fever usually lasts only a few days. With the flu, fever can be accompanied by a temperature of 40°C (104°F) or even higher.
* Side symptoms gastrointestinal tract. , and diarrhea can accompany the flu, especially often in children. Nausea and abdominal pain may occur with viral acute respiratory infections and streptococcal infections.
* Heavy. Strong muscle pain typical for influenza, especially against the background of a sudden onset of sore throat, accompanied by fever, chills, cough and headaches.
* Fatigue and malaise. Any type of URTI can be accompanied by these symptoms. Complete loss of strength and exhaustion are characteristic of the flu.
Bacteria.
When collecting anamnesis it is almost impossible to carry out differential diagnosis for viral and bacterial pharyngitis. If the symptoms do not go away within 10 days and gradually worsen after the first 5-7 days, it is quite possible to assume the bacterial nature of the disease. Group A hemolytic streptococcus deserves special attention as a pathogen. The presence of an episode in a personal history (especially with clinical carditis or a complicated defect), or household contact with a person who had a history of streptococcal infection, significantly increases the patient’s risk of developing acute or recurrent rheumatic fever. Suspicion of infection with group A streptococcus is confirmed by the presence of prolonged fever, as well as the absence of cough, rhinorrhea and conjunctivitis, which are more characteristic of. Bacterial pharyngitis is characterized by seasonal incidence from November to May, and also indicates the age of patients from five to fifteen years.
Pharyngeal symptoms (from the pharynx). There is pain or sore throat, soreness and difficulty swallowing. If the uvula and the back wall of the pharynx are involved in the inflammation process, there may be a sensation of a lump in the throat. Breathing through the mouth, due to nasal congestion, leads to a feeling of dry mouth, especially in the first half of the day. The streptococcal nature of pharyngitis is characterized by abrupt start and acute sore throat.
Nasal discharge. The discharge is usually viscous, mucous, whitish or yellow-green, which, however, does not always indicate a bacterial infection.
Cough. It may be due to the involvement of the mucous membrane of the larynx or upper respiratory tract in the process of inflammation, or due to nasal discharge (postnasal drip).
The following symptoms are also characteristic:
* Bad breath. It arises as a consequence of the release of waste products of pathogenic flora and products of the inflammatory process itself. Bad breath can also occur with allergic rhinitis.
* Headache. It is typical for streptococcal (group A) and mycoplasma infections, but can also be observed with URTI of a different etiology.
* Fatigue and general malaise. It is observed with any URTI, but a clear loss of strength is characteristic of an influenza infection.
* Fever. The fever is usually mild or absent, but in newborns and infants the temperature can reach 39.4°C (103°F).
* Availability. Indicative for, especially in children and adolescents under 18 years of age.
* . It is typical for streptococcal infection, but can accompany influenza and other acute respiratory viral infections.
* History of recent oral-genital sexual intercourse, which is especially important in cases of gonococcal pharyngitis.
Acute viral or bacterial.
Initial manifestations sinusitis is often similar to nasopharyngitis and other viral infections of the upper respiratory tract, since the nasal cavity is anatomically connected to the paranasal sinuses, which determines the generality of the inflammatory process. Sinusitis is characterized by a two-phase progression pattern, in which initially there is a temporary improvement, then a deterioration. Unilateral localization of symptoms confirms suspicions of sinus involvement. With complete extinction inflammatory symptoms within a week there can hardly be any talk of sinusitis.
Nasal discharge. Characterized by persistent mucopurulent discharge, pale yellow or yellow-green in color, which, however, is not a defining symptom, since discharge can also be observed with uncomplicated rhinopharyngitis. Rhinorrhea is usually mild and does not respond to decongestants or antihistamines. In some patients, nasal congestion predominates. Unilateral nasal congestion and mucopurulent discharge from one nostril indicate sinusitis.
Hyposmia, or loss of smell, is secondary to inflammation of the nasal mucosa.
Pain in the area of projection of the sinuses. In older children and adults painful symptoms, as a rule, are localized in the area of projection of the affected sinus. Characterized by pain localized in the forehead area, upper jaw, infraorbital region. Inflammation maxillary sinus may result in toothache on the affected side. Pain radiating to the ear may indicate otitis media or peritonsillar abscess.
Oropharyngeal symptoms. A sore throat may be the result of irritation from nasal secretions running down the back wall throats. Breathing through the mouth, due to nasal congestion, leads to a feeling of dry mouth, especially after sleep and in the first half of the day.
or bad breath. It arises as a consequence of the release of waste products of pathogenic flora and products of the inflammatory process itself. Bad breath can also occur with allergic rhinitis.
Cough. Inflammatory syndrome of the upper respiratory tract is accompanied by a constant flow of nasal mucous into the pharynx (postnasal drip), requiring more frequent cleaning throat, that is, accompanied by a cough. The cough that accompanies rhinosinusitis is usually present throughout the day. The cough may be most severe in the morning, after sleep, in response to irritation of the throat with secretions that have accumulated overnight. A daytime cough lasting more than 2 weeks suggests bronchial asthma and a number of other conditions. It is also possible that coughing exclusively at night may be a characteristic symptom of some other diseases. Cough caused by inflammation of the upper respiratory tract can sometimes be accompanied by vomiting due to irritation by secretions from the base of the tongue. Clinically significant amount purulent sputum may suggest pneumonia.
Increased body temperature. Fever is not entirely typical and is observed more often in children. The rise and fall of temperature occurs almost synchronously with the appearance and cessation of purulent discharge. In ARVI complicated by sinusitis, an increase in temperature often precedes the appearance of purulent discharge.
Fatigue and malaise occur as with any other upper respiratory tract infection.
This disease is more common in children aged 1 - 5 years, and is characterized by sudden appearance clinical symptoms:
1. Sore throat.
2. Drooling - difficulty or pain when swallowing, feeling of a lump in the throat.
3. - hoarseness or total loss vote.
4. The cough is predominantly dry, shortness of breath is observed.
Increased body temperature and weakness are observed in the same way as with other upper respiratory tract infections.
& nbsp &n bsp .
Nasopharyngeal (nasopharyngeal) symptoms. Laryngitis and tracheitis are often preceded by nasopharyngitis for several days. Swallowing is difficult or painful, and there may be a feeling of a lump in the throat.
Cough can be of several types:
* Dry cough. In adolescents and adults, it can manifest as a protracted, hacking, dry cough that follows the typical prodromal period of URTI. Minor hemoptysis may be present.
* Barking cough. Laryngotracheitis or croup in children can manifest itself as a characteristic barking, so-called “copper” cough. Symptoms may be worse at night. also produces a barking cough.
* Whooping cough is an attack of convulsive uncontrollable cough, which is characterized by noisy “moaning” sounds during inspiration and an almost complete cessation of breathing at the height of the attack. Whooping cough is more common in children. This cough often comes in coughing paroxysms of a dozen or more attacks in a row, and often worsens at night. The cough may persist for several weeks.
Posttussive symptoms are attacks of nausea and vomiting following a paroxysm of whooping cough.
- breathing disorder: