The first symptoms of jaundice in children. Jaundice syndrome in newborns. Is jaundice contagious in newborns?
Jaundice or icteric syndrome is a visible change in color skin and the child’s sclera turns yellow, which is caused by an increase in the level of bilirubin in the blood and tissues.
In most cases, icteric syndrome develops against the background of liver or biliary tract diseases.
Due to the fact that the main factor in the development of jaundice syndrome is damage to liver cells by hepatovirus, many call hepatitis jaundice. This is an erroneous, but popular name. In order to know what to do when icteric syndrome appears, you need to understand the causes of its occurrence, forms and manifestations.
Causes and mechanism of development of jaundice
With the physiological breakdown of red blood cells, indirect biliverdin is released, which is subsequently converted into free or indirect bilirubin. Then free bilirubin is captured by hepatocytes (functional liver cells) in which it binds with glucuronic acid, forming bound or direct bilirubin, which enters the intestine with bile and is excreted from the body. digestive tract. A small part of the conjugated bilirubin is absorbed in the intestine and excreted in the urine.
The cause of the development of icteric syndrome is the appearance of disturbances in the cycle of formation and excretion of bilirubin, in which its concentration in the blood increases.
The reason for this situation may be:
the formation of too much bilirubin in the absence of disturbances in its excretion; impaired excretion of conjugated bilirubin at a normal rate of formation.
In most cases, the cause of the development of icteric syndrome is viral hepatitis of various types, which destroys liver cells and disrupts the binding of bilirubin, which causes a significant increase in its concentration in the blood.
Types of jaundice in a child
Depending on the concentration of bilirubin, we can talk about true and false jaundice syndrome; symptoms of jaundice in newborns are also distinguished.
False (keratin) jaundice
A condition in which the yellow color of the skin of the soles, palms and face is caused by eating large amounts of foods, medications or dietary supplements that contain carotene. The reason for the change in skin tone in this case is the accumulation of carotene derivatives in it. To products with big amount carotene can be found in carrots, oranges, and pumpkin. This pathology develops in children aged from one to 2.5 years. And since the child was not sick with anything, treatment for false jaundice is not required, everything should be done - just reduce the amount of carotene in the diet.
True jaundice
True jaundice in children develops only when the concentration of bilirubin in the blood increases.
Depending on what stage of the cycle of elimination of this substance from the body the failure occurred, three forms of icteric syndrome can be distinguished:
Hemolytic (suprahepatic) - develops with increased formation of bilirubin. Parenchymal (liver) - in this form, the binding of free bilirubin in liver cells is impaired due to their damage caused by various diseases. Obstructive or subhepatic - also called mechanical and is associated with a violation of the excretion of the bound form.
With viral hepatitis, a parenchymal form of true jaundice develops, which in some situations can occur without a pronounced change in the color of the skin.
Jaundice syndrome in newborns (physiological jaundice)
Physiological infant jaundice develops in infants 2-3 days after birth; this condition is a sign of the baby’s adaptation to new living conditions. Jaundice syndrome occurs due to an immature enzyme system and impaired bilirubin metabolism. Changes in skin and sclera color are perhaps the only symptom that manifests this condition. Most often, such jaundice develops in premature babies; it is not transmitted to people around the child. Specific treatment not required, unnatural skin coloring goes away on its own within 7-10 days. Jaundice one month old baby is not physiological; when it appears, you must urgently consult a doctor to identify the causes of the development of the pathology.
Types, routes of transmission and clinical picture of viral hepatitis
Currently, several hepatitis viruses have been discovered, but three of them are the most common: viruses type A, B, C, D, E.
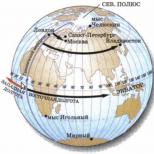
Routes of transmission of viral hepatitis
Experts identify several routes of transmission of infection:
Fecal-oral – virus particles enter the feces child, microparticles of which can contaminate objects, hand skin and soil. The virus is transmitted by failure to follow hygiene rules, by using shared utensils, toys, personal hygiene items, by contact or playing with a carrier of the virus, or by eating unwashed vegetables or berries. Viral hepatitis A and E, also called dirty hands disease, are transmitted in this way. When diagnosing a disease in one child from a group in kindergarten in most cases, quarantine is declared. Parenteral - infection occurs through contact with blood or other biological fluids (saliva, tears), during medical procedures, dental treatment, and surgical interventions. During breastfeeding, the hepatitis virus can enter the child's body if there are cracks or wounds on the mother's nipples or areola, and it is not contained in breast milk. The hepatitis B, C and D virus is transmitted parenterally. Vertical - transmission of the virus from mother to child during pregnancy (in utero) or the moment he is born, most often the type B virus is transmitted this way.
In order to create immunity against the hepatitis B virus, vaccination is done on the first day of the baby’s life, and revaccination is carried out according to a schedule for up to a year.
Clinical manifestations of various types of hepatitis
Depending on the type of virus, infants with an infectious inflammatory process have a different clinical picture of the disease. Features of the course of each type of hepatitis appear with varying intensity, which is due to the severity inflammatory process, the child’s age and the state of his immune system.
Hepatitis type A
In 15 cases out of 100, infection occurs in a kindergarten, more often in those groups in which there are children under 3 years old who do not know how to use a potty. The disease, caused by the type A virus, spreads rapidly and is characterized by quite light current and a favorable outcome in most cases. The virus may not die for a long time in an open environment under favorable conditions; when boiled, it dies in 4-5 minutes. The period from infection until the first signs of the disease appear is called incubation; it can last from 7 days to 5 weeks.
Manifested by the following symptoms:
Symptoms general intoxication the body are the first signs of the disease - they appear even before the color of the skin changes. These include chills, fever, fever, headaches, weakness and fast fatiguability, aching bones and muscles. Clinical manifestations from the outside digestive system develop during the first week of the disease - bitterness in the mouth, nausea, frequent urge vomiting, pain in the right hypochondrium, diarrhea (in this case, the stool becomes light, almost discolored), enlarged liver and spleen. Change in the color of urine - it takes on a shade from reddish-brick to brown, due to great content bilirubin that enters the urine from the blood. Skin symptoms appear at the beginning of the second week, gradually increase and begin to subside at 3-4 weeks of the disease. Manifestations from the skin include severe itching, which develops as a result of stagnation of bile, then a change in color of the sclera and oral mucosa appears, after which the skin turns yellow.
After the signs of jaundice disappear, the child will need at least six months to full recovery health. Hepatitis E virus manifests itself with symptoms similar to the clinical picture described above; they will help establish the correct diagnosis laboratory methods diagnostics
In infants, as well as during the first years of life, hepatitis A can occur without severe symptoms.
Depending on the totality of symptoms of the disease, several types can be distinguished:
icteric typical – the only symptom absent is itching of the skin; icteric form with a pronounced cholestatic component - the period of icteric syndrome is long and joins itchy skin; icteric atypical – a rare form of the disease, characterized by the absence of intoxication symptoms and severe severity skin signs and itching, most cases are diagnosed in adolescent children; anicteric – there are no skin symptoms, the development of this form is indicated by weakness, pain in the right hypochondrium and lack of appetite; often diagnosed in an advanced form, since the symptoms are mild; subclinical - only an increase in the size of the liver can indicate the development of hepatitis; other signs are completely absent.
Hepatitis A causes the development of stable immunity - if a child has this disease even in the first months, he is protected from re-infection for life.
Hepatitis type B
Hepatitis type B is a disease transmitted parenterally or vertically. Jaundice syndrome in this form of pathology does not occur in all cases, but if it develops, it has pronounced manifestations.
Features of symptoms of acute hepatitis B:
sudden increase in body temperature to 38.5-39 degrees; the appearance of attacks of nausea and vomiting; severe pain in the right hypochondrium; significant increase in size and hardening of the liver.
With a long course, skin rashes may appear, nosebleeds may develop, menstruation is heavier than usual in girls, gingivitis (inflammation of the gums), damage to the spleen, pancreas, and bile ducts may occur.
If treatment is started untimely or prescribed incorrectly, acute form the disease becomes more severe chronic, which is characterized by long periods remissions followed by exacerbations. To prevent a child from getting hepatitis B, he is vaccinated while still in the maternity hospital in order to cause the development of immunity to this disease. Since the formation of immunity does not occur immediately, revaccination is carried out during the first years of life. To maintain immunity, starting from adolescence, it needs to be done every 5 years. In some cases, if there are medical outlets up to one year old, vaccination against hepatitis B begins later; in any case, vaccination against this disease will protect the child from the possibility of becoming infected with it in the future.
Hepatitis type C
The most dangerous form of the disease, in most cases developing primarily chronic, and even with acute hepatitis In almost 80 cases out of 100, the disease becomes chronic. The virus is transmitted predominantly parenterally; infection of the child from the mother during pregnancy is observed in 5-6% of cases. The disease can occur typically (accompanied by icteric syndrome) or atypically (anicteric form).
Features of clinical manifestations:
feeling unwell for a long time; lethargy, chronic fatigue and weakness in the child; decreased appetite; in 20-35% of cases, icteric syndrome develops, lasting 7-21 days; significant increase in liver size (hepatomegaly).
In infants and young children it develops predominantly atypical form diseases, which often leads to the development chronic pathology and fibrotic degeneration of the liver. Typical form of acute hepatitis C childhood in most cases it has a mild or moderate course. A severe and malignant (often fatal) course is extremely rare.
Methods for diagnosing hepatitis
The following laboratory methods are used to confirm the diagnosis:
blood biochemistry; study for markers for hepatitis; enzyme immunoassay of venous blood; analysis PCR method; ultrasonography liver; needle biopsy of the liver.
Hepatitis Treatment Methods
Treatment for any form of hepatitis can only be prescribed by a specialist; attempts to cure the disease at home without consulting a doctor (especially in infants) can lead to serious complications, including fatal outcome.
First of all, when hepatitis develops, it is prescribed dietary food(table No. 5 according to Pevzner), if the disease is observed in infants, a change in diet will be suggested to the mother.
The following groups of drugs are prescribed:
hepatoprotectors; choleretic drugs; vitamin complexes; sorbents; interferons; medicinal mineral water(in case of illness in infants, the doctor will determine whether it is possible to use it).
For infants and young children, the dosage and route of administration of drugs is determined individually.
For a speedy recovery of the child, parents must strictly follow all doctor’s recommendations regarding regimen, nutrition, medication and fluid intake. Treatment of this disease is always carried out in a hospital; after discharge, a child who has suffered from hepatitis remains under the supervision of a doctor on an outpatient basis for quite a long time. Features of monitoring patients chronic forms diseases consist of registration at a dispensary; in case of exacerbations, hospitalization is necessary, and after them sanatorium-resort treatment.
Gastroenterologists in your city
Select city:
To the question “What is hepatitis?” very often you can hear the answer: “jaundice.” However, a icteric tint of the skin is not yet an indicator of hepatitis; forms of the disease are erased and anicteric. The names of hepatitis viruses are similar to the alphabet – A, B, C…. Let's talk about hepatitis viruses and discuss the first signs of jaundice in a child.
Ways of transmission of infection:
fecal–oral– ingestion of particles of the patient’s secretions containing virus A with food through the mouth;
parenteral– through infected blood and biological fluids (saliva, tears, breast milk). Characteristic of hepatitis B and C viruses;
Botkin's disease - hepatitis A– dirty hands disease – the most common form viral hepatitis, although it is the most favorable, and those who have recovered from this form of jaundice acquire long-term immunity. The hepatitis A virus lives approximately 30 days at a temperature of +25 degrees in external environment, and in water - for 3-10 months. When boiled, it dies within 5 minutes.
The first signs of jaundice caused by the hepatitis A virus in a child:
The pre-icteric period lasts 5-7 days;
A sharp increase in body temperature;
The occurrence of weakness, headache, body aches;
Chills and fever;
Liver damage and gastrointestinal tract. Children complain of bitterness in their mouths sharp pains in the right hypochondrium;
Deterioration of appetite, complete aversion to food may occur;
The appearance of diarrhea and vomiting;
With severe stagnation of bile, severe skin itching begins;
After 2-3 days, a change in the color of urine is noted, it becomes the color of beer or strong brewed tea;
Feces, on the contrary, become discolored.
Very young children may have minimal or no symptoms.
The icteric period is optional and lasts 7-15 days. First of all, the mucous membrane of the mouth turns yellow, then the sclera, and only then the skin. When jaundice appears in a child, intoxication subsides, but weakness and loss of appetite persist for a long time. The outcome of hepatitis A is favorable; in 90% of cases, complete recovery occurs within 3-4 weeks from the onset of the disease. The recovery period after illness is longer and ranges from 3 to 6 months.
Serum hepatitis – hepatitis B- a much more dangerous disease. The symptoms are very similar; in children, the infection is often asymptomatic; clear complaints arise only in adults.
The first signs of jaundice caused by the hepatitis B virus in a child:
The pre-icteric period lasts 7-12 days;
Increased body temperature;
The occurrence of nausea, vomiting;
Headache, joint pain;
Enlarged liver and spleen;
Skin rashes are possible.
The occurrence of jaundice in children with hepatitis B is not very typical, but if it does exist, it is expressed very clearly; in some children, the gums bleed and from nose goes blood. The duration of the jaundice period is 1-3 weeks. The recovery period lasts up to three months. Children often complain of weakness for a long time; they have an enlarged liver, damage to the biliary tract, and pancreas. These symptoms do not indicate the development of chronic hepatitis. At full recovery stable lifelong immunity is developed. Erased, asymptomatic forms often become chronic.
The most insidious - hepatitis C– his virus “escaps” from under protective forces body, constantly changing. This ability allows it to live in the body for many years, sometimes throughout a person’s life. With hepatitis C, more often than with other types, passive virus carriage occurs, during which the virus has a destructive effect on the liver without manifesting itself external signs. Most patients with hepatitis C often experience the phenomenon of “imaginary recovery,” in which blood tests are normal for several weeks or months, and sometimes these periods are mistaken for recovery. You can get sick with hepatitis C again, even if treatment was successful, immunity to this hepatitis virus is not developed. Because of this, it is impossible to create a vaccine against hepatitis C.
The first signs of jaundice caused by the hepatitis C virus in a child:
Deterioration in health;
Lethargy, weakness;
Fast fatiguability;
Loss of appetite;
Mild yellowing of the sclera;
Short-term darkening of urine;
Short-term lightening of stool.
Recovery from acute hepatitis C most often occurs with the icteric variant of the disease. In 80% of patients, hepatitis C becomes chronic.
Diagnosis of jaundice in children:
Biochemical blood test;
Blood test for antibodies;
PCR (polymerase chain reaction);
ELISA (enzyme-linked immunosorbent assay);
Ultrasound (ultrasound examination) of organs abdominal cavity;
Liver puncture biopsy.
Treatment of jaundice in children:
Bed rest before the onset of a “urinary crisis” is mandatory;
Diet - stick to acute period Necessarily. Important in therapeutic nutrition are vegetable fats, products containing protein, having a lipotropic effect ( oatmeal, cottage cheese, low-fat fish), easily digestible carbohydrates (honey, fruits, compotes, fruit drinks), fried, smoked, hot, spicy foods are strictly prohibited;
The use of vitamins, active regulators of metabolic processes, vital activity of cells and tissues, is an important part of treatment. Vitamin preparations should be taken with caution to avoid allergic reactions, it is better to include more fruits and vegetables in your diet;
Use choleretic drugs only during the recovery period;
Prescribing enterosorbents to relieve symptoms of general intoxication, release toxic products from the gastrointestinal tract, enhance the evacuation of bile acids, and prevent their absorption in the intestine;
For hepatitis B, antiviral treatment is prescribed under medical supervision. Drugs that improve metabolic processes in liver cells are also used. After recovery from jaundice, the child is exempt from physical education for six months.
Tags: signs of jaundice
Jaundice is a significant increase in the level of the bilirubin component in the blood of adults and children, which manifests itself in the acquisition of a yellow tint to the skin, mucous membranes and sclera of the eyes. It is not an independent disease, but a symptom of disorders in the body.
Bilirubin is a yellow pigment released when red blood cells break down in the body. The red blood cell cell is destroyed and the component bilirubin is released into the blood.
Typically, the liver neutralizes it and removes it from the body in the form of bile. However, if metabolic processes are disrupted, this can lead to icteric syndrome.
When diagnosed with jaundice, the symptoms of yellowing of the skin and mucous membranes are caused by an increase in the rate of destruction of red blood cells (hemolysis), which suppresses the liver’s ability to neutralize harmful cells. We will look at how to identify jaundice later in the article.
Causes of icteric syndrome
Mostly newborn children suffer from this disease. But there are frequent cases of the disease manifesting itself in adults.
Jaundice most often occurs as a manifestation of a variety of liver diseases, which causes excessive saturation of the blood with bilirubin and interferes with the removal of excess cells from the body.
Possible causes of icteric symptoms in adults:
Symptoms of icteric syndrome
The main symptoms of jaundice are the appearance yellowish tint white area of the eyes and skin, as well as dark-colored urine. An increase in bilirubin in the blood can be detected by medical examination. The presence of yellowness of the eye shell in adults indicates high concentration bilirubin in the body – at least 3 mg/dl.
 However, you need to be careful possible complications. Hyperbilirubinemia occurs due to an increase in the unconjugated fraction. In this case, bilirubin actively accumulates in the gray matter of the central nervous system, which can ultimately lead to cretinism.
However, you need to be careful possible complications. Hyperbilirubinemia occurs due to an increase in the unconjugated fraction. In this case, bilirubin actively accumulates in the gray matter of the central nervous system, which can ultimately lead to cretinism.
Depending on the degree of exposure, effects range from clinically subtle effects to serious injury and even death.
Signs of jaundice are divided into three categories, depending on which part of the physiological mechanism is damaged.
| Category | Causes | Symptoms |
|---|---|---|
| Hepatocellular (hepatocellular) | Diseases (viral, alcoholic) of the liver or its injuries |
|
| Suprahepatic (hemolytic) | Hemolysis (accelerated destruction of red blood cells) leads to increased production of bilirubin |
|
| Subhepatic (obstructive; mechanical) |
Biliary obstruction (the system of channels that carries bile from the liver to gallbladder And small intestine), which retains bile in the liver |
|
Symptoms of jaundice are often observed in newborns in the first 1-2 weeks of life. This is a common condition, affecting more than 50% of newborns, especially premature babies (boys more often than girls).
Infant jaundice is rarely a cause for concern and usually goes away on its own. However, in some cases, jaundice in a child can lead to brain damage and even death. It is not always possible to recognize the signs of pathological forms of jaundice in newborns.
 In a child, jaundice most often occurs due to a physiological excess of bilirubin. Hemoglobin (red blood cells) mothers, who provide oxygen supply to the baby in the uterus, after birth in the baby’s blood, as unnecessary, begin to actively disintegrate.
In a child, jaundice most often occurs due to a physiological excess of bilirubin. Hemoglobin (red blood cells) mothers, who provide oxygen supply to the baby in the uterus, after birth in the baby’s blood, as unnecessary, begin to actively disintegrate.
This provokes an increase in the level of bilirubin in the child’s body, and the child’s underdeveloped liver cannot promptly filter and remove excess bile from the body. This is considered a normal physiological condition in newborns.
In some cases, signs of jaundice in children may be caused by one of several underlying disorders:

The most common symptoms are jaundice (yellow color of the skin and whites of the eyes) and dark urine. Typically, yellowing in a child begins from the head, and then spreads to the chest, abdomen, arms and legs and goes away quite quickly.
However, it is worth remembering that this symptom may be a sign of pathological jaundice in a child (the symptoms in this case intensify and do not go away for a long time), which can cause significant harm to the baby’s body.
Therefore, it is extremely important to consult with a specialist in time and begin treatment of the diseases that caused icteric syndrome.
In contact with
Classmates
Doctors often diagnose jaundice in children. But this does not mean that liver pathology is present. The skin of newborn babies may turn yellow because the level of bilirubin in the blood is elevated. But at the same time, the nervous system can remain unharmed. And as soon as the main filter returns to normal, the manifestations will disappear. It's another matter if we're talking about about infection with the hepatitis virus. Then, after identifying the cause, appropriate therapeutic measures will be needed.
Thus, jaundice occurs:
- hemolytic (suprahepatic);
- parenchymal (liver);
- obstructive (subhepatic).
In the first case, the syndrome appears as a result of excessive breakdown of red blood cells. Therefore, too much bilirubin is produced. Tests will show anemia.
In the hemolytic form, symptoms occur:
- the skin, sclera and mucous membranes acquire a yellow tint;
- the level of indirect bilirubin increases;
- stool changes color to dark brown;
- the liver and spleen increase in volume;
- The lifespan of red blood cells decreases.
If the syndrome is caused by pathological changes in hepatocytes or in its bile ducts, then the jaundice is diagnosed as hepatic. That is, the hepatic metabolism of bilirubin is disrupted.
When jaundice syndrome is a consequence of an obstructive form, in other words, mechanical, it means that there are problems with the outflow of bile.
The following signs are observed:
- the syndrome increases gradually;
- urine has a so-called beer color;
- stools become colorless clayey, and fatty acids are detected in large quantities;
- blood tests reveal that cholesterol, bilirubin, bile acids and alkaline phosphatase are present in excess.
Attention should be paid to physiological jaundice, which manifests itself in newborns. Jaundice small child, which has just been born, is not considered dangerous. This condition indicates that the body is trying to adapt.
Why then does the syndrome occur? Certain symptoms are present due to the fact that the children's enzyme system has not yet fully matured, and bilirubin metabolism is impaired. IN in this case, the skin and sclera turn yellow. No other symptoms occur.
The syndrome is usually diagnosed in premature babies. There is no need for any treatment. Such symptoms will go away on their own in 10 days. But if the syndrome is detected in a one-month-old baby, then this condition should under no circumstances be ignored.
If the cause of jaundice is the hepatitis virus
When signs of jaundice occur, this does not mean that hepatitis is developing. But jaundice can be caused by his virus.
As a result of infection with hepatitis A, the first symptoms are as follows:
- the duration of the pre-icteric period is about a week;
- temperatures are rising rapidly;
- there is weakness, aches and headache;
- there is a fever and chills;
- the liver and gastrointestinal tract (gastrointestinal tract) are affected, which is expressed in the form of bitterness in the mouth and sharp pain in the side of the right side;
- Appetite may completely disappear;
- the child suffers from vomiting and diarrhea;
- little patient suffers from severe itching skin (if bile stagnation is pronounced);
- urine darkens and stool loses color.
If children are very young, then symptoms are often absent or mild.
A more serious illness is infection with hepatitis B. Signs are also often not observed.
But in general it is worth mentioning the presence of:
- elevated temperature;
- nausea and vomiting;
- headaches, aching joints;
- enlarged liver and spleen;
- skin rashes (sometimes).
The pre-icteric period lasts from 7 to 12 days. If the disease occurs, it is clearly expressed. Sometimes you can observe bleeding from the gums and nose.
But hepatitis C is considered the most insidious. The virus often remains in the body for life. Often the patient becomes a passive virus carrier. In this case, the liver is destroyed, but the disease does not manifest itself in any way.
The first symptoms are:
- the child complains of deterioration in health;
- he is lethargic and weak;
- gets tired quickly;
- appetite weakens;
- the sclera acquires a slight yellow tint;
- urine darkens for a short time;
- The feces become lighter for a short period.
If the icteric variant develops, patients with acute hepatitis recover much more often.
Features of therapeutic therapy
As soon as the first manifestations make themselves felt, it is immediately necessary to undergo an examination. This way the doctor can decide what treatment will be.
Without a diet, recovery will be much longer.
If we talk about nutrition in a few words, preference is given to:
- carbohydrates that are easily digested.
- products containing protein and having a lipotropic effect;
You should forget about fried, spicy, smoked and spicy dishes.
Successful treatment is impossible without taking vitamins. The main thing is to carefully use vitamin preparations, otherwise allergies cannot be ruled out. It is recommended to eat enough fruits and vegetables.
- Drugs with a choleretic effect are used only after the onset of the recovery period. To eliminate general intoxication, enhance the excretion of bile acids and avoid their absorption in the intestines, enterosorbents are prescribed.
- Antiviral treatment in the presence of hepatitis B must be supervised by a doctor. When the disease passes, the child may not attend physical education classes for six months.
- Treatment may not be necessary if the child is vaccinated on time. Vaccination has become especially popular in Lately. Sometimes vaccination helps prevent infection. Immunoprophylaxis is necessary to prevent the infection from spreading.
The hepatitis A vaccine is given to people of any age. It is well tolerated by the body. There are two stages of vaccination. Between stages should pass from 6 to 12 months. After two weeks, antibodies appear. The duration of protection is about 10 years.
The vaccination, which is done to protect the body from hepatitis B, differs in the content of immunogenic protein substance. Since the disease can be contracted through blood, everyone who deals with it should be vaccinated.
In maternity hospitals, vaccinations are mandatory for infants. After month period the procedure is repeated. The third approach is after 5 months. This is how the baby produces specific antibodies, which helps prevent the development of the disease when the virus penetrates.
Probably, many are familiar with the term jaundice, the symptoms of which in children and adults include the coloring of the skin and mucous membranes in a yellowish color. This process is caused by the accumulation of pigment - bilirubin - in the tissues. Jaundice is not a separate disease, it is rather a sign or a kind of signal that something “abnormal” is happening in the body. And it’s always scary when a similar phenomenon occurs in a small child. So what is hidden under the term “jaundice”? How is she treated? What are the signs of jaundice in children and adults?
What is bilirubin?
Before delving into the essence of this yellow syndrome, you need to understand what bilirubin is. Simply put, it is a coloring pigment of bile, which is a product of the breakdown of hemoglobin. Under normal conditions, bilirubin accumulates in the digestive tract and is then excreted from the body. naturally, that is, through feces. But if a person has an unhealthy condition in which this pigment is not excreted and begins to accumulate in the blood, his skin and sclera acquire a yellowish tint.
Bilirubin: normal
Normal bilirubin levels in healthy people are as follows:
- General – up to 20.5 µmol/l.
- Direct – up to 5.1 µmol/l.
- Free – up to 16.2 µmol/l.
It is worth noting that bilirubin is an extremely dangerous compound. It is very toxic to our body. Its significant excess has Negative influence on human health. Excess bilirubin leads to intoxication of the entire body and malfunction of organs. This exposure is especially dangerous for newborns.
Types of jaundice and main causes
The symptom of jaundice itself develops only in three cases:
- Firstly, if bilirubin is formed in excess.
- Secondly, if the processing process of this enzyme is disrupted.
- And thirdly, if its excretion is impaired.
Based on these three cases, three forms of jaundice are distinguished:
- Suprahepatic. In this case it happens overeducation bilirubin due to increased breakdown of red blood cells, and the liver simply does not have time to process it.
Prehepatic jaundice develops with the following diseases and certain causes:
There is also the so-called false jaundice, which appears due to the consumption of foods with a large amount of keratin. Similar signs of jaundice in children (1 year - 2.5 years) occur if the baby eats a lot of carrots, pumpkin or oranges.
The first signs of jaundice in children
Each form of this syndrome has its own certain symptoms. Signs of jaundice in children aged 3 years differ little from those in adults. But in a child, jaundice most often occurs against the background of hepatitis. To prevent children from getting this disease, compulsory vaccination is carried out in our country. Now let’s look at the symptoms for each form, and consider the signs of jaundice in a child (2 years and older).
You can understand that a baby has suprahepatic jaundice by the following indicators:
- Increased indirect bilirubin in the blood.
- The skin, sclera and mucous membranes become yellow with moderate pallor.
- The feces also change color and become dark brown.
- The liver and spleen increase in size. There may be pain in the left hypochondrium.
- Temperature increase.
- Whims, headaches, increased fatigue and increased heart rate in the child.
The second form of jaundice (hepatic) is characterized by the following symptoms:
- Bright orange tint of the skin and mucous membranes.
- Enlarged liver and spleen.
- Chills and fever.
- Lack of appetite in the baby.
- Nausea, headache.
- Apathy.
- Possible nosebleeds.
- Diarrhea.
This form of jaundice can be identified by the following signs:
- Dark colored urine with foam.
- Colorless stool with a lot of fatty acids.
- Increased levels of bilirubin and cholesterol in the blood.
Jaundice in a newborn
Approximately 60% of all newborns develop a specific skin color on average by day 3. Jaundice in infants is called physiological, since it does not signal any disease, but indicates a period of adaptation. This phenomenon is temporary and lasts no more than 10 days. So why does it occur and what are the main signs of jaundice in a newborn baby?
The fact is that when a child is in the womb, he has blood with special hemoglobin, which carries oxygen throughout the organs. When the baby begins to breathe through the lungs, his blood composition changes, special hemoglobin is destroyed and “live” is formed. This is where excess bilirubin appears, and the small body is not yet able to cope with it, so jaundice appears. Signs of this syndrome in young children are expressed only by jaundice of the sclera and skin, but otherwise the baby is quite normal condition. The liver and spleen are of normal size. In newborns, jaundice cannot be treated with medication, since the liver independently restores its function.
Treatment of jaundice comes down to determining the causes that caused it. For example, prehepatic jaundice, the symptoms of which in children were described above, is treated by stopping the breakdown of red blood cells. If jaundice is caused by liver destruction, then in this case drugs are used that can restore it. In the case of viral hepatitis, it is prescribed antiviral drugs. With more serious illnesses liver transplant is possible. And subhepatic jaundice, the symptoms of which in children were described above, can only be treated surgically.
Nutrition for jaundice
When treating a disease that causes jaundice, you must adhere to a certain diet. The essence of the nutritional principle will be to reduce the load on the liver and cleanse the bile ducts. Here is a list of foods that should be excluded from the diet during illness:
- Any broths and soups (fish, meat, chicken, mushroom).
- Any pickles, as well as pickled foods and canned goods.
- Chocolate and all products that contain cocoa.
- Smoked meats and deli meats.
- Cold drinks and ice cream.
- Spices and seasonings.
- Mushrooms.
- Sweet buns and fresh bread.
- Fruits and berries with sourness.
- Eggs (any kind).
- Legumes
- Vegetables: Radishes, radishes and spinach.
- Alcohol.
- Strong coffee and tea.
- And, of course, fatty and fried foods.
Yes, the list is impressive! Any violation can aggravate the situation, so you need to strictly adhere to this diet. After jaundice, you will have to eat this way for about 2 more weeks, otherwise there is a high risk of relapse of the disease.
Probably, at first glance, many people will think that they will have to go hungry. But that's not true. There is a list of allowed foods, from which it is quite possible to create a daily diet:
- All low fat dairy products.
- All cereals, pasta and vegetable dishes.
- Boiled meat (any kind).
- "Yesterday's" bread.
- Fruits.
- Butter (butter, sunflower).
- Weak tea and vegetable juice.
And finally, the food should be fresh and warm. Your attending physician will help you create a nutrition plan, depending on the severity of the disease.
Preventive measures
The simplest and most basic preventive method is to observe the rules of personal hygiene for both yourself and your child. Particular attention should be paid to the purity of food products. That is, all vegetables and fruits must be thoroughly washed. Be sure to teach your child to wash their hands before eating and after using the toilet. It is also necessary to avoid contact with other people's personal belongings, for example, do not use someone else's razor, comb, toothbrush, or nail scissors. These items may contain biological products from a sick person. Drink only boiled water. Try not to eat in street cafes. You can also become infected with the disease through certain procedures, for example, piercing, manicure, pedicure, tattooing. Therefore, carry out these manipulations only in trusted salons that have the appropriate certificates. And the surest and most effective way of prevention is vaccination.
Conclusion
The liver is a kind of filter in our body; it absorbs everything unnecessary and harmful. And when its function is impaired, the body is attacked by toxins and other harmful substances. If you notice external signs of jaundice in your baby or yourself, contact your doctor as soon as possible. Timely treatment will always ensure recovery. Do not be ill!
Jaundice or icteric syndrome is a visible change in the color of the baby's skin and sclera to yellow, which is caused by an increase in the level of bilirubin in the blood and tissues.
In most cases, icteric syndrome develops against the background of liver or biliary tract diseases.
Due to the fact that the main factor in the development of jaundice syndrome is damage to liver cells by hepatovirus, many call hepatitis jaundice. This is an erroneous, but popular name. In order to know what to do when icteric syndrome appears, you need to understand the causes of its occurrence, forms and manifestations.
Causes and mechanism of development of jaundice
With the physiological breakdown of red blood cells, indirect biliverdin is released, which is subsequently converted into free or indirect bilirubin. Then free bilirubin is captured by hepatocytes (functional liver cells) in which it binds with glucuronic acid, forming bound or direct bilirubin, which enters the intestine with bile and is excreted from the body by the digestive tract. A small part of the conjugated bilirubin is absorbed in the intestine and excreted in the urine.
The cause of the development of icteric syndrome is the appearance of disturbances in the cycle of formation and excretion of bilirubin, in which its concentration in the blood increases.
The reason for this situation may be:
the formation of too much bilirubin in the absence of disturbances in its excretion; impaired excretion of conjugated bilirubin at a normal rate of formation.
In most cases, the cause of the development of icteric syndrome is viral hepatitis of various types, which destroys liver cells and disrupts the binding of bilirubin, which causes a significant increase in its concentration in the blood.
Types of jaundice in a child
Depending on the concentration of bilirubin, we can talk about true and false jaundice syndrome; symptoms of jaundice in newborns are also distinguished.
False (keratin) jaundice
A condition in which the yellow color of the skin of the soles, palms and face is caused by eating large amounts of foods, medications or dietary supplements that contain carotene. The reason for the change in skin tone in this case is the accumulation of carotene derivatives in it. Products with a large amount of carotene include carrots, oranges, and pumpkin. This pathology develops in children aged from one to 2.5 years. And since the child was not sick with anything, treatment for false jaundice is not required, everything should be done - just reduce the amount of carotene in the diet.
True jaundice
True jaundice in children develops only when the concentration of bilirubin in the blood increases.
Depending on what stage of the cycle of elimination of this substance from the body the failure occurred, three forms of icteric syndrome can be distinguished:
Hemolytic (suprahepatic) - develops with increased formation of bilirubin. Parenchymal (liver) - in this form, the binding of free bilirubin in liver cells is impaired due to their damage caused by various diseases. Obstructive or subhepatic - also called mechanical and is associated with a violation of the excretion of the bound form.
With viral hepatitis, a parenchymal form of true jaundice develops, which in some situations can occur without a pronounced change in the color of the skin.
Jaundice syndrome in newborns (physiological jaundice)
Physiological infant jaundice develops in infants 2-3 days after birth; this condition is a sign of the baby’s adaptation to new living conditions. Jaundice syndrome occurs due to an immature enzyme system and impaired bilirubin metabolism. Changes in skin and sclera color are perhaps the only symptom that manifests this condition. Most often, such jaundice develops in premature babies; it is not transmitted to people around the child. No specific treatment is required; the unnatural coloring of the skin goes away on its own within 7-10 days. Jaundice in a one-month-old baby is not physiological; when it appears, you must immediately consult a doctor to identify the causes of the development of the pathology.
Types, routes of transmission and clinical picture of viral hepatitis
Currently, several hepatitis viruses have been discovered, but three of them are the most common: viruses type A, B, C, D, E.
Routes of transmission of viral hepatitis
Experts identify several routes of transmission of infection:
Fecal-oral – virus particles enter the child’s stool, microparticles of which can contaminate objects, the skin of the hands and the soil. The virus is transmitted by failure to follow hygiene rules, by using shared utensils, toys, personal hygiene items, by contact or playing with a carrier of the virus, or by eating unwashed vegetables or berries. Viral hepatitis A and E, also called dirty hands disease, are transmitted in this way. When a disease is diagnosed in one child from a group in a kindergarten, in most cases a quarantine is declared. Parenteral - infection occurs through contact with blood or other biological fluids (saliva, tears), during medical procedures, dental treatment, and surgical interventions. During breastfeeding, the hepatitis virus can enter the child's body if there are cracks or wounds on the mother's nipples or areola, and it is not contained in breast milk. The hepatitis B, C and D virus is transmitted parenterally. Vertical - transmission of the virus from mother to child during pregnancy (in utero) or the moment he is born, most often the type B virus is transmitted this way.
In order to create immunity against the hepatitis B virus, vaccination is done on the first day of the baby’s life, and revaccination is carried out according to a schedule for up to a year.
Clinical manifestations of various types of hepatitis
Depending on the type of virus, infants with an infectious inflammatory process have a different clinical picture of the disease. The course of each type of hepatitis manifests itself with varying intensity, which is determined by the severity of the inflammatory process, the age of the child and the state of his immune system.
Hepatitis type A
In 15 cases out of 100, infection occurs in a kindergarten, more often in those groups in which there are children under 3 years old who do not know how to use a potty. The disease caused by the type A virus spreads quickly and is characterized by a fairly mild course and a favorable outcome in most cases. The virus may not die for a long time in an open environment under favorable conditions; when boiled, it dies in 4-5 minutes. The period from infection until the first signs of the disease appear is called incubation; it can last from 7 days to 5 weeks.
Manifested by the following symptoms:
Symptoms of general intoxication of the body are the first signs of the disease - they appear even before the color of the skin changes. These include chills, increased body temperature, fever, headaches, weakness and fatigue, aching bones and muscles. Clinical manifestations from the digestive system develop during the first week of the disease - bitterness in the mouth, nausea, frequent vomiting, pain in the right hypochondrium, diarrhea (the stool becomes light, almost discolored), enlarged liver and spleen. Change in the color of urine - it takes on a shade from reddish-brick to brown, due to the high content of bilirubin that enters the urine from the blood. Skin symptoms appear at the beginning of the second week, gradually increase and begin to subside at 3-4 weeks of the disease. Manifestations from the skin include severe itching, which develops as a result of stagnation of bile, then a change in color of the sclera and oral mucosa appears, after which the skin turns yellow.
After the signs of jaundice disappear, the child will need at least six months to fully recover health. Hepatitis E virus manifests itself with symptoms similar to the clinical picture described above; laboratory diagnostic methods will help establish the correct diagnosis.
In infants, as well as during the first years of life, hepatitis A can occur without severe symptoms.
Depending on the totality of symptoms of the disease, several types can be distinguished:
icteric typical – the only symptom absent is itching of the skin; icteric form with a pronounced cholestatic component - the period of icteric syndrome is long and accompanied by skin itching; atypical icteric – a rare form of the disease, characterized by the absence of intoxication symptoms and severe severity of skin signs and itching, most cases are diagnosed in adolescent children; anicteric – there are no skin symptoms, the development of this form is indicated by weakness, pain in the right hypochondrium and lack of appetite; often diagnosed in an advanced form, since the symptoms are mild; subclinical - only an increase in the size of the liver can indicate the development of hepatitis; other signs are completely absent.
Hepatitis A causes the development of stable immunity - if a child has this disease even in the first months, he is protected from re-infection for life.
Hepatitis type B
Hepatitis type B is a disease transmitted parenterally or vertically. Jaundice syndrome in this form of pathology does not occur in all cases, but if it develops, it has pronounced manifestations.
Features of symptoms of acute hepatitis B:
sudden increase in body temperature to 38.5-39 degrees; the appearance of attacks of nausea and vomiting; severe pain in the right hypochondrium; significant increase in size and hardening of the liver.
With a long course, skin rashes may appear, nosebleeds may develop, menstruation is heavier than usual in girls, gingivitis (inflammation of the gums), damage to the spleen, pancreas, and bile ducts may occur.
If treatment is started untimely or prescribed incorrectly, the acute form of the disease turns into a more severe chronic form, which is characterized by long periods of remission followed by exacerbations. To prevent a child from getting hepatitis B, he is vaccinated while still in the maternity hospital in order to cause the development of immunity to this disease. Since the formation of immunity does not occur immediately, revaccination is carried out during the first years of life. To maintain immunity, starting from adolescence, it needs to be done every 5 years. In some cases, if there are medical exemptions before the age of one, vaccination against hepatitis B begins later; in any case, vaccination against this disease will protect the child from the possibility of becoming infected with it in the future.
Hepatitis type C
The most dangerous form of the disease, in most cases developing primarily chronic, and with acute hepatitis C in almost 80 cases out of 100 the disease becomes chronic. The virus is transmitted predominantly parenterally; infection of the child from the mother during pregnancy is observed in 5-6% of cases. The disease can occur typically (accompanied by icteric syndrome) or atypically (anicteric form).
Features of clinical manifestations:
feeling unwell for a long time; lethargy, chronic fatigue and weakness in the child; decreased appetite; in 20-35% of cases, icteric syndrome develops, lasting 7-21 days; significant increase in liver size (hepatomegaly).
In infants and young children, a predominantly atypical form of the disease develops, which often leads to the development of chronic pathology and fibrotic degeneration of the liver. The typical form of acute hepatitis C in childhood in most cases has a mild or moderate course. A severe and malignant (often fatal) course is extremely rare.
Methods for diagnosing hepatitis
The following laboratory methods are used to confirm the diagnosis:
blood biochemistry; study for markers for hepatitis; enzyme immunoassay of venous blood; PCR analysis; ultrasound examination of the liver; needle biopsy of the liver.
Hepatitis Treatment Methods
Treatment for any form of hepatitis can only be prescribed by a specialist; attempts to cure the disease at home without consulting a doctor (especially in infants) can lead to serious complications, including death.
First of all, when hepatitis develops, dietary nutrition is prescribed (table No. 5 according to Pevzner); if the disease is observed in infants, a change in diet will be suggested to the mother.
The following groups of drugs are prescribed:
hepatoprotectors; choleretic drugs; vitamin complexes; sorbents; interferons; medicinal mineral water (in case of illness in infants, the doctor will determine whether it can be consumed).
For infants and young children, the dosage and route of administration of drugs is determined individually.
For a speedy recovery of the child, parents must strictly follow all doctor’s recommendations regarding regimen, nutrition, medication and fluid intake. Treatment of this disease is always carried out in a hospital; after discharge, a child who has suffered from hepatitis remains under the supervision of a doctor on an outpatient basis for quite a long time. Features of monitoring patients with chronic forms of the disease consist of registration at a dispensary; in case of exacerbations, hospitalization is necessary, and after them sanatorium-resort treatment.
Gastroenterologists in your city
Select city:
To the question “What is hepatitis?” very often you can hear the answer: “jaundice.” However, a icteric tint of the skin is not yet an indicator of hepatitis; forms of the disease are erased and anicteric. The names of hepatitis viruses are similar to the alphabet – A, B, C…. Let's talk about hepatitis viruses and discuss the first signs of jaundice in a child.
Ways of transmission of infection:
fecal–oral– ingestion of particles of the patient’s secretions containing virus A with food through the mouth;
parenteral– through infected blood and biological fluids (saliva, tears, breast milk). Characteristic of hepatitis B and C viruses;
Botkin's disease - hepatitis A– dirty hands disease is the most common form of viral hepatitis, although it is the most favorable, and those who have recovered from this form of jaundice acquire long-term immunity. The hepatitis A virus lives for approximately 30 days at a temperature of +25 degrees in the external environment, and in water for 3-10 months. When boiled, it dies within 5 minutes.
The first signs of jaundice caused by the hepatitis A virus in a child:
The pre-icteric period lasts 5-7 days;
A sharp increase in body temperature;
The occurrence of weakness, headache, body aches;
Chills and fever;
Damage to the liver and gastrointestinal tract. Children complain of bitterness in the mouth, sharp pain in the right hypochondrium;
Deterioration of appetite, complete aversion to food may occur;
The appearance of diarrhea and vomiting;
With severe stagnation of bile, severe skin itching begins;
After 2-3 days, a change in the color of urine is noted, it becomes the color of beer or strong brewed tea;
Feces, on the contrary, become discolored.
Very young children may have minimal or no symptoms.
The icteric period is optional and lasts 7-15 days. First of all, the mucous membrane of the mouth turns yellow, then the sclera, and only then the skin. When jaundice appears in a child, intoxication subsides, but weakness and loss of appetite persist for a long time. The outcome of hepatitis A is favorable; in 90% of cases, complete recovery occurs within 3-4 weeks from the onset of the disease. The recovery period after illness is longer and ranges from 3 to 6 months.
Serum hepatitis – hepatitis B- a much more dangerous disease. The symptoms are very similar; in children, the infection is often asymptomatic; clear complaints arise only in adults.
The first signs of jaundice caused by the hepatitis B virus in a child:
The pre-icteric period lasts 7-12 days;
Increased body temperature;
The occurrence of nausea, vomiting;
Headache, joint pain;
Enlarged liver and spleen;
Skin rashes are possible.
The occurrence of jaundice in children with hepatitis B is not very common, but if it does exist, it is very pronounced; some children have bleeding gums and noses there's blood coming out. The duration of the jaundice period is 1-3 weeks. The recovery period lasts up to three months. Children often complain of weakness for a long time; they have an enlarged liver, damage to the biliary tract, and pancreas. These symptoms do not indicate the development of chronic hepatitis. With complete recovery, lasting lifelong immunity is developed. Erased, asymptomatic forms often become chronic.
The most insidious - hepatitis C– his virus “escapes” from the body’s defenses, constantly changing. This ability allows it to live in the body for many years, sometimes throughout a person’s life. With hepatitis C, more often than with other types, passive virus carriage occurs, during which the virus has a destructive effect on the liver without showing any external signs. Most patients with hepatitis C often experience the phenomenon of “imaginary recovery,” in which blood tests are normal for several weeks or months, and sometimes these periods are mistaken for recovery. You can get sick with hepatitis C again, even if treatment was successful, immunity to this hepatitis virus is not developed. Because of this, it is impossible to create a vaccine against hepatitis C.
The first signs of jaundice caused by the hepatitis C virus in a child:
Mild yellowing of the sclera;
Short-term darkening of urine;
Short-term lightening of stool.
Recovery from acute hepatitis C most often occurs with the icteric variant of the disease. In 80% of patients, hepatitis C becomes chronic.
Diagnosis of jaundice in children:
Biochemical blood test;
Blood test for antibodies;
PCR (polymerase chain reaction);
ELISA (enzyme-linked immunosorbent assay);
Ultrasound (ultrasound examination) of the abdominal organs;
Liver puncture biopsy.
Treatment of jaundice in children:
Bed rest before the onset of a “urinary crisis” is mandatory;
Diet is mandatory to adhere to during the acute period. Important in therapeutic nutrition are vegetable fats, products containing protein, having a lipotropic effect (oatmeal, cottage cheese, low-fat fish), easily digestible carbohydrates (honey, fruits, compotes, fruit drinks), fried, smoked, hot, spicy foods are strictly prohibited products;
The use of vitamins, active regulators of metabolic processes, vital activity of cells and tissues, is an important part of treatment. You should be careful when taking vitamin preparations to avoid allergic reactions; it is better to include more fruits and vegetables in your diet;
Use choleretic drugs only during the recovery period;
Prescribing enterosorbents to relieve symptoms of general intoxication, release toxic products from the gastrointestinal tract, enhance the evacuation of bile acids, and prevent their absorption in the intestine;
For hepatitis B, antiviral treatment is prescribed under medical supervision. Drugs that improve metabolic processes in liver cells are also used. After recovery from jaundice, the child is exempt from physical education for six months.
In contact with
Young mothers, while in the maternity hospital, are often faced with the fact that their baby develops infantile jaundice. Doctors are quick to reassure: jaundice in children, or more precisely in newborns, is a consequence of the immaturity of the liver enzyme system, which is not dangerous to the health and life of the child. But there are various shapes diseases that may appear for other reasons. Why they are dangerous, and what measures need to be taken in case of symptoms of jaundice in children in order to avoid complications - are detailed in this material.
What is jaundice
It’s worth starting with the fact that jaundice is not defined as a separate disease. This is a condition characterized by yellow discoloration of the skin, visible mucous membranes and sclera of the eyes. The cause of yellowing is the pigment substance bilirubin, which is formed during the breakdown of red blood cells and accumulates in tissues. Normally, it should be excreted from the body along with feces, thanks to the enzymes produced by the liver. But when, for a number of reasons, it fails to cope with its functions, the kidneys begin to remove excess bilirubin. Other organs also receive additional stress, and the skin becomes jaundiced.
Forms
Yellowing of the skin and sclera of the eyes may indicate one of the following violations: Either an excessive amount of bilirubin is released, or it does not have time to be eliminated from the body. Typically, the circulation of this substance is as follows: during the breakdown of red blood cells, indirect biliverdin is released, which turns into indirect (free) bilirubin, which is captured by liver cells, and it binds to glucuronic acid. After this, direct, that is, bound, bilirubin, along with bile, enters the intestines and leaves the body through it. At the last stage, it is partially absorbed back, after which it is excreted by the kidneys.
The sun don't shine
The form of jaundice in a child depends on at what stage in this chain the failure occurred. There are 3 forms:
- suprahepatic (hemolytic),
- hepatic (parechymatous),
- subhepatic (obstructive, or mechanical).
Suprahepatic form
Hemolytic jaundice occurs due to increased breakdown of red blood cells, resulting in the release of a large number of hemoglobin and, accordingly, the same amount of indirect bilirubin is formed. The liver cannot cope with its transformation into a straight line.
This form is often found in newborns. The liver itself does not suffer, and transaminases are normal.
Among the reasons for the development of this form of jaundice are hemolytic and pernicious anemia, sepsis, endocarditis, malaria, intoxication with drugs that provoke hemolysis, as well as transfusion of incompatible blood.
At hemolytic jaundice The baby exhibits the following symptoms:
TEST: What is the condition of your liver?
Take this test and find out if you have liver problems.
- moderate pallor of the skin and the appearance of jaundice on them, as well as on the sclera and mucous membranes;
- change in color of stool to dark brown;
- enlarged liver and spleen.
Blood tests record an increase in the level of reticulocytes (precursors of red blood cells) and a shortening of the lifespan of the red blood cells themselves.

Jaundice is not a disease, but a sign of liver problems
Hepatic form
In this case, icteric syndrome can be triggered by any pathological process occurring in the liver cells or biliary tract. The metabolism of bilirubin in the organ is disrupted, and the child develops one of the following types of jaundice.
Hepatocellular
It develops according to the following algorithm: the integrity of liver cells is disrupted, and bilirubin enters the extracellular space, after which it can only be excreted from the body in urine; and not with bile.
The hepatocellular form can be caused by:
- viral hepatitis;
- poisoning with certain chemicals;
- intolerance medicines;
- liver cirrhosis;
- infectious mononucleosis;
- leptospirosis.
Cholestatic
Occurs due to metabolic disturbances; components of bile and changes in the degree of permeability of bile capillaries. In the blood, the level of both types of bilirubin, bile acids and alkaline phosphatase. The elimination of bilirubin metabolites from the body does not occur or its rate is significantly reduced.
The causes of cholestatic jaundice are:
- cholestatic hepatitis;
- cirrhosis of the liver;
- taking certain medications.
Enzymopathic
It is a consequence of a deficiency of enzymes necessary for the normal metabolism of bilirubin. Her reasons:
- starvation;
- introduction special drugs during fluoroscopy;
- the presence of Gilbert-Meulengracht and Crigler-Najjar syndrome.
With enzymopathic jaundice, it is recorded in the blood increased level indirect bilirubin.

The main thing is to notice the symptoms in time
Subhepatic form
The first signs of the subhepatic form are:
- increasing jaundice;
- the presence of foam when urinating and a “beer” shade of urine;
- colorless feces with a clayey consistency. Analysis shows high levels of fatty acids and soaps.
A blood test reveals high levels of cholesterol, bilirubin, bile acids and alkaline phosphatase.
A special form of icteric syndrome
This is carotene jaundice, which is otherwise called “false”. Its distinctive feature is the absence of yellowing of the eye sclera - only the skin on the palms and soles, as well as the tip of the nose, is colored. The reason for this condition is the predominance of foods high in carotene in the child’s diet: pumpkin, carrots, apricots, broccoli, tomatoes, etc. Therapy in this case consists of reducing the consumption of such foods.
Jaundice of newborns
3–4 days after birth, a fairly large number of babies develop icteric syndrome. Most often, physiological jaundice occurs (immaturity of liver enzyme systems), which, in the absence of pathologies, gradually disappears without any consequences.

Jaundice in newly born babies usually does not have negative health consequences.
Premature babies are more susceptible to jaundice syndrome. In addition, their general health suffers noticeably, to the point where blood transfusions become necessary. Already on the 5th – 6th day of a child’s life, the level of bilirubin in the body reaches its maximum value. Signs of jaundice are pronounced and remain so for 3-4 weeks. In severe cases, they are accompanied by swelling.
In addition to physiological, there is pathological jaundice, the causes of which are most often:
- incompatibility of blood groups or Rh factor of mother and baby;
- congenital diseases, including cytomegalovirus hepatitis and autoimmune hepatitis;
- premature birth;
- diabetes mellitus in the mother, including gestational;
- the presence of hemorrhages, even minor ones, in a newborn;
- blood from the nipples swallowed during breastfeeding;
- administration of certain medications to the woman in labor, for example, oxytocin, and to the child - antibiotics.
Treatment of jaundice in children involves treatment of diseases that cause yellowing of the skin. Physiological jaundice in newborns is treated with phototherapy: the wavelength of light from the lamps used breaks down bilirubin, and after 10–12 hours its derivatives are naturally eliminated from the body. Doctors recommend combining phototherapy with breastfeeding.
The most dangerous is infectious jaundice. Its common cause is viral hepatitis.

Children are the bravest patients
Hepatitis in children
Often accompanied by yellow discoloration of the skin and mucous membranes. But icteric syndrome is just external manifestation serious violations, characterizing the disease, or rather, a whole group of liver diseases that are viral in nature.
In terms of frequency, the acute form of viral hepatitis ranks third after intestinal infections and acute respiratory viral infections and is life-threatening. The same applies to chronic hepatitis, one of the ten most common causes of death in the world.
Hepatitis A is the most common among children and is transmitted as follows:
- through household items, toys and dirty hands– small children constantly “taste” all this;
- through water with insufficient degree of purification;
- through food if the person preparing it did not follow the rules of hygiene;
- by airborne droplets (not recognized by all scientists).
In the first year of life, thanks to innate immunity, hepatitis does not pose a danger to children. But then the protection disappears, and in the period from 2 to 10 years the child’s body becomes most susceptible to the disease. The risk of illness during this period is high due to children’s frequent violation of personal hygiene rules.
Course of the disease
Viral hepatitis A in children occurs cyclically; the following periods are distinguished in its development:
- virus incubation;
- pre-icteric period;
- icteric period;
- recovery.
The typical course of the disease is the icteric form, the atypical form is anicteric, latent and erased. According to the severity, hepatitis is divided into mild, moderate, severe and malignant, and according to duration - into acute, protracted and chronic.
The incubation period for hepatitis A usually lasts from 2 to 4 weeks.

Mom always feels when something is wrong
Symptoms of hepatitis in children
Symptoms during the pre-icteric period depend on the type of its course:
- the influenza-like type is characterized by fever, weakness, lack of appetite, nasal congestion and cough, and nosebleeds. It is not uncommon for a doctor in such a situation to diagnose ARVI.
- gastric type is different painful sensations in the epigastric region and under the ribs on the right side, lack of appetite, nausea, and in some cases, vomiting. Adults often mistake this for food poisoning.
- The asthenovegetative type is characterized by drowsiness, fatigue, weakness, decreased appetite and frequent headaches.
- with arthralgic syndrome, complaints of pain in the joints are recorded, and sometimes there are rashes on the skin. Thus, the pre-icteric period often occurs with viral hepatitis B.
After 2–4 weeks, the pre-icteric period turns into the icteric period, and the child begins to show the following signs of hepatitis A:
- the liver enlarges;
- urine has a dark tint;
- feces become light, like white clay;
- the skin and mucous membranes rapidly turn yellow. Jaundice reaches a peak and then quickly passes;
- symptoms of intoxication are practically not bothersome, with the exception of severe cases when it increases;
- the spleen enlarges;
- skin itching often occurs;
- sometimes the functioning of the central nervous system is disrupted (insomnia, nightmares), and the pulse decreases.
The period of jaundice in mild form lasts about 2 weeks, in severe form – about 1.5 months. Rarely does this period reach 3 months.

Anti-hepatitis injection is a mandatory procedure for every one-year-old child
Vaccination of children against hepatitis A
The hepatitis A vaccine is used both routinely and before the start of seasonal activity of the virus: in August or September. Immunization against hepatitis A is practiced in regions with high incidence rates (12 children and adolescents out of 1000).
Parents of infants are interested in what the vaccination schedule for the little ones is, where the injection is given, and what will happen if the vaccine gets wet. For children over 1 year of age, A is administered intramuscularly according to the standard vaccination schedule. If the vaccine against hepatitis B is to be administered at the same time, then the injections are made in different parts of the body. As a rule, children tolerate the drugs used well, and 95% of those vaccinated acquire immunity. It is not recommended to bathe the baby on the first day after the injection.
Possible consequences of the vaccine administration
Side effects from anti-hepatitis drugs occur in rare cases. The reaction can be expressed in the form of pain, hyperemia and swelling at the injection site. Fever, chills and allergic skin rashes may occur.
Contraindications
Anti-hepatitis A drugs are not administered when hypersensitivity to their components is proven.
Jaundice in children is not an independent pathology - it is always associated with a deviation in work internal organs responsible for the metabolism of bilirubin. Therefore, it is important to get diagnosed and begin treatment as early as possible.
Jaundice(icterus) - yellow discoloration of the mucous membranes, sclera and skin due to the accumulation of excess bilirubin in the blood. Absolutely anyone can get jaundice: both adults and children.
Jaundice can be caused by many diseases and they are all quite different. Jaundice is one of the characteristic symptoms liver diseases, as well as lesions of the biliary tract and disorders in the erythrocytopoiesis system.
The cause of any type of jaundice is an imbalance between the formation and excretion of bilirubin. There are suprahepatic (hemolytic), hepatic (parenchymal) and subhepatic (obstructive) jaundice.
If a person is diagnosed with jaundice, treatment is based on establishing its cause and eliminating the underlying disease, and not the consequence, which is a change in the color of the skin and mucous membranes.
Most often, jaundice is a sign of “unwashed hands” and contaminated foods that we eat. One of the most common causes of jaundice is hepatitis A, which can be found in water or on unwashed fruits and vegetables. Jaundice can be infected, but only that which occurs with hepatitis A or Botkin's disease. Infection can occur through a kiss or if you eat food from the same container with a person with hepatitis A. The hepatitis A virus can survive in water for about 3 months.
Most often, children become infected with jaundice due to hepatitis A, since it is difficult to force them to adhere to the rules of personal hygiene; the most common reason for the appearance of jaundice in them is eating food with dirty hands. This of course also applies to adults, but to a lesser extent. In other cases, diseases caused by jaundice are not transmitted from person to person. Obstructive jaundice - when jaundice occurs due to obstruction of the bile ducts, it appears due to disruptions in the functioning of the body, and accordingly it cannot be transmitted in any way. The same applies to problems with the destruction of red blood cells.
Symptoms of jaundice
The main symptom of jaundice is yellowing of the skin and mucous membranes, which is where the name “jaundice” comes from.
True jaundice is distinguished by a change in color not only of the skin, but also, for example, the sclera of the eyes and mucous membranes - while false jaundice, which develops as a result of excessive consumption of carotene, is characterized by selective yellowing of the skin. In addition, with true jaundice, darkening of the urine is observed, since part of the bilirubin is excreted by the kidneys, and discoloration of the stool, since bilirubin does not enter the intestines.
In chronic liver diseases, jaundice is combined with a variety of clinical manifestations:
- pain in the right hypochondrium,
- enlarged liver and spleen,
- nosebleeds,
- skin itching,
- periodic increase in temperature,
- signs of portal hypertension (varicose veins of the esophagus, stomach, hemorrhoidal veins, venous network on the front abdominal wall, ascites),
- anemia,
- leuko- and thrombocytopenia.
Treatment of jaundice
A patient with jaundice must be hospitalized as quickly as possible in order to clarify the diagnosis and conduct rational treatment.
Treatment of the underlying disease is very important and often of paramount importance, including surgery(for example, with obstructive jaundice).
Therapeutic measures aimed at reducing the intensity of jaundice are carried out, as a rule, in cases of Gilbert-Meulengracht, Crigler-Najjar syndromes, etc. In this case, enzyme-inducing substances are used that increase the activity of the endoplasmic reticulum of hepatocytes (benzonal, zixorine, phenobarbital). For cholestatic jaundice, drugs that bind bilirubin and bile acids in the intestine (cholestyramine) are prescribed. Hemosorption and lymphosorption are carried out.
Emergency care is primarily necessary for patients with toxic liver damage. It consists of immediately stopping the entry of a toxic substance into the body, quickly neutralizing and removing it. Patients with obstructive jaundice with severe pain are injected subcutaneously with 0.5-1 ml of a 0.1% solution of atropine sulfate and 1 ml of a 2% solution of papaverine. It is better to refrain from administering drugs of the morphine group so as not to increase the spasm of the sphincter of Oddi. Hospitalization of a patient with jaundice due to viral hepatitis should be carried out in the infectious diseases department.
A patient with obstructive jaundice is sent to a surgical hospital for examination and resolving the issue of surgical treatment. Patients with hemolytic jaundice with splenomegaly are sent for treatment to a therapeutic hospital. In chronic liver diseases, stable jaundice is prognostically unfavorable, as it is a sign functional failure liver. All patients with chronic liver diseases with persistent hepatocellular or cholestatic jaundice are advised to planned hospitalization to the therapeutic department.
Jaundice in children (newborns)
Jaundice in children, particularly in newborns, is observed much more often than in adults.
This is due to the fact that in newborns, especially premature infants, bilirubin metabolism is easily disrupted due to insufficient activity of the glucuronyl transferase enzyme.
Bilirubin metabolism may be disrupted by in different ways its formation, transformation and excretion, and therefore in the neonatal period conjugative, hemolytic, hepatic and obstructive jaundice are distinguished.
Conjugation jaundice in children
Conjugation jaundice is caused by a disruption in the process of converting indirect bilirubin into direct bilirubin due to reduced activity of the enzyme glucuronyltransferase. It is observed with physiol, hyperbilirubinemia of full-term and premature newborns (physiological jaundice), Gilbert-Meulengracht syndrome, with hypothyroidism, etc. General state with conjugation jaundice it is not affected. It is characterized by the accumulation of indirect bilirubin in the blood, normal content hemoglobin and red blood cells, the liver and spleen are not enlarged. The prognosis is favorable, with the exception of jaundice in premature infants with severe hyperbilirubinemia, when active therapy and, in some cases, replacement blood transfusion are often required.
Hemolytic jaundice in children
Hemolytic jaundice is associated with increased destruction of red blood cells under the influence of maternal antibodies (with incompatibility of the blood of mother and fetus according to the ABO system and the Rh factor), with a deficiency of red blood cell enzymes, as well as with a violation of the shape and structure of the red blood cell or the structure of hemoglobin. This type of jaundice is observed in hemolytic disease of the newborn, microspherocytic anemia of Minkowski-Choffard, thalassemia, and sickle cell anemia. Accumulation of indirect bilirubin in the blood, enlargement of the liver and spleen, and anemia are noted. In cases of severe hyperbilirubinemia, replacement blood transfusion is indicated.
The prognosis for impaired bilirubin metabolism in children, accompanied by jaundice, depends on the course of the underlying disease, as well as the degree of impairment of bilirubin metabolism. With a sharp increase in the level of indirect bilirubin in the blood of newborns - above 340 μmol (above 20 mg%) - and in the absence of active measures aimed at reducing it (replacement blood transfusion), brain damage is possible (bilirubin encephalopathy).
Obstructive jaundice
Mechanical (subhepatic) jaundice develops when there is an obstruction to the flow of bile from the bile ducts into the duodenum.
Obstructive jaundice is characterized by a gradual increase in yellowness of the skin. In rare cases, for example with the so-called valve stone of the common bile duct, jaundice appears and disappears. With obstructive jaundice, all the components of bile accumulate in the blood - bilirubin, cholesterol, bile acids, and the amount of alkaline phosphatase increases. Urine takes on the color of beer with bright yellow foam. The feces are discolored, have a clayey appearance, white-gray in color, contain a large amount of fatty acids and soaps, stercobilin is not detected. At first, as a rule, there is no significant impairment of functional liver tests.
Hemolytic jaundice
Hemolytic (prehepatic) jaundice is caused by increased breakdown of red blood cells or their immature precursors. The consequence of this is overeducation bilirubin, exceeding the ability of the liver to bind and excrete it, and an increase in the content of bilirubin not associated with glucuronic acid (free) in the blood, urobilin in the urine, and stercobilin in the feces. Bilirubin is usually absent in urine. At the same time, reticulocyte count and anemia are observed.
Causes of hemolytic jaundice
The main causes of hemolytic jaundice are hereditary and acquired hemolytic anemia. In addition, it can develop with B12 deficiency anemia ( pernicious anemia), erythropoietic porphyria, prolonged septic, heart attacks various organs(more often pulmonary infarctions), radiation sickness, etc., as well as in case of poisoning with poisons or substances that can cause hemolysis (arsenous hydrogen, trinitrophenol, phosphorus, sulfa drugs), during transfusions of incompatible blood, etc.
Symptoms of hemolytic jaundice
Hemolytic jaundice of various origins is characterized by a number of common symptoms that make it possible to distinguish it from other types of jaundice. These include:
- moderate yellowness of the mucous membranes, sclera and skin along with more or less pronounced pallor;
- an increase in the content of indirect (unconjugated) bilirubin in the blood serum (hyperbilirubinemia) outside of hemolytic crises, usually up to 34-50 µmol/l (2-3 mg%), and during periods of crises - up to 80 µmol (4.7 mg%) or more ;
- enlargement of the spleen and sometimes liver;
- hyperpigmented stool (dark brown);
- an increase in the number of reticulocytes in the blood and an increase in the production of red blood cells in the bone marrow;
- shortened lifespan of red blood cells.
Liver function tests with hemolytic jaundice change slightly.
Hepatic jaundice
Hepatic (parenchymal) jaundice is caused by a pathological process localized in the liver cells (hepatocytes) and (or) in the intrahepatic biliary tract. Hyperbilirubinemia is associated with disruption of various parts of the metabolism and transport of bilirubin within the liver. Depending on location pathological process There are three types of hepatic jaundice: hepatocellular, cholestatic and enzymopathic. Hepatocellular jaundice is one of the most common manifestations of acute and chronic liver damage.
Causes of hepatocellular jaundice
Its occurrence may be associated with leptospirosis, toxic liver damage ( alcohol intoxication, chemical poisoning substances, drug intolerance, etc.), chronic active hepatitis, liver cirrhosis (), hepatocellular cancer. The leading role in the development of hepatocellular jaundice is the disruption of the integrity of hepatocyte membranes and the release of bilirubin glucuronide into the liver sinusoids. The excretion of bilirubin into the intestines with this type of jaundice is reduced, and sometimes absent at the height of jaundice. The excretion of urobilin in urine and stercobilin in feces is reduced or absent. Bilirubin is excreted in the urine (bilirubinuria).
Causes of cholestatic jaundice
Cholestatic jaundice is more often observed with cholestatic hepatitis, primary biliary cirrhosis () and taking various medications, especially aminazine, chlorpropamide, testosterone, sulfonamides. The cause of this type of jaundice is a violation of the metabolism of bile components, as well as a change in the permeability of bile capillaries. There are increased levels of direct and indirect bilirubin in the blood serum, high levels of alkaline phosphatase and bile acids. The excretion of urobilinogen in urine and stercobilinogen in feces is reduced or absent.
Causes of enzymopathic jaundice
Enzymopathic jaundice is caused by a deficiency of enzymes responsible for the uptake, transport, binding to glucuronic acid and excretion of bilirubin from the hepatocyte. This type of jaundice is observed during prolonged fasting, sometimes after the administration of radiocontrast agents, radionuclide preparations and other substances that compete with bilirubin for uptake by the hepatocyte. More often, the primary link in the mechanism of development of enzymopathic jaundice is a violation of the binding of bilirubin to glucuronic acid in the smooth endoplasmic reticulum (Gilbert-Meulengracht, Crigler-Najjar syndromes, etc.). With enzymopathic jaundice, the content of indirect bilirubin in the blood increases.
Diagnosis of jaundice
Differential diagnosis of various jaundices presents significant difficulties. Much attention One should pay attention to the presence of a history of blood transfusions, contact with patients with infectious diseases, poisons, taking medications, prolonged (lasting months and years) itching of the skin (preceding jaundice), operations on the abdominal organs, abdominal pain, etc. In some cases distinguishing between different types of jaundice requires additional examination using instrumental methods.
Questions and answers on the topic "Jaundice"
Question:Hello! The child developed jaundice on the 3rd day after birth. We were discharged on the 5th day with bilirubin 220. GV. They didn’t take any medications, they just lay in the sun. At 1 month, the yellowness on the skin noticeably subsided: only the yellow head remained. And at 2 months we went to another pediatrician and we were told to get tested for bilirubin. The result is 33. We were prescribed Hepel. And the instructions say that when taken, the bilirubin level may increase. Is it worth giving it to a child? Or retake the test at 3 months.
Answer: Good afternoon Newborn babies often experience jaundice due to the immaturity of the liver and its functions, but in this case your child’s body coped with it on its own, because 33 µmol/l after 220 is very good. With breastfeeding, jaundice goes away faster, so continue to feed your baby. About homeopathic medicines there are many different opinions opposing each other, but they do not bring “harmful” effects if prescribed in accordance with the instructions. If the icteric tint of the skin decreases, then there is no need to inject a vein again at 3 months, the main thing is to be observed by a pediatrician in a timely manner.
Question:The child fell ill with Botkin's disease, i.e. jaundice. We always adhere to cleanliness, both in food and in everything else. What can such a disease be transmitted from?
Answer: Botkin's disease is infectious disease. Infection can occur through dirty hands and flies. Symptoms of the disease appear 20-45 days after infection.
Question:Hello! We were born on July 4th. We were already home on the 6th. came on the 10th district doctor. He said that we have jaundice and the child needs to be given holosas ( choleretic drug, 1 drop 3 times a day). Although at the maternity hospital they said everything would pass, this is a normal physiological phenomenon. So I don’t know whether to give it or not. Can it wait a while? I would like to know your opinion. Thank you
Answer: Not needed yet. This physiological state(provided that your child was born healthy) can last up to 2 weeks for the child. If after this period some manifestations remain, only then should the issue of prescribing treatment be decided, but certainly not with holosas.
Question:Good afternoon, my son is 10 months old. The doctor suspected jaundice due to the yellow color of the skin (the whites of the eyes were normal), and they donated blood for total bilirubin and ALT. Today I received the result, but the doctor went on vacation, please help me with the decoding. Total bilirubin - 5 µmol/l. Alanine aminotransferrase - 203.2 units/l. How do I understand ALT is not normal, what do these results mean and what should I do with my child? Thank you in advance.
Answer: ALT levels are indeed significantly elevated. You should take your child to another pediatrician as soon as possible. The cause of increased ALT levels may be liver damage (hepatitis, biliary tract pathology, viral infections). We do not recommend that you conduct examinations without the knowledge of your doctor - contact the doctor who prescribed biochemical analysis blood and continue the examination under his guidance.
Question:As a result of a blood group conflict, a newborn child was diagnosed with emolytic jaundice on the second day; why is it dangerous and is a favorable outcome possible?
Answer: Modern medicine has a number of treatments for hemolytic anemia of newborns caused by blood group conflict. The course of the disease is favorable - do not worry, after 1.5 - 2 weeks the child will be out of any danger.
Question:Good afternoon I am 21 years old. I'm on a fast. On the evening of the third day, the whites of the eyes turned yellow, and then the tongue also turned yellow. There are no more problems. On the fourth day I did a cleansing enema using an Esmarch mug. I know what to do and why the squirrels turned yellow.
Answer: Yellowing of the whites of the eyes is a sign of jaundice, which, as is known, usually indicates a dysfunction of the liver, but it is unlikely that in your case the cause of jaundice was fasting. What kind of fasting are you doing exactly? You have completely given up food or are eating something like vegetables. If you eat vegetables (for example, carrots), then this may be the reason for the yellowing of the whites of your eyes and tongue. If you haven't eaten carrots or other vegetables, consult a doctor. You need to undergo an examination to determine the cause of jaundice.
Question:A month ago I suffered from obstructive jaundice (I am 46 years old). Now the therapist, having examined my throat with a wooden stick, made a diagnosis - follicular tonsillitis. Temperature 36.6, no pain or complaints. I contacted you about a hepatitis vaccination. The doctor prescribed me the medicine amoxiclav, the instructions for which say: contraindications if there is a history of indications of cholestatic jaundice. Can I take this drug? I am preparing for surgery to remove my gallbladder. Thank you for your attention.
Answer: It is better for you to refrain from taking Amoxiclav and ask your doctor to replace it with another antibiotic.
Question:Hello! Please tell me, the whites of my eyes have turned yellow. I went to the doctor, they told me that I shouldn’t have come - everything is fine with me! The whites of the eyes turned yellow in the corners. This worries me a lot. Is there any way to get rid of this? I am 23 years old. Hepatitis vaccinations have been completed.
Answer: Due to the fact that the main reason for the yellow color of the whites of the eyes may be an increase in the level of bilirubin in the blood (however, the whites turn yellow completely, and not just in the corners of the eyes), we recommend that you take a blood test for bilirubin.
Question:Hello! We are one and a half months old, the yellowness of the skin does not go away, the sclera of the eyes are yellow. They donated blood from a vein: total bilirubin - 127.4; direct bilirubin - 11.7; ALT-32.9; AST-63.3.
Answer: In cases where newborn jaundice lasts longer than 2 weeks, it is considered pathological. Pathological jaundice of newborns requires special examination And urgent treatment, since unbound bilirubin has a neurotoxic effect and affects the child’s brain. The most common cause of pathological jaundice in newborns is hemolytic anemia, biliary atresia, etc. We recommend that you show your child to a pediatrician and hematologist as soon as possible.