Hemorrhagic shock symptoms and treatment. Emergency conditions, shocks. Hypovolemic (hemorrhagic) shock. Urgent Care
Hemorrhagic shock is a complex, requiring urgent assistance the patient's condition, with heavy or moderate blood loss. Achieving a critical state occurs as a result of failure of a multisystem or multiorgan type.
Modulation failure blood cells is organic in nature, the pathology prevents the penetration of essential nutrients into the body tissues. There are also problems with constant access of oxygen and products energy plan. With hemorrhagic shock, there is no possibility of normal elimination of toxins and harmful, polluting elements from the body. Over time, oxygen starvation develops. Its intensity is determined by the specific rate of loss of the main nutrient fluid. This type of shock occurs when the body loses approximately 500 milliliters of blood or more. Such a difficult condition can cause the patient’s death, development anaphylactic shock, problems with pulmonary or brain activity. Blood circulation in the lungs or brain is disrupted, which causes the subsequent manifestation of all the described problems.
Prerequisites for the development of shock
The main prerequisite for the manifestation and subsequent development state of shock, is getting serious traumatic injuries leading to blood loss. In such cases, open and closed damage vessels of the blood circulation. Another reason can be considered severe bleeding, which is caused by diseases of the uterus, stomach and intestinal organs, and perforated ulcers. In addition, the described situations can become consequences of the development of cancerous formations, this is especially typical for the final stages of cancer.
The pathogenesis of hemorrhagic shock has a central link in the form of failures of the systemic circulation in the large or small circle. Decreasing rapidly total blood circulating in circles. Accordingly, the natural forces of the whole organism are unable to independently resist the current negative situation. Nerve receptors muscle endings transmit impulses that cause disorders normal operation hearts and failures vascular activity. Breathing quickens, blood circulation is centralized, biological fluid increases circulation in space internal organs. Over a period of time, there is a gradual isolation of all organs and systems from the blood supply processes of the entire body. In the lung system, the total volume of oxygen produced sharply decreases, which can lead to death.
Shock symptoms
Medical experts distinguish the following main symptoms of the development of a state of shock:
- The patient's mouth becomes very dry.
- Attacks of severe nausea appear and subsequently spread.
- The person begins to feel severe dizziness and a feeling of weakness.
- The vision becomes dark, and in some cases there is even loss of consciousness.
- A compensatory distribution of blood occurs, in the muscles its total amount decreases, in the skin various areas the body turns pale from this. It may also acquire a serous tint, which is especially typical for specific cases of loss of consciousness.
- Over time, the limbs gradually become moisturized and acquire a sticky tint from the protruding sweat.
- There is a disruption in blood circulation in the kidney area, which can lead over time to hypoxia, as well as other unpleasant disorders.
- The patient has severe shortness of breath, breathing function is severely impaired.
- Heart rhythms become erratic and excessive arousal appears.
Such symptoms allow specialists to diagnose the described condition. Pathology requires immediate identification, this is required so that there is a real opportunity to avoid death.
Classification
Classification of the condition under consideration is possible according to a number of characteristics. Below are some of them.
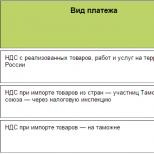
According to the degree of blood loss
By stage of development
The stages of development of the described syndrome are directly related to the stages of the described blood loss. When blood loss reaches 15%, initial stage hemorrhagic shock. The patient is fully conscious and is just beginning to feel weak. Subsequently, as the volume of blood lost increases general state the person deteriorates significantly. The second stage of development begins, followed by the third. When the level of blood loss reaches 45%, tachycardia indicators reach 160 pulses per minute. Possible loss of consciousness and central nervous system disorders nervous system. Subsequent disturbances in the processes of normal blood circulation can cause irreversible loss of plasma, coldness of the extremities, and permanent stupor. Respiratory system disorders increase sharply. Last stage the development of the described state of shock suggests the need for urgent hospitalization.
According to the Algover shock index
The rate of blood loss is critical when it is necessary to determine hemorrhoidal shock using the Algover index. The division of the index into systolic blood pressure, the indicator of which at normal position things cannot be below one.
According to the described index, the following categories of distribution degrees are accepted:
- Mild degree, the index takes values from 1 to 1.1.
- Moderate severity, index value in in this case accepted 1.5.
- Heavy variety. The index in this case is taken to be equal to a value not lower than two.
- Extreme degree gravity. The indicator of the described index value is assumed to be above 2.5.
Blood loss is the main indicator of the considered level of hemorrhoidal shock. Depending on the total volume Lost blood changes the value of the coefficient by which the Algover index is determined.
Diagnostic measures
The duration of the bleeding process and the level of blood lost are the main indicators for diagnosing the shock condition in question. Difficulties often arise with insufficient assessment of the volume of lost fluid and, as a result, delays in starting therapy occur.
Mandatory diagnostic measures in the situation under consideration are the following:
- the total volume of blood lost in the body is clarified as efficiently as possible; it is correlated with the exact, calculated volume;
- determined exact condition activity of the central nervous system, its mental and reflex functions;
- general condition is assessed skin at the current moment in time, their color, different shades, and changes in color scheme are taken into account;
- calculation is being carried out exact value shock index:
- The final value of hourly and minute diuresis is calculated.
The final stage of the diagnosis is an accurate assessment of the severity of the patient's condition. A structural diagnosis is made taking into account all the above factors. A subsequent strategy for providing effective medical care is being formed.
First aid
The principles of first aid for such a state of shock involve identifying the source of bleeding and its gradual elimination. Gynecological practice assumes in similar cases mandatory surgical intervention.
Subsequently, a speedy recovery is considered necessary. normal process blood circulation Simultaneously, catheterization of two main vessels located on the periphery should be performed. If the victim's condition is critical or close to it, it is necessary to perform intra-arterial injection of solutions.
All these measures are aimed at maintaining the proper level of oxygen consumption by the body’s tissues. Metabolism in them is maintained at the proper level. Extended artificial ventilation x body organs and lungs, precise maneuvering of gas systems and adequate pain relief are performed.
Means to stop bleeding:
Basics of treatment of hemorrhagic shock
The basis of therapy for hemorrhagic shock is stopping bleeding and taking everything necessary measures to eliminate the possibility of subsequent development of this condition.
Therapeutic measures
Infusion therapy is actively used in order to fully restore plasma volumes in the human body, which will help prevent dangerous complications and negative processes. To do this, it is recommended to use the following means:
- installation of plasma substitutes, in the manufacture of which bases from hydroxyethyl starch were used;
- crystalloid-type solutions are prescribed for use;
- colloidal solutions are used;
- doses of donor blood are poured in;
- drugs are used to constrict blood vessels, necessary for high-quality relief of their spasms.
Therapy methods
IN medical practice The following common methods of treating the shock condition in question are used:
- Elimination of hypovolemia and the procedure for restoring lost blood circulation volume.
- Carrying out detoxification.
- High-quality microcirculation and guaranteeing cardiac output.
- Stabilization of the initial values of bipolarity and the ability of blood to transport oxygen.
- Bringing in normal condition and subsequent maintenance of diuresis at the proper level.
- Prevention of the condition in question.
All considered therapeutic techniques only apply experienced specialists their business in medical institutions.
Preparations and means
Protein substances. Albumin in the form of solutions of concentration from 5% to 20%. Responsible for a qualitative increase in pressure and promotes the flow of fluids into the bloodstream. The increase in total plasma volume is facilitated by the use of protein proteins.
Plasma in dry and liquid states. It is transfused in compliance with safety regulations to prevent leaks and taking into account the established Rh factor. Dry plasma is diluted saline solution. Transfusion is carried out using organic and inorganic elements as blood substitutes.
Donor blood in canned form. When eliminating the consequences of a shock, blood transfusion and the use of appropriate solutions are not enough. It also requires the use of whole blood from a donor, to which coagulating substances are added.
Possible complications
Cardiac cessation is possible in case of large blood loss. In some cases there may be pathological changes conditions also after surgery and incorrectly performed therapy. Liver failure and hypoxia may develop as a result of a decrease in hemoglobin levels in the blood. An increase in the level of breathing is accompanied by the development pulmonary failure. At renal failure There have been cases of blood clotting disorders and other similar problems.
Prevention
Properly performed prevention is extremely important to prevent future similar situation. Prevention of hemorrhagic shock includes the following measures:
- prescribing particularly risky factors for signs of bleeding;
- qualified and high-quality care for victims at any stage with adherence to the prevention of complications due to bleeding;
- readiness medical personnel to any emergency measures on patient rehabilitation;
- coordinated implementation of all actions at all therapeutic stages;
- availability and bringing to full readiness of all necessary tools and medications to carry out the necessary activities.
Preventive measures may vary in the nature of implementation and degree of complexity depending on the nature of the development of the victim’s condition.
Hemorrhagic shock is essentially pathological loss of blood. When blood volume decreases sharply and by a significant amount, the body goes into stressful state. Usually the body saturates with about 5-6 liters of blood, even a slow loss of about 400 milliliters, which is usually taken from a donor, causes immediate weakness. That is why, after donating blood, to stimulate the restoration of the full volume of fluid circulating through the vessels, doctors strongly recommend drinking sweet warm tea with hematogen.
This reaction is provoked by slow blood loss, to say nothing of rapid blood loss. With a sudden loss of blood, the tone of the veins is increased, and the body is immediately thrown into shock from an instant decrease in blood volume. When the blood supply decreases, the body begins to function differently. More than 15% of the leak includes a kind of energy saving mode - the body switches forces to life-supporting organs: the heart, lungs, brain, and the remaining parts are considered secondary. There is hemorrhagic and hypovolemic shock. They are distinguished by and large only by the rate of decrease in blood volume. Hypovolemia does not provoke a catastrophic outcome, because the recovery algorithm is activated. This means that only shock during a rapid decrease in volume can be considered hemorrhagic.
Causes of hemorrhagic shock
The basis of hemorrhagic shock is serious. Acute leakage of fluid in the vessels implies the absence of half a liter to a liter of blood, combined with rapid decline amount of circulating fluid. This situation is usually provoked by serious injuries, which are accompanied by severe damage to blood vessels. Often hemorrhagic shock is a consequence of gynecological pathologies: trauma during childbirth, postpartum hemorrhage, prematurely separated placenta, intrauterine fetal death, ectopic pregnancy. Of course, heavy bleeding can happen after surgery when it disintegrates cancer tumor, the occurrence of a through hole and, as a result, a gastric ulcer.
Clinical manifestations
Manifestation acute blood loss directly depends on the amount of fluid lost. Doctors distinguish three stages of hemorrhagic shock. The division occurs in direct proportion to the volume of blood lost:
- Stage I. The degree to which compensation for lost fluid is still possible. The victim is conscious, maintains sobriety, looks quite pale, the pulse is palpable weakly, there is a low arterial pressure and decreased temperature of the extremities. Wherein lost volume does not exceed 15–25% of the total volume. The heart muscle tries to compensate for the missing fluid with the heart rate, so the heart rate increases to 90–110 per minute;
- Stage II. At this stage, the normal functions organs. The lack of a large volume of blood forces the body to distribute life support processes in accordance with the priority of specific organs. There is oxygen starvation of the brain, the heart pumps out blood noticeably weaker. Symptoms appear when there is a loss of 25 to 40% of circulating blood volume. The victim’s consciousness is disturbed - the person’s thinking is inhibited. The fluid in the vessels is critically low, so the face, arms, legs turn bluish, and protrudes throughout the body. sticky sweat. A thread-like pulse appears, blood pressure decreases, and the heart rate reaches 140 beats. The kidneys stop filtering fluid normally, urination decreases;
- Stage III. This is an irreversible shock. The patient's condition is considered extremely critical. Consciousness is completely absent, the skin acquires a marble tint, the pressure in the arteries decreases to 60-80 millimeters of mercury or is not detected at all. Tachycardia occurs - the heart contracts up to 140-160 times per minute.

How is the degree of blood loss determined?
Doctors determine the levels of shock stages using the Algover index. This number shows the proportional ratio of the number of contractions of the heart muscle to the upper blood pressure. The numerical value of the index directly depends on the severity of the victim’s condition. Normal indicator is within 1.0. Doctors further divide the severity of the indicator into:
- light, within 1.0 to 1.1;
- moderate severity, within 1.1 to 1.5;
- severe, within 1.5 to 2.0;
- critical severity, ranging from 2.0 to 2.5.
Severity
Of course, only the index indicator cannot be considered as absolute. Doctors see it in combination with blood loss. The classification of shock severity types is named in the same way as the indices, but requires the presence of a certain volume of blood. So, mild degree assumes a shock index of 1.0-1.1 and a blood loss of 10 to 20% of volume, but not more than 1 liter. Moderate severity - shock index up to 1.5, loss from 20 to 30% of volume, but not more than 1.5 liters. Severe degree - index up to 2.0, loss up to 40% or up to 2 liters. Extreme severity - index up to 2.5, loss more than 40% or more than 2 liters.
Diagnosis of the disease
Hemorrhagic shock (ICD 10 code - R 57.1) is classified as a condition similar to dehydration, which is characterized by a sharp decrease in the amount of blood found in the body. The focus of diagnosing the symptoms of hemorrhagic shock is to determine the amount of blood lost, the source of the leak, and its intensity.
The first step is to inspect the source of fluid leakage from the vessels. The doctor assesses the extent of the damage. Blood may flow out in a pulsating stream or spurt out. It is important to understand that leakage occurs suddenly, in large volumes and over a short period.

How to provide first aid
It is very important to correctly assess the condition of the victim. It is necessary to find the cause of bleeding and eliminate it as quickly as possible. Correctly provided first aid helps the victim recover from shock more quickly, and sometimes can even save his life.
So, let's figure out what needs to be done in case of hemorrhagic shock. First of all, it is necessary to localize the source of the loss. The area above the source of blood leakage should be bandaged with a bandage or tourniquet. The tourniquet usually puts a lot of pressure on the vessels and can damage them, so emergency doctors recommend using a rag or gauze bandage. It needs to be tightly bandaged over the wound, with a tight bundle wrapped on top, which after 1 hour will need to be gradually untwisted to avoid tissue death below the bandaged area. It is not recommended to take any further measures without doctors. You need to wait for the ambulance to arrive and be sure to write on the victim the time a tight bandage was applied so that doctors understand how long the wound is localized from the blood supply.

Treatment of hemorrhagic shock
After the ambulance arrives, doctors will begin to restore the volume of fluid in the vessels. If the leak is severe, the patient is given an infusion. If the blood loss is moderate or mild, then a special replenishment solution can be used - saline solution, blood substitute, red blood cell mass.
Possible complications
Hemorrhagic shock can cause quite serious complications. It all depends on the amount of fluid lost, its intensity, and the speed of localization of the source. Most complications occur due to oxygen starvation. This is damage to the mucous membrane of the lungs, mild brain exhaustion, damage to the functions of the brain, kidneys, and liver. In case of shock due to labor activity Irreversible damage to reproductive organs is possible.
So, we have found out how hemorrhagic shock manifests itself, what its degrees and stages are, and how to provide first medical care to the victim. If you still have questions after reading the article, feel free to write them in the comments.
Hemorrhagic shock in medicine refers to extensive blood loss, an unexpected release of blood from the blood vessels. This phenomenon usually develops quite rapidly and can lead to severe consequences, up to a tragic outcome. What are the signs to use to diagnose hemorrhagic shock, and what kind of help can those around them provide to a person with sudden bleeding?
Causes of hemorrhagic shock
Root causes of hemorrhagic shock - various damages, injuries, operations, etc.
For your information. According to medical statistics, hemorrhagic shock in obstetrics ranks first in frequency of occurrence.
Excessive acute blood loss occurs in expectant mothers in the following cases:
- gap fallopian tube- consequences of ectopic pregnancy;
- uterine rupture;
- some types of uterine bleeding;
- so-called acute fatty liver of pregnancy.
The consequences of this condition can be:
- development of cancer of the female genital organs;
- sepsis accompanied by tissue necrosis;
- ovarian apoplexy.
Hemorrhagic shock is also considered as a result of delayed or incorrectly selected therapy for such conditions/diseases as:
- cholera;
- diabetes;
- peritonitis;
- sepsis;
- cancer;
- osteomyelitis;
- long stay in an environment with elevated temperature air;
- pathology that provokes dehydration of the body, etc.
The following are considered indirect causes of shock:
- Incorrect assessment of bleeding characteristics - volume or speed.
- Incorrectly chosen method of replenishing lost blood.
- Incorrect/delayed error correction during blood transfusion.
- Late/incorrect choice of medications that can stop blood loss.
What determines the severity of the development of shock?
The basis of disruption of the body's vital functions during hemorrhagic shock is a sharp decline blood volumes distributed through the vessels. A decrease in the amount of blood provokes a spasm in these same vessels. The result is a transition tissue fluid into the blood vessels, which contributes to blood thinning and disruption of its microcirculation in organs.

Absence timely assistance threatens global failures of microcircular processes and threatens human health and even life.
The intensity of blood loss depends on a number of determining factors:
- body endurance;
- immunity strength;
- state of the nervous system (it is directly involved in the control of vascular tone);
- heart pathologies, etc.
The term “shock” in medical terminology refers to a critical state of microcirculation in the body, in which the total capacity of the vessels does not correspond to the volume of circulating blood.
One of the causes of shock may be acute blood loss - a sudden, immediate release of blood outside the vascular bed.
Such shock, which occurs as a result of acute pathological blood loss of more than 1% -1.5% of body weight, is called hypovolemic, or hemorrhagic.
The accompanying decrease in blood supply to organs and multiple organ failure are clinically manifested by tachycardia, a drop in blood pressure and pallor of the skin and mucous membranes.
The causes of hemorrhagic shock (HS) during acute loss can be divided into three main groups:
- spontaneous bleeding;
- post-traumatic bleeding;
- postoperative bleeding
Hemorrhagic shock often occurs in obstetrics, becoming one of the main causes of maternal mortality. Most often they lead to it:
- early abruption or placenta previa;
- postpartum hemorrhage;
- hypotension and atony of the uterus;
- obstetric injuries of the uterus and genital tract;
- ectopic pregnancy;
- vascular embolism with amniotic fluid;
- intrauterine fetal death.
In addition, the causes of hemorrhagic shock are often oncological pathology and septic processes leading to massive tissue necrosis and erosion of the vascular wall.
The rate of blood loss plays an important role in the occurrence of hemorrhagic shock. With slow bleeding, compensation mechanisms have time to engage, so hemodynamic disturbances develop gradually, without leading to serious consequences. Conversely, rapid blood loss of a smaller volume of blood inevitably leads to dangerous hemodynamic disturbances ending in hemodynamic syndrome.
Symptoms

The diagnosis of hemorrhagic shock is based on an assessment of its main clinical manifestations:
- states of consciousness;
- coloring of visible mucous membranes and skin;
- respiratory rate;
- condition and pulse value;
- level of systolic (BP) and venous pressure (VP);
- the amount of diuresis (volume of urine excreted).
Despite the importance of assessing the symptoms of hemorrhagic shock, relying only on the subjective sensations of patients is not only short-sighted, but also extremely dangerous.
Clinically significant symptoms appear, as a rule, already in the second, uncompensated stage of shock, the most significant of which is a steady decrease in blood pressure, indicating the depletion of one’s own compensation mechanisms.
How is the degree of blood loss determined?
For adequate and effective therapy For HS, it is important to accurately and timely determine the degree of blood loss.
Of the currently existing classifications of acute blood loss, the largest practical use got the following:

- mild degree (blood loss from 10% to 20% of blood volume), not exceeding 1 liter;
- moderate degree (blood loss from 20% to 30% of blood volume), up to 1.5 liters;
- severe degree (blood loss of about 40% of blood volume), reaching 2 liters;
- extremely severe or massive blood loss - when over 40% of blood volume is lost, amounting to more than 2 liters
IN in some cases Due to intense blood loss, irreversible homeostasis disorders develop that cannot be corrected even by immediate replenishment of blood volume. The following types of blood loss are considered potentially fatal:
- loss of 100% of circulating blood volume (CBV) during the day;
- loss within 3 hours of 50% of bcc;
- immediate loss of 25% of the volume of the central fluid (1.5-2 liters);
- forced blood loss at a rate of 150 ml per minute
To determine the degree of blood loss and the severity of hemorrhagic shock, it is used comprehensive assessment clinical, paraclinical and hemodynamic parameters.
Of great importance is the calculation of the Algover shock index, defined as the quotient when dividing the heart rate by the value systolic pressure. Normally, the shock index is less than 1. Depending on the degree of blood loss and the severity of shock, this may be:
- index from 1 to 1.1 corresponding mild degree blood loss;
- index 1, 5 — medium degree blood loss;
- index 2 - severe blood loss;
- index 2.5 - extremely severe blood loss
In addition to the Algover index, measuring the value of arterial and central venous pressure (BP and CVP), monitoring minute or hourly diuresis, as well as the level of hemoglobin in the blood and its relationship with the hematocrit (the specific gravity of the erythrocyte mass from the total blood volume) helps to clarify the volume of lost blood.
The following signs indicate a mild degree of blood loss:
- Heart rate less than 100 beats per minute, pale, dry and low temperature skin, hematocrit value from 38 to 32%, central venous pressure from 3 to 6 mm water column, diuresis value more than 30 ml.
Moderate blood loss is manifested by more pronounced symptoms:
- An increase in heart rate up to 120 beats per minute, agitation and restless behavior, the appearance of cold sweat, a drop in central venous pressure to 3-4 cm of water column, a decrease in hematocrit to 22-30%, and diuresis of less than 30 ml.
Severe blood loss is indicated by:
- Tachycardia more than 120 per minute, drop in blood pressure below 70 mm Hg, and venous pressure less than 3 mm H2O, severe pallor of the skin accompanied by sticky sweat, anuria (lack of urine), decrease in hematocrit below 22%, hemoglobin - less than 70 g/ l.
Video on the topic
Hemorrhagic shock is a serious, life-threatening condition that develops as a result.
This is because blood is one of the most important fluids in the body. It transports nutrients to tissues and organs that are necessary to ensure their normal functioning. Therefore, this problem is referred to as hypovolemic conditions or dehydration.
Causes of hemorrhagic shock
Causes of hemorrhagic shock - trauma of different nature, surgery etc. Anyway this state develops against the background of spontaneous bleeding. The rate of blood loss matters. If it is low, the human body has time to adapt and turn on special compensatory mechanisms.
Therefore, a slow loss of 1-1.5 liters of blood is not so dangerous. In this case, hemodynamic disturbances appear gradually and often do not lead to serious consequences for the body. With intense bleeding, which occurs spontaneously and is characterized by the loss of a large volume of blood, a person develops a state of hemorrhagic shock.
Also this problem often found in obstetrics. Massive blood loss may occur during pregnancy, difficult childbirth, or postpartum period. The development of hemorrhagic shock occurs in the following cases:
- rupture of the uterus, birth canal;
- abruption or placenta previa;
- termination of pregnancy for any reason, etc.
Bleeding very often occurs when a woman has accompanying pathologies. These include not only serious illnesses which were observed before, but also gestosis during pregnancy, severe injuries during labor.
What determines the severity of the development of shock?
The pathogenesis of the body's compensation for intense blood loss depends on many factors:
- the state of the nervous system, which is involved in the process of regulating vascular tone;
- presence of pathologies of cardio-vascular system, its ability to work effectively in hypoxic conditions;
- intensity of blood clotting;
- conditions environment(saturation of air with oxygen and others);
- general condition of the body;
- level of immunity.

Stages
The stages of hemorrhagic shock are usually divided based on the amount of blood loss and the severity of the person’s condition. Depending on these factors, it is customary to divide:
- first stage. It is also called compensated. In this case, there is a loss of no more than 15-25% of the total blood volume;
- second stage. Its second name is decompensation. It is characterized by more intense blood loss, which amounts to 25-40% of the total blood volume;
- third stage or irreversible. Characterized by serious condition, which is explained by the loss of 50% of the total blood volume.

Signs of the compensated stage in hemorrhagic shock
The first degree of hemorrhagic shock develops with a loss of about 0.7-1.2 liters of blood. This leads to the inclusion of special adaptive mechanisms of the body. The first thing that occurs is the release of substances such as catecholamines. As a result, with the development of hemorrhagic shock, the following symptoms appear:
- pale skin;
- desolation of veins in the arms;
- increase in the number of heart contractions (up to 100 beats per minute);
- decrease in the volume of urine excreted;
- development of venous hypotension, while arterial hypotension is completely absent or weakly expressed.
Such a clinical picture of hemorrhagic shock can be observed quite for a long time, even if blood loss has completely stopped. If the bleeding continues, there is a rapid deterioration in the person’s condition and the development of the next stage.
Signs of the decompensated stage of hemorrhagic shock
In this case, a loss of about 1.2-2 liters of blood occurs. Stage 2 hemorrhagic shock is characterized by increased disorders associated with the blood supply to the main tissues and organs. This leads to a drop in blood pressure levels. Against the background of circulatory disorders, it develops, which is reflected by insufficient intake of all nutrients to the tissues of the heart, liver, brain, etc.
Other developments are also taking place unpleasant symptoms hemorrhagic shock:
- a drop in systolic blood pressure below 100 mm. rt. Art.;
- development, which is accompanied by an increase in the number of heartbeats to 130 per minute;
- the pulse is characterized as threadlike;
- shortness of breath appears;
- the skin turns bluish;
- cold, sticky sweat appears;
- the patient is in a restless state;
- a sharp decrease in the volume of urination;
- central venous pressure decreases.

Signs of the third stage of hemorrhagic shock
The development of the third stage is accompanied by blood loss, the volume of which exceeds 2 liters. In this case, the patient's condition is characterized as very serious. To preserve its life, a variety of resuscitation measures. Stage 3 is usually indicated by the presence of the following symptoms:
- the patient is unconscious;
- the skin becomes marbled and pale;
- Blood pressure very often is not determined at all. Sometimes you can only measure top figure, which does not exceed 60 mm. rt. Art.;
- increase in heart rate to 140-160 beats per minute;
- with great skill, the pulse can only be detected in the carotid arteries.

Signs of shock in patients of the younger age group
The symptoms of hemorrhagic shock in children are not very different from those in adults. At the same time, everything possible complications develop more rapidly and pose a huge danger to the child’s life. Initially, the following symptoms appear:
- pallor of the skin. Over time, the body acquires a bluish, leaden or gray tint;
- characteristic marbling of the skin appears;
- the body is usually wet, the sweat is sticky and cold;
- lips and mucous membranes also become pale;
- the child first becomes restless, after which apathy towards everything that happens and slowness of reaction appears;
- all reflexes weaken;
- eyeballs are usually sunken;
- breathing is shallow, rapid;
- pulse weak, threadlike;
- blood pressure levels decrease.

Diagnosis of hemorrhagic shock
It is not difficult to determine the presence of this dangerous condition, since it is accompanied by significant blood loss. Taking into account the classification of hemorrhagic shock, you just need to carefully study all the developing symptoms, which allows you to choose the right treatment tactics and assess the degree of development of complications. Therefore, the following diagnostic techniques are used:
- determination of the shock index. To do this, calculate the ratio between heart rate and systolic blood pressure. There is a real threat to life if this indicator is 1.5 or more;
- measurement of hourly urine output. A life-threatening condition can be considered if the volume of urine excreted decreases to 15 ml per hour;
- measurement of the level of central venous pressure. If it is below 50 mm. water Art., the patient needs to restore the volume of circulating blood. If the central venous pressure is above 140 mm. water Art., treatment includes the mandatory use of cardiac drugs;
- determination of hematocrit. Indicate the degree of blood loss. Indicators below 25-30% are considered life-threatening;
- characteristics of ABS (acid-base balance).

First aid for hemorrhagic shock
Urgent Care for hemorrhagic shock consists of the following measures:
- First of all, it is necessary to establish and eliminate the cause of bleeding. For this, jutes, bandages and other devices are used. If the bleeding is internal, surgery is indicated.
- Before providing qualified assistance, it is necessary to ensure that the patient is in a supine position. If a person has not lost consciousness, he may inadequately assess his condition.
- If possible, it is recommended to provide the patient drinking plenty of fluids. This will help prevent dehydration.
- Treatment of hemorrhagic shock in mandatory involves restoring blood volume in the human body. If bleeding continues, then the intravenous infusion rate should advance the loss by 20%.

- To monitor the effectiveness of treatment measures, it is necessary to constantly monitor the main indicators of blood pressure, heart rate, and central venous pressure.
- Catheterization is mandatory large vessels, which allows the necessary drugs to be introduced into the bloodstream in a timely manner.
- In the presence of complications, artificial ventilation of the lungs can be performed as part of all resuscitation measures.
- To reduce the degree of hypoxia, patients are offered oxygen masks.
- Eliminate severe pain caused by injury, painkillers are prescribed.
- Except careful care For the patient, what will be needed at first is to warm him up.

Main treatment for hemorrhagic shock
After effective stop bleeding and catheter placement therapeutic measures are aimed at the following:
- It is necessary to completely restore the blood volume in the vascular bed.
- If necessary, detoxification is carried out.
- Undertaking adequate measures to normalize blood microcirculation.
- Provided optimal conditions to restore transportable blood function.
- Normal diuresis is maintained.
- Conducted preventive actions to prevent DIC syndrome.

Methods of infusion therapy
To restore blood volume in the human body and prevent many dangerous complications are used the following means for infusion therapy:
- plasma expanders, which are made on the basis of hydroxyethyl starch;
- crystalloid solutions;
- hemorrhage, in particular, red blood cells;
- colloidal solutions;
- donor blood;
- glucocorticosteroids in the maximum possible doses;
- vasodilators used to relieve vasospasm.

Possible complications
Hemorrhagic shock - dangerous condition, which, if incorrect or untimely treatment may lead to the patient's disability or death. This occurs against the background of development, oxygen paradox, asystole, myocardial ischemia, ventricular fibrillation, etc.
Due to circulatory disorders of the main organs, they begin to function incorrectly. This leads to disruption of basic vital important processes, which is the reason for the unfavorable outcome.