Survey radiographic examination of the abdominal organs: an old technique, indispensable in modern medicine. What can be seen on an abdominal x-ray Abdominal x-ray with barium
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
What does an abdominal x-ray show?
Abdominal x-ray is a study with a long history of application. Its versatility lies in the fact that with just one image you can obtain certain information about the condition of all abdominal organs at once. Although the data obtained through the survey x-ray, may not be enough to establish an accurate diagnosis; with its help, an experienced doctor can prescribe the necessary treatment as early as possible. Thanks to plain X-rays, it is possible to save time that would otherwise be required for other, more accurate diagnostic procedures.Abdominal X-rays are used to examine the following organs:
- small and large intestines;
- gallbladder and bile ducts;
- spleen;
Stomach on abdominal x-ray
The stomach is mostly located on the left side of the midline. It has a hook or horn shape with medium filling. The shape of the stomach varies widely depending on its fullness and the state of motor function. Its volume in an adult is 1.5 - 3 liters. The stomach is successfully examined using x-ray methods. However, this requires filling it with a contrast agent. An x-ray can reveal the structure of the inner wall of the stomach and its division into sections.The following sections are distinguished in the stomach on an x-ray:
- cardiac part ( located near the esophagus);
- vault ( transition part);
- body ( main part of the stomach);
- pyloric region ( pyloric section, located near the duodenum).
Each section of the stomach is characterized by certain features of the folds of the mucous membrane. Thus, the folds of the arch have the greatest thickness ( up to 2 centimeters), and the smaller one - at the gatekeeper ( up to 5 mm). In the body of the stomach, the folds are about 1 centimeter thick. Visualization of the gastric folds may be obstructed by the envelopment of the gastric mucosa by protective mucus, fluid, or food debris.
Using X-rays, you can study the motor-evacuation function of the stomach. It is regulated by complex neural reflex mechanisms. Under the influence of peristaltic waves, the contents of the stomach move to the pylorus, but its removal into the duodenum depends on the opening of the pylorus. Usually after 30–40 minutes, half of the contrast mass leaves the stomach. After 1 - 3 hours, the stomach is almost completely cleared of it. To monitor this process, a series of x-rays are taken at large intervals.
X-ray anatomy of the small intestine
The small intestine is the longest section of the gastrointestinal tract. Its initial section, the duodenum, is of greatest importance, since digestive enzymes enter it and food is digested here. The entry of food into the duodenum reflexively depends on its fullness and acidity level. An x-ray uses a contrast suspension to highlight the internal contour of the small intestine, its folds and the width of the lumen.The small intestine has the following sections:
- Duodenum. At the beginning of the duodenum ( the so-called onion) folds are not visible, so on a normal x-ray it should be smooth. Then oblique, transverse, and longitudinal folds about 3 mm high appear. On x-ray, the wall of the duodenum has a mottled appearance. It is explained by the penetration of barium suspension into the spaces between the folds.
- Jejunum. It is the longest section of the small intestine. A characteristic anatomical feature is the transverse folds, located particularly densely in the jejunum. However, due to the small height of the folds, they are practically invisible on x-rays.
- Ileum. Has the smallest clearance. The folds in the ileum are larger in size than in the jejunum, so its serration resembles the duodenum. The ileum opens into the side of the large intestine.
X-ray picture of the large intestine is normal
The large intestine is examined on X-ray using irrigoscopy - rectal injection of barium suspension. The procedure is quite unpleasant, but it allows you to reliably detect inflammatory and tumor diseases of the large intestine. When the large intestine is tightly filled with barium, the fusiform relief of the large intestine is clearly visible - the so-called haustra ( folds), composed of a muscular and submucosal layer. Conventionally, the large intestine is divided into sections that have similar anatomical features.The large intestine consists of the following sections:
- Cecum. The initial section of the large intestine. It is 20 mm long and 15 mm in diameter. The haustra of the cecum are large but rare. The cecum is separated from the small intestine by the so-called ileocecal valve, which regulates the passage of food into the large intestine.
- Ascending colon. It has a slightly smaller diameter than the cecum. The length of the ascending colon is 60 mm, it is directed upward, which explains its name.
- Transverse colon. It runs from right to left in the retroperitoneal space and is 50 centimeters long.
- Descending colon. It runs parallel to the ascending colon and is distinguished by less pronounced haustra and vertical orientation of the mucosal folds. Has a length of 70 mm.
- Sigmoid colon. Has different shapes and sizes, wide clearance ( up to 30 mm).
- Rectum. It is the terminal portion of the large intestine and gastrointestinal tract.
Liver on abdominal x-ray is normal
The liver is located in the upper right part of the abdominal cavity, mostly covered by the costal arches. The liver is a parenchymal organ. This means that it is made entirely of functional fabric and has no cavities. The liver consists of hepatocytes ( cells of a special structure), united into slices. The liver is divided into two lobes ( right and left) and consists of 8 segments. Unfortunately, it is impossible to distinguish these structures using X-rays. The normal size of the liver is 9–11 cm along the midclavicular line and 8–9 cm along the midline.On an x-ray, the liver has the appearance of a uniform triangular shadow that stands out well against the background of the rest of the abdominal organs. The upper contour of the liver coincides with the contour of the diaphragm. The outer contour of the liver stands out against the background of fatty tissue and muscles of the anterior abdominal wall. The lower contour of the liver corresponds to its anterior edge during palpation, approximately parallel to the costal arch. With conventional x-rays, the intrahepatic ducts or vessels of the porta hepatis cannot be seen. Therefore, the capabilities of X-rays in studying the liver are limited and inferior to techniques such as ultrasound ( Ultrasound) or magnetic resonance imaging ( MRI) .
Gallbladder and biliary tract on abdominal x-ray
The gallbladder and bile ducts are not visible on a regular abdominal x-ray. An indirect sign of the gallbladder is a notch in the lower contour of the liver. A prerequisite for studying the biliary tract on x-ray is the use of contrast agents. When they are used, their lumen is completely colored, allowing you to see their anatomical structure.With a contrast X-ray of the gallbladder, it is determined in the form of an oval formation 6–10 cm long, 2–4 cm in diameter. Normally, it is filled with a contrast agent evenly, the contour of its internal walls is even and smooth. The volume of the gallbladder is 30 - 70 cubic centimeters. In response to food intake, its muscle wall contracts, and the organ is halved in size.
The bile ducts begin inside the liver. The left and right hepatic ducts depart from the lobes of the liver, which unite into the common hepatic duct. After joining the cystic duct, a common bile duct is formed, which flows into the duodenum. Regardless of the method of entry of the contrast agent into the bile ducts, they normally look the same on x-rays. Due to the high density of the contrast agent, the bile ducts appear bright white on x-rays.
The basis of a normal bile tree is the uniformity of its lumen, the absence of expansions or contractions. If the contrast agent does not penetrate certain areas, this indicates a mechanical reason for the closure of the lumen of the biliary tract. The diameter of the common hepatic duct on x-ray normally does not exceed 5 mm, and the common bile duct – 10 mm. The common bile duct has a length of 5 to 10 centimeters, and when it flows into the duodenum, it forms a physiological extension - the ampulla.
X-ray anatomy of the pancreas
The pancreas is an important organ of the digestive system. It secretes enzymes that allow it to digest proteins and carbohydrates. The pancreas is located in the retroperitoneal space, conditionally located between the right kidney and the spleen. The pancreas consists of a head, body and tail. The main pancreatic duct passes through the entire thickness of the pancreas, which opens into the wall of the duodenum.The pancreas is normally not visible on x-ray. This is due to the fact that its tissue completely transmits x-rays. On the contrary, only with certain diseases and changes in the tissue of the pancreas does it become visible on x-rays. This occurs when stones or calcifications are included in it ( deposition of calcium salts). In this regard, X-ray examination of the pancreas is rarely performed, in contrast to ultrasound examination of this organ.
When performing endoscopic retrograde cholangiopancreatography ( ERCP) a radiopaque substance is injected into the main pancreatic duct. This study allows you to see the lumen and walls of the duct. Normally, the diameter of the main pancreatic duct is from 1 mm ( in the tail area) up to 3 mm ( in the head area). Normally, its walls are smooth and do not have expansion or protrusion.
Anatomy of the kidneys. Kidneys on abdominal x-ray
The kidney is the main organ of the urinary system. The kidney filters the blood, purifying it from excess water, salts and metabolic products. The buds are bean-shaped and about 120 mm long. They are located in the retroperitoneal space, however, in terms of their location they correspond to the upper floor of the abdominal cavity. The kidney tissue is divided into the medulla and cortex, but this boundary can only be traced on x-ray using contrast techniques.On a plain X-ray of the abdominal area, the kidneys are identified as two bean-shaped shadows in the area of transition of the thoracic to lumbar spine. Part of the kidneys is covered by the lower ribs. The left kidney is located slightly higher than the right. It is not possible to determine the features of the internal structure of the kidneys using this research method. Due to anatomical features and insufficient contrast of the equipment, the kidneys may not be visible on a plain x-ray. However, in any case, it can be used to detect stones or foreign bodies.
The shadow of the kidneys with excretory urography is more contrasting. The main advantage of this method is the display of the collecting system. Typically three calyxes can be found ( top, middle and bottom), which flow into one larger pelvis. The size and shape of the cups and pelvis can vary. The ureters look like a shadow in the form of a narrow strip.
Normally, the following image characteristics are noted on excretory urography:
- clear contours of the collecting system, ureters, bladder;
- uniform and symmetrical release of contrast agent;
- The renal collecting system has no bulges, the diameter of the calyces is no more than 5 mm, and the diameter of the pelvis is no more than 20 mm.
What diseases can be detected using an abdominal x-ray?
 X-ray imaging has a very long history of use. Today, there are a large number of X-ray examination techniques adapted for specific organs. Each technique has its own set of indications. By combining all x-ray examination options together, you can significantly expand the list of indications. Thus, using X-ray methods it is possible to diagnose almost any disease of the abdominal organs. However, at the same time, a survey X-ray of the abdominal cavity is not universal, this is its main drawback.
X-ray imaging has a very long history of use. Today, there are a large number of X-ray examination techniques adapted for specific organs. Each technique has its own set of indications. By combining all x-ray examination options together, you can significantly expand the list of indications. Thus, using X-ray methods it is possible to diagnose almost any disease of the abdominal organs. However, at the same time, a survey X-ray of the abdominal cavity is not universal, this is its main drawback. Stomach diseases on abdominal x-ray. Chronic gastritis. Peptic ulcer
Radiation examination of the stomach is often indicated. This is due to the fact that due to malnutrition of modern man, the stomach and digestive tract as a whole suffer to a large extent.If abdominal pain, heartburn, or malnutrition occurs, a diagnosis of peptic ulcer or chronic gastritis is assumed. To diagnose them, it is necessary to take an x-ray using a barium suspension.
Chronic gastritis in most cases is characterized by an increase in folds, acquiring sizes of 3–5 mm, limited by deep grooves. Gastric fields ( clusters of folds) because of this they become clearly distinguishable. At the same time, functional disorders of the stomach are detected. With an exacerbation of chronic gastritis, the stomach is reduced in size due to tonic contraction, and its peristalsis is increased. Abdominal pain occurs due to muscle spasms. Using X-rays, you can distinguish several types of chronic gastritis.
On X-ray, the following variants of chronic gastritis are distinguished:
- Warty ( polyposis) gastritis. X-rays reveal thickening of the folds of the mucous membrane in the form of polyps. This variant of chronic gastritis occurs most often. Increased folds of the mucous membrane ( hypertrophy) is a protective reaction to inflammation or irritants.
- Atrophic gastritis. X-rays show thinning of the gastric mucosa. The wall of the stomach has reduced tone, there is a small amount of fluid in it.
- Sclerosing ( rigid) gastritis. With this disease, the outlet section of the stomach is affected. The mucous membrane here thickens unevenly, acquires a jagged outline on x-ray, at the same time, the outlet section of the stomach decreases in diameter and becomes immobile.
Signs of an ulcer on an abdominal x-ray are:
- "Niche" symptom. It is a contrasting depression in the wall of the stomach. The recess has smooth edges and a rounded shape. It is surrounded by a raised shaft, to which folds of the mucous membrane converge concentrically.
- Deformation of the stomach wall. With a long-term ulcerative process, scarring occurs in the gastric mucosa - the replacement of epithelial tissue with connective tissue. It tightens the edges of the ulcer, causing the stomach to become deformed and take on an irregular shape.
- Violation of the tonic and motor functions of the stomach. They are observed mainly locally, in the area of the ulcerative defect. In this case, at the site of the ulcer there is a decreased tone of the stomach wall, as well as a slowdown or complete absence of peristaltic waves.
Free gas on abdominal x-ray
The reason for the appearance of gas in the abdominal cavity is a violation of the integrity of the wall of a hollow organ. X-ray examination plays an important role in diagnosing complications of gastric and duodenal ulcers. One of the most serious complications of peptic ulcer disease is rupture of the stomach wall. This condition requires urgent medical attention. When an ulcer perforates into the abdominal cavity, free gas is found in it.If a perforation of an ulcer is suspected, an x-ray examination is carried out in the position in which the patient was taken to the x-ray room. The gas enters the abdominal cavity through an opening in the wall of the stomach. On radiographs it forms a clearly visible clearing. The gas occupies the uppermost sections of the abdominal cavity, and it changes its location depending on the person’s posture. It can be located under the diaphragm, under the anterior abdominal wall, or in the lateral sections of the abdominal cavity. Therefore, when perforation of the abdominal cavity occurs, the gas is called free.
Upon penetration ( penetration of the ulcer into neighboring organs) certain radiological signs are revealed. Ulcerative defect ( niche) has large dimensions ( a few centimeters). The ulcer is fixed; it does not move when palpating the stomach or changing body position. To treat the penetration of an ulcer, a surgical operation is required, during which the ulcerative defect is sutured.
Fluid on abdominal x-ray
Free fluid in the abdominal cavity, like gas, appears only as a result of pathological processes. However, fluid can appear in the abdominal cavity for several reasons. It is very important to establish the exact cause through a thorough examination, since the quality of medical care depends on this. If free fluid in the abdominal cavity is detected on an x-ray, it is necessary, first of all, to eliminate the cause of its appearance. Only after this is the fluid removed from the abdominal cavity using puncture and drainage.Free fluid appears in the abdominal cavity for the following reasons:
- Abdominal trauma. When various organs are injured, intra-abdominal bleeding occurs. At the same time, the person’s condition does not change until a certain moment. After the loss of a quarter of circulating blood, blood pressure drops sharply and cerebral circulation decreases.
- Ascites. It is the release of fluid into the abdominal cavity through the wall of the veins as a result of stagnation of blood flow. Ascites is observed in heart failure and liver failure, kidney disease. With cirrhosis of the liver, dilation of the veins of the anterior abdominal wall is also observed, reminiscent of the “head of a jellyfish”. The fluid from ascites is usually sterile and free of bacteria.
- Perforation of hollow organs. When the gallbladder ruptures, gastric ulcer or duodenal ulcer occurs, their contents may enter the free abdominal cavity. In this case, acute pain occurs, caused not only by rupture of the wall of the hollow organ, but also by irritation of the peritoneum.
- Peritonitis. It is an inflammation of the peritoneum as a result of bile, blood, pus entering the abdominal cavity, and infection of ascitic fluid. Peritonitis is a complication of various purulent diseases, such as appendicitis. Peritonitis requires surgical treatment, as it can be quickly fatal due to the proliferation of pathogenic microorganisms.
Acute mechanical intestinal obstruction on abdominal x-ray
Typically, intestinal diseases are diagnosed on X-ray only with the use of contrast agents. However, if intestinal obstruction is suspected, a regular x-ray is taken, without their use. The fact is that additional introduction of a contrast agent into the gastrointestinal tract can aggravate the situation. With acute intestinal obstruction, paroxysmal pain, severe bloating and vomiting appear. Acute intestinal obstruction is an emergency.In acute intestinal obstruction, an x-ray reveals swelling of the intestinal loops above the blockage and emptying of the intestine below this area. A sign of mechanical obstruction on x-ray is the so-called Kloiber cups. They represent the fluid levels in the loops located above the site of intestinal blockage. Kloiber's cups are detected within an hour after the onset of intestinal obstruction. Rapid progression of this condition can be fatal.
Among intestinal diseases, the following pathologies are most common:
- Crohn's disease and others.
Crohn's disease is an inflammatory bowel disease of immunological nature. Crohn's disease manifests itself with the same symptoms as enterocolitis - abdominal pain, prolonged diarrhea ( diarrhea), loss of appetite, weakness. With this disease, any part of the intestine can be affected, but more often the initial part of the large intestine and the final part of the small intestine are affected.
The main sign of Crohn's disease on x-ray is narrowing of the intestinal loops with the formation of cicatricial constrictions. This area looks like a narrow, uneven channel ( "cord symptom"). The folds of the mucous membrane disappear, cracks and slit-like ulcers appear between them. The contrast agent penetrates into these spaces. When viewed, such a wall resembles the appearance of a “cobblestone street.” A complication of Crohn's disease is the appearance of abscesses. They are drained under the control of an ultrasonic sensor.
Appendicitis on abdominal x-ray
Appendicitis is an acute inflammation of the appendix, located at the initial part of the large intestine. It is known that appendicitis manifests itself as pain in the right lower abdomen. Its diagnosis is usually not difficult, but in unclear cases they resort to radiation diagnostic methods. Most often, they begin with the use of ultrasound and, if necessary, an x-ray of the abdominal cavity.On x-ray, acute appendicitis leads to thickening of the colon, the appearance of gas and liquid in it. The accumulation of gas looks like a clearing against the background of the wall of the large intestine. The folds of the mucous membrane are thickened and rigid, their mobility is reduced. There may be stones in the appendix that appear light on x-ray. An abscess at the site of the appendix looks like a darkening and depression on the wall of the cecum. When the appendix ruptures, there may be small amounts of gas or liquid in the abdomen.
Diagnosis of liver diseases using abdominal x-ray
Liver diseases are the subject of study by doctors of various specialties. For correct diagnosis, in addition to a clinical examination, a blood test and radiological data are also required. Diseases of parenchymal organs are usually diagnosed using X-ray only at a late stage. A more accurate test for diagnosing liver diseases is ultrasound.An abdominal x-ray can reveal diffuse or local changes in the liver. Unfortunately, they are not specific, that is, they cannot be used to establish an accurate diagnosis with certainty. With hepatitis, X-rays show an increase in the size of the liver and slight heterogeneity of the organ parenchyma. With fatty hepatosis ( a large number of fatty inclusions in the liver cells) the liver on x-ray is characterized by low density.
Changes in liver cirrhosis are much more pronounced. Cirrhosis is the final condition of the liver, which is caused by various chronic diseases. Cirrhosis manifests itself as scarring of the organ and functional failure. X-rays show a decrease in the size of the liver, deformation of its lobes, and jagged contour. In liver tissue, heterogeneity is even more pronounced than in hepatitis. At the same time, the spleen is enlarged. Free fluid may be detected in the abdominal cavity - a sign of ascites.
Focal changes in the liver on x-ray include:
- cysts ( fluid-filled cavities);
- abscesses ( accumulations of pus);
- tumors ( accumulations of cells atypical for the liver).
Diseases of the gallbladder and biliary tract. Gallstone disease on abdominal x-ray
Biliary tract diseases occur in a very large percentage of the population ( about 10%). Only in rare cases do they require surgical treatment. But, unfortunately, these diseases force you to limit your diet, primarily excluding fatty foods and alcohol. The first method for diagnosing the biliary tract is ultrasound ( Ultrasound). In cases where ultrasound is ineffective, special X-ray research methods using contrast are used.The most common diseases of the gallbladder and biliary tract are the following:
- acute and chronic cholecystitis;
- gallbladder damage;
- tumors.
One of the main symptoms of bile duct damage is jaundice of the skin. This symptom can become a complication of gallstone disease. Obstructive jaundice is the closure of the lumen of the bile ducts by various formations located inside or outside them. For obstructive jaundice, the use of cholangiography and cholegraphy is a valuable way to determine the cause of its occurrence.
Indirect signs of acute pancreatitis on a plain radiograph of the abdominal cavity are:
- focal clearings in the pancreas area, corresponding to gas bubbles;
- symptom of “cut-off colon” ( distension of the transverse colon to the beginning of the descending colon);
- increase in the size of the pancreas.
The best methods for diagnosing pancreatic diseases are ultrasound, magnetic resonance imaging and computed tomography. Using these methods, it is possible to pay closer attention to the internal structure of the organ, which cannot be examined using a regular abdominal x-ray.
Kidney disease on abdominal x-ray
Kidney diseases are very diverse. To diagnose them, doctors use various diagnostic methods, each of which serves a specific purpose. For example, for diseases of the kidney vessels, angiography is required, for chronic pyelonephritis, excretory urography is required, and to identify kidney stones, a survey x-ray of the abdominal cavity may be sufficient. In controversial cases, computer or magnetic resonance imaging can be used.The most acute condition that requires an abdominal x-ray is renal colic. During renal colic, sharp pain in the lower back and difficulty urinating appear. Renal colic is a complication of urolithiasis and is caused by a stone blocking the urinary tract. In the vast majority of cases, kidney stones are composed of calcium and phosphate, which makes them visible on x-rays. A survey x-ray can determine its presence or absence. Using excretory urography, you can determine the exact position of the stone relative to the ureters or pyelocaliceal system.
In case of urolithiasis, the following signs are revealed using X-ray methods:
- presence of kidney stones ( contrast shading);
- expansion of the pyelocaliceal system;
- the sign of a “large white kidney” is an increase in the size of the kidneys and an increase in its contrast on a plain radiograph.
Sometimes x-rays can reveal a decrease in kidney size ( less than 10 centimeters in length). This sign is considered an unfavorable change. Kidneys shrink during long-term chronic diseases ( glomerulonephritis or pyelonephritis). This condition is called nephrosclerosis. Along with a decrease in size, the kidney becomes less functional, which threatens to increase blood pressure and intoxicate the body with its own metabolic products.
Almost any renal vascular disease can be detected using angiography. On an X-ray with good image quality, they are determined by narrowing or dilation of the renal vessels at various levels. Changes in the renal artery are called renovascular pathology. In chronic glomerulonephritis or pyelonephritis, the vessels inside the kidneys are affected. This form is called parenchymal. The basis for angiography is unexplained elevated blood pressure ( the lower value is more than 110 mmHg. Art.).
Using angiography, the following diseases of the kidneys and renal vessels can be determined:
- atherosclerosis, renal artery thrombosis;
- chronic glomerulonephritis and pyelonephritis;
- renal arterial hypertension;
- congenital disorders of renal vascular development;
- kidney tumors ( especially malignant).
Where can I get an abdominal x-ray?
 A routine abdominal x-ray can be performed at any medical facility that has an x-ray room. This can be either a public or private diagnostic and treatment center. However, for more complex X-ray techniques ( such as cholecystography, urography) specialized medical personnel are required. They are usually carried out in medical centers of the appropriate profile.
A routine abdominal x-ray can be performed at any medical facility that has an x-ray room. This can be either a public or private diagnostic and treatment center. However, for more complex X-ray techniques ( such as cholecystography, urography) specialized medical personnel are required. They are usually carried out in medical centers of the appropriate profile. Make an appointment for an abdominal x-ray.
To make an appointment with a doctor or diagnostics, you just need to call a single phone number
+7 495 488-20-52 in Moscow
+7 812 416-38-96 in St. Petersburg
The operator will listen to you and redirect the call to the desired clinic, or accept an order for an appointment with the specialist you need.
In Moscow
In St. Petersburg
X-rays are actively used to diagnose diseases of the abdominal organs. Plain radiography of the abdominal cavity is widely used - an X-ray examination without the introduction of a contrast agent, which allows one to obtain a general picture of the condition of the abdominal cavity.
Abdominal organs: general information
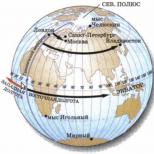
The abdominal cavity is the abdominal cavity, which is limited above by the diaphragm, in front by the abdominal wall, behind by the lumbar spine, on the sides by the abdominal muscles, below by the ilia and the pelvic diaphragm. Inside the abdominal cavity are the organs of the digestive system - the stomach, gall bladder, liver, intestines, pancreas, as well as the spleen and organs of the urinary system - kidneys and ureters.
Examination of the pancreas, gallbladder, liver and spleen is usually carried out using methods that turn out to be the most informative for these organs. To examine the remaining organs of the abdominal cavity, predominantly other diagnostic methods are used, including radiography.
What does an abdominal x-ray show?
The method is based on the fact that tissues of different densities absorb X-rays differently. Denser, for example, bone tissue transmits rays less well, so in the picture such tissue appears lighter. The method allows you to determine the location of organs, their integrity, the presence of foreign bodies and neoplasms.
An abdominal x-ray shows:
- how gas and liquid are distributed in the abdominal cavity, whether there is free fluid in the abdominal cavity;
- whether there are foreign bodies in the abdominal cavity (swallowed objects in the intestines, gallstones, kidney stones);
- whether there is damage to internal organs;
- whether there is intra-abdominal bleeding.
 From the point of view of assessing the condition of specific organs, plain radiography of the abdominal cavity is not very informative, but it allows you to quickly determine whether the picture is pathological or not. If the wall of the stomach or intestines ruptures (perforation of an ulcer or destruction of the wall by a tumor), an x-ray will show gas escaping into the free abdominal cavity. Using an abdominal x-ray, you can diagnose intestinal obstruction and even determine the approximate location of the problem.
From the point of view of assessing the condition of specific organs, plain radiography of the abdominal cavity is not very informative, but it allows you to quickly determine whether the picture is pathological or not. If the wall of the stomach or intestines ruptures (perforation of an ulcer or destruction of the wall by a tumor), an x-ray will show gas escaping into the free abdominal cavity. Using an abdominal x-ray, you can diagnose intestinal obstruction and even determine the approximate location of the problem.
When is an abdominal x-ray prescribed?
A survey radiography of the abdominal cavity is prescribed if there are severe complaints. Similar pain can occur with the following diseases:
- appendicitis;
- abscesses and inflammatory diseases of the abdominal organs;
- tumor processes;
- intestinal ischemia;
- intestinal obstruction;
- intestinal volvulus.
Plain radiography of the abdominal cavity is also prescribed for abdominal injuries.
How is an abdominal x-ray performed?
No special preparation is required for a plain abdominal x-ray.
Radiography can be performed in both one and two projections (in standing and lying positions). Sometimes it is enough to take an X-ray only in a standing position (this position allows you to better localize the problem of intestinal obstruction, as well as see a perforation of the stomach or intestines).
Before the examination, it is necessary to remove metal objects (jewelry). There is no need to take off your clothes. During the x-ray, you will need to stand still for some time, and hold your breath while the picture is taken.
Internal organs under X-rays are not characterized by high information content. Parenchymal and air tissues do not reflect radiation, therefore a clear picture is not visualized on radiographs. To detect the pathology of hollow structures and low-density formations, they need to be completely contrasted (injected with a contrast agent).
What is plain abdominal radiography?
A plain X-ray of the abdomen shows x-ray contrast of stones in the gallbladder, urinary tract, kidneys and colon. In case of perforation (destruction of the intestinal wall), the study can detect free gas under the right dome of the diaphragm and fluid levels in the lower abdominal cavity, as well as the pelvis. Plain X-ray of the abdomen shows:
- large tumors;
- feces;
- intestinal obstruction (bowls and arches of Kloiber).
The examination is not preventive and is not prescribed for every patient. An X-ray of the abdomen is performed if there is a suspicion of intestinal obstruction, perforation of the intestinal wall, or for lower back pain.
What is the passage of barium through the intestines?
The passage of barium through the intestines is carried out if an intestinal need is suspected, but before the procedure, perforation (destruction of the wall with the release of air) of the gastrointestinal tract should be excluded using FGDS.
Photo of the radiograph 6 hours after taking barium: Kloiber's cups are traced (marked by arrows) in acute intestinal obstruction
Attention! Passage with barium through the intestines when the intestinal wall is destroyed is contraindicated. Barium sulfate is a water-insoluble contrast agent. Its entry into the peritoneum will contribute to the development of peritonitis (inflammation of the peritoneum).
The technique involves oral (by mouth) administration of a contrast agent and taking pictures after 1, 3, 6, 9, 12 and 24 hours. At these intervals, the contrast moves to different parts of the gastrointestinal tract:
- After 1 hour - contrast agent in the small intestine.
- 3 hours - barium accumulates in the transition area between the small and large intestines.
- 6 o’clock – initial sections of the ascending colon.
- 9 o’clock – transverse and colon.
- 12 o’clock – descending colon and sigmoid colon.
- 24 hours – rectum.
A barium passage through the intestines shows:
- narrowing of the lumen of the gastrointestinal tract;
- difficulties in its advancement during blocking;
- intestinal obstruction;
- small bowel fistulas.
Let us remind you that an X-ray of the abdominal organs without a contrast agent is not very informative. But it perfectly shows an emergency condition - acute intestinal obstruction, in which free gas is visible under the dome of the diaphragm (the “sickle” symptom). If such signs are detected, urgent surgical intervention is necessary to identify the causes of perforation (perforation).
When is a plain radiography of the abdominal organs done with contrast?
Survey radiography of the abdominal organs is done for the following diseases:
- pancreatitis - inflammation of the pancreas;
- cholecystitis – inflammatory changes in the gallbladder;
- abscess - a purulent cavity;
- urolithiasis, nephrolithiasis – stones in the kidneys and urinary tract;
- intussusception - twisting of the intestine around an axis;
- blockage of the lumen by a tumor;
- diverticulitis;
- traumatic injuries;
- stomach pain.
For these diseases, a survey x-ray of the abdominal organs is first performed. This requires preliminary preparation. It involves a cleansing enema 2 hours before the procedure.
After a survey image is taken and in the absence of X-ray signs of perforation of the intestinal wall, organs are contrasted with oral barium.
Attention! During a contrast study of the abdomen and large intestine (irrigoscopy), the contrast is administered through the rectum.
Method of passage with barium through the gastrointestinal tract
 Virtual endoscopy: spastic contractions of the large intestine during colitis
Virtual endoscopy: spastic contractions of the large intestine during colitis The passage technique is highly informative for studying the small intestine. This part of the abdominal cavity has many anatomical formations, bends, anatomical narrowings, tumors, areas of impaired motility and secretory activity.
To study all parts of the small intestine, it is necessary to perform targeted radiographs every 30-60 minutes. As a result, it is accompanied by significant radiation exposure to the patient.
As barium moves into the abdominal cavity, the structure of various sections can be studied. When the cecum is visible on the X-ray image during the passage with barium, the study is stopped so as not to further irradiate the patient.
If there is pain in the abdominal wall, as well as symptoms of tension in the abdominal cavity, radiography can be continued to study the condition of the large intestine. True, it should be planned in advance in order to thoroughly cleanse the gastrointestinal tract (activated carbon, fortrans). 1-2 days before the procedure, the person is prescribed a slag-free diet.
Preparing for contrast radiography of the abdomen
How to prepare for a plain radiography of the abdominal cavity with subsequent contrast:
- In 2-3 days you should give up dairy products, brown bread, coffee, spicy foods, chocolate, alcohol and smoking.
- You can eat butter, white bread, pasta, fish.
- On the day of the procedure, the stomach should be empty. To do this, refrain from eating, smoking, and chewing gum.
To eliminate slag accumulations in the intestines, some doctors recommend the drug fortrans. It can be purchased at a pharmacy. Before use, the sachet of the product is diluted with a liter of boiled water. Fortrans is applied in the evening at intervals of 1 hour until the dosage recommended by the doctor is completed.
X-rays of internal organs are performed if dangerous conditions are suspected. If your doctor has prescribed a test, you should not refuse it. A barium passage can save a life!
The use of a contrast agent for examining the gastrointestinal tract and preparation for the examination require professional skills. To obtain high-quality images, you need not only the ability to schedule X-rays. It is important to prepare the barium correctly. This substance is diluted with water, but is not water soluble. Depending on the density of the suspension, an X-ray image is obtained. To examine the small intestine, located near the bauhinian valve (small intestinal junction), it is necessary to prepare a low-density solution.
A diagnostic method such as radiography has been used in medicine for quite some time. Today, thanks to improvements in the quality of equipment, the speed of image acquisition, and the absence of the process of developing images, this diagnostic method has become effective, accurate and relatively safe.
Concept and types
The method is named after its inventor (Wilhelm Roentgen) and the Greek. gráphō – food. It refers to non-invasive medical research, and is based on the projection of X-rays onto paper or special film.
The rays, passing through the anatomical structures of the body, give an image in the form of light and shadow, weakened in those places where the structure of the organ is more dense.
In modern (digital) devices, the resulting image can be recorded on a cassette with a special film or on the matrix of an electronic device. Subsequently, the film can be printed, or the image is stored in a database and displayed on the monitor if necessary.
Before proceeding with a detailed examination, a survey fluoroscopy of the abdominal and thoracic organs is performed. If survey fluoroscopy cannot provide a complete picture of the examination, then they resort to a contrast procedure using barium mass.
Contrast radiography
During X-ray examination of the gastrointestinal tract, an aqueous suspension of barium is used as a contrast agent. The solution is drunk by the patient or, in some situations, administered through a tube.
Barium is almost insoluble in water and physiological fluids, but has the ability to absorb X-rays, which makes it possible to judge the relief of the mucous membrane
While the barium mass moves through the digestive organs, its progress is monitored using transillumination. In this case, the radiologist examines the function of the intestine and identifies the presence of tumors, obstruction or damage.
Overview
Survey radiography allows one to judge the condition of the organs adjacent to the esophagus, stomach, and other organs of the gastrointestinal tract.
The abdominal organs have a less dense structure, so the shadow in the image is less pronounced than that of the bones. But a survey examination allows you to see the presence of foreign objects or changes in any organ due to injury or illness.
This examination is prescribed in conjunction with other studies to clarify the diagnosis. It takes a few minutes and is quite affordable.
Indications
Diseases that require such diagnostics:
- cholecystitis;
- pancreatitis;
- soft tissue damage;
- abscesses.
This method is used when the patient complains of:
- pain, discomfort in the abdomen;
- bloating;
- heaviness in the digestive system.
With the help of X-ray examination, peristalsis and tone of the organ, changes in the relief of the mucous membrane are clarified. The method also allows you to determine the level of fluid in hollow organs.
Contraindications
There are practically no contraindications to the study. The disadvantages of this method include:
- exposure to ionizing radiation on the patient;
- difficult assessment of organ functions;
When examining soft tissues with little distinguishable density, there is insufficient information content without the use of contrast agents.
Preparation
 The examination requires the absence of gases and food, liquid, and mucus in the hollow organs.
The examination requires the absence of gases and food, liquid, and mucus in the hollow organs.
Before the procedure, the following preparation is carried out:
- When examining the liver and gallbladder, radiopaque agents (Iopagnost, Holevid) are used, which accumulate in the gallbladder and liver. To study the contractility of the gallbladder, choleretic agents can be used.
- On the eve of the examination of the duodenum and stomach, for constipation and severe flatulence, do a cleansing enema and drink 30 g of castor oil.
- On the day of the procedure, if there is severe flatulence, a cleansing enema is also given 2 hours before fluoroscopy. And also if there is a large amount of mucus, liquid, or food debris in the stomach, rinsing is carried out 3 hours before the test.
It is better to conduct the study on an empty stomach, having eaten a light dinner the day before. Patients with normal bowel function do not require special preparation in the form of enemas or diets.
How is an abdominal x-ray done?
It is advisable to carry out a diagnostic study in different projections, since the photograph is a flat image of a three-dimensional organ, and you need to look at all the walls. Therefore, the study is carried out in different body positions.
During a procedure using barium, with the patient in a horizontal position, the movement of the contrast mass slows down, which allows it to fill the hollow organ and take the necessary pictures:
- after 1 hour– the contrast mass reaches the small intestine;
- 3 hours– accumulates in the transition between the small intestine and the large intestine;
- 6 hours– reaches the initial parts of the colon;
- 9 – colon and transverse intestine;
- 12 – sigmoid colon;
- 24 – large intestine.
The X-ray procedure is relatively inexpensive and varies depending on the type of examination:
- plain radiography – from 350 rubles;
- X-ray of the stomach – from 750 rubles;
- radiography with barium of the large intestine - from 600 rubles;
- small intestine - from 950 rubles;
- examination of the esophagus – from 500 rubles;
- cholangiopancreatography (examination of the liver and biliary tract) – from 1,500 rubles;
- irrigoscopy – from 1000 rub.
Since over the last 2 decades, progressive gastrointestinal diseases have become more common in people, when the corresponding symptoms appear, doctors prescribe their patients a time-tested research method called abdominal x-ray. This type of medical non-invasive manipulation is based on the effect of ionizing rays on the body, which “transparent” a certain area of the body and reflect the patient’s condition at the current moment in time, visualizing the most important structures - organs and tissues.
Main types of diagnostics
At the moment, the study is divided into only three main types, each of which is widely used in medical practice:
| Name | Short description | «+» | «-» |
| Plain radiography of the abdominal cavity | Only one main image is taken, reflecting the general condition of the pelvic bones, organs located below the diaphragm, and major large tissues. This type of diagnosis is often carried out during routine medical examinations. | relatively low radiation dose, speed (the procedure lasts a maximum of 1-2 minutes) | insufficient information content |
| Contrast radiography | Before the X-ray session begins, the patient is asked to drink a special composition, which will quickly spread throughout the body through the bloodstream and color its barely noticeable components. In rare cases, a person is given a substance through a tube | high level of visualization of dense tissues, detection of tumor formations of any stage | duration (a session can take up to 2 hours), rare occurrence of side effects (headaches, weakness, etc.) |
| X-ray | In this case, the image of the organ system is displayed on a special screen - a small sheet of thick cardboard on which special fluorescent particles are evenly distributed. In new generation devices, the image can be reflected on a computer monitor in real time | short duration (up to 7–10 minutes), quick development of the image, the ability to transfer the image to modern electronic media, painlessness, volumetric visualization | increased body radiation |
Progress of the procedure
As soon as the patient removes metal objects and decorative elements, he should position himself near the device, the position of which will be adjusted by the radiologist in accordance with the person’s height. After preparing the device, the specialist goes to his own separate office and adjusts its individual settings. Then the X-rays will begin to have a localized effect on the body, at this moment it is necessary to remain static - this will allow you to obtain the most reliable image.
If you need to hold your breath for a few seconds, the doctor will warn you about this. Since X-rays are a two-dimensional (flat) image, a second scan may be required with the body in a horizontal position. This approach allows you to study a medical problem in several perspectives, which increases the likelihood of a correct diagnosis.
Before the examination, you do not need to take off your clothes, but in some cases you will need to expose your stomach: you must first put on a loose jacket that can be easily lifted
When the examination results are ready, they are transmitted either to the patient or to the clinician. If an X-ray with contrast is required, before the actual start of the study, the person will be given a container with a suspension, which should be drunk to the bottom. Often, this radiopaque substance is barium sulfate, which has excellent throughput. The chemical element is insoluble in water, and therefore does not penetrate into the cellular structures of the gastrointestinal tract and is not absorbed into the blood.
The contrast is painlessly eliminated from the body naturally over the next 12–24 hours. Sometimes barium sulfate is replaced with another substance, for example, nitric oxide. This happens at the slightest suspicion of the presence of perforations (through holes) in the internal organs, since the more common contrast drug, when it enters the abdominal cavity, can cause peritonitis, which can be fatal.
Before taking an x-ray using a contrast solution, you should find out whether there is an individual intolerance to its components.
Object of study
X-ray diagnostics allows you to determine the structural features and location of such organs as
- spleen;
- prostate;
- ureters;
- pancreas;
- intestines;
- ovaries;
- testes;
- liver;
- uterus;
- kidneys;
- gallbladder and bladder;
- stomach.
An overview X-ray image can also show the diaphragm, heart, lower part of the lungs, and free pairs of ribs. Fluoroscopy, in addition, reveals the dynamics of development - displacement, extensibility and contraction of the heart muscle and other types of organs and tissues.
Indications for use
An X-ray of the abdominal organs is extremely necessary for those who have:
- abscess;
- polyps;
- pain in the lower back or abdomen;
- tumor process;
- suspicion of injury to any organs;
- diverticulitis;
- cysts;
- intestinal obstruction;
- chronic bloating, etc.

Sharp pain in the right quadrant of the abdomen is a reason to urgently consult a doctor and undergo an x-ray: this symptom may signal inflammation of the appendix
A survey x-ray should be taken at least once a year to prevent gastrointestinal diseases.
Main contraindications
The procedure using ionizing radiation is characterized by an almost complete absence of contraindications. X-rays are prescribed even if a person has implants, piercings and tattoos, which is impossible with MRI. However, two categories of people should not visit the X-ray room without special circumstances: pregnant women, minors under the age of 12 years.
If necessary, expectant mothers will most likely be prescribed alternative diagnostic methods - ultrasound or MRI. After all, X-ray radiation will focus specifically on the abdominal region of the body, where the developing fetus is located. Since the consequences of X-ray exposure on the baby are officially considered unstudied, this diagnosis should be neglected until the end of the gestation period.
If a person suffers from dehydration (dehydration), cystic fibrosis or bronchial asthma, the possibility of undergoing the study must be discussed in advance with the treating doctor. X-rays are not performed on children at all, since the radiation dose from the device significantly exceeds the usual daily norm.
What does an x-ray show?
A doctor with the proper level of qualifications will be able to detect the following diseases and phenomena on an x-ray:
- tumors at any stage of development;
- appendicitis;
- inflammatory process (peritonitis, cholecystitis, etc.);
- nephrolithiasis (formation of kidney stones);
- pancreatitis;
- polyps;
- internal hematomas;
- abnormal structure of hollow organs;
- cholelithiasis;
- polycystic disease;
- diverticulitis;
- intestinal obstruction;
- various injuries;
- biliary and hepatic colic.

In the X-ray images, Kloiber's cups are visualized on the left, and the crescent sign on the right
In a young child, using X-rays, you can determine the location of swallowed foreign objects: coins, buttons, needles, beads, nuts, etc. Sometimes a specialist can detect quite dangerous phenomena on photosensitive film: Kloiber's cups and the crescent sign.
The sickle symptom is an accumulation of free air caused by a violation of the integrity of one of the sections of the gastrointestinal tract. Externally, it is a lightened crescent-shaped spot, which is most often located under the right dome of the diaphragm - the muscular septum separating the abdominal cavity from the chest. Kloiber's bowls resemble bowl-shaped two-layer elements filled not only with gases, but also with liquid.
If the number of vertically oriented spots prevails in the image, then the patient has obstruction of the large intestine, and if horizontal, then obstruction of the small intestine. Both cases considered indicate the presence of extremely advanced pathologies, which after X-rays should be eliminated as soon as possible.
Stages of preparation for radiography
If a person is urgently admitted to the hospital, special preparation for an x-ray is not required. In the case of a scheduled examination, it is worth taking care in advance to cleanse the body of toxins, which are reflected in the image in the form of unnecessary shadows that make it difficult to make a diagnosis. 2-3 days before the x-ray, beans, confectionery, raw fruits and vegetables, milk, and fast food should be excluded from the diet.
This product causes gases to appear in the intestines, which also “smear” the image on the film. You should drink enough clean water and simple meals. On the eve of the study, it is advisable to do a cleansing enema. The use of strong laxatives, for example, Guttalax and Bisacodyl, is discussed individually with the doctor.

The diet involves unlimited consumption of slimy porridges and creamy soups
Where can I get an abdominal x-ray?
After the patient receives a referral for an x-ray from a nephrologist, gastroenterologist, endocrinologist or urologist, it is worth finding out about the availability of specialized centers equipped with the necessary devices at their place of residence. You need to pay attention not only to the price of an x-ray, but also directly to the category of the medical institution, the qualifications of the doctors and the model of the equipment used for scanning.
Also, do not neglect reviews on the Internet and the opinions of familiar people. If the previously chosen clinic is characterized extremely negatively by former patients, you should refuse to visit it. Even if the stumbling block becomes a financial issue (in the case of paid centers), it is better to save the required amount of money and maintain your health than to lose it due to your own stinginess.
Cost of examination
Since each region of Russia has different price indicators, the cost of research in different cities varies significantly. As a rule, a person will need to pay from 350 to 2100 rubles for an x-ray of the abdominal organs. In the Moscow region, the price can reach 3,000 rubles. It is worth keeping in mind that interpretation of the x-ray is also included in the total cost. If the doctor has given the patient a referral for the procedure, then it will be carried out at the expense of compulsory medical insurance (i.e., free of charge).

If a doctor at a private clinic insists on paid x-rays in their institution, without particularly justifying his choice, it is recommended to consult with independent doctors before agreeing to radiation diagnostics
Differences and advantages of CT and X-ray
In fact, computed tomography is also a type of research based on the use of X-rays. Only when scanning does the image reflect the state of the organs in several sections and projections, which allows you to view a particular area of the body from the necessary angles. Although CT is more informative, it has not managed to displace classical x-rays from medical practice, which has some advantages:
- a high level of safety (the radiation dose is 10–20 times lower than with tomography);
- low cost;
- accessibility for the majority of the population.
Moreover, X-rays best visualize bone tissue, and CT scans best visualize the structure of bones, adjacent vessels, organs and soft tissues. In order to make the right choice, you should consult in advance with a specialist of a certain profile, and then adhere to his recommendations, developed on the basis of the patient’s individual indicators.