Normal eye pressure values. Eye pressure: symptoms, normal, treatment of increased. Symptoms of high eye pressure
Pressure exerted by liquid contents eyeball on the sclera and cornea of the eye, called intraocular. An increase or decrease in this indicator entails a decrease in visual acuity. With this problem, it is recommended to individually consult an ophthalmologist.
Normal intraocular pressure in adults
Valid range intraocular pressure varies from 11 to 21 mm. rt. Art.
Average is 16 mm. rt. Art.
The indicated figures may deviate by 7–8 mm. rt. Art., while in individual clinical cases they remain acceptable values. The normal indicator is affected by climatic conditions, gender, change of day, etc.
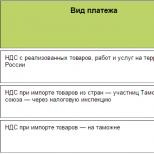
| Age, years | Acceptable measurement of intraocular pressure, mm. rt. Art. |
|
Normal eye pressure in children
Indicator in childhood does not differ from data in adult patients. Normal eye pressure can rise or fall for certain reasons. If there are disturbances, the child begins to have a headache, vision problems arise, and changes in the psycho-emotional state are observed. An ophthalmologist can determine the etiology of the pathological process, and diagnosis is carried out using tonometry. Normal indicators in childhood:
- full-term children: up to 1 year – 17.33 +/- 0.59 mm. rt. Art., from 1 to 3 years – 16.64 +/-0.17 mm. rt. Art.;
- premature: up to 1 year – 17.08 +/- 0.24 mm. rt. Art., from 1 to 3 years – 16.85 +/-0.23 mm. rt. Art.
For glaucoma
Wherein ophthalmological disease Intraocular pressure increases, but visual acuity may remain at the same level. During the pathological process, the optic nerve is damaged.
The greater the deviation from the norm, the more dangerous the disease.
We are talking about severe ocular hypertension with an intraocular pressure of 26 mm or more. rt. Art. Normal value it cannot happen when you are sick. According to the degree, pressure in glaucoma is distinguished:
- moderately increased – up to 33 mm. rt. Art.;
- high – from 33 mm. rt. Art.

How is eye pressure measured?
To measure fundus pressure, ophthalmologists use several proven methods that speed up diagnosis; their data will help choose a treatment regimen:
- Palpation (approximate). The ophthalmologist presses on the upper eyelid and gives a rough assessment of the condition of the fundus. Another name for the method - finger - is inaccurate.
- Contactless. The method is based on the use of modern tonometers, which are complex electronic devices.
- Contact. Diagnosis is carried out using tonometers, it is painful, and there is a high probability of infection through the device.
Classification of popular diagnostic methods:
- Electronography. It's painless and safe method changes based on increased fluid production inside the eye.
- Tonometry according to Maklakov.
Diagnosis is carried out under local anesthesia, since the procedure gives the patient painful sensations, internal discomfort.
Special weights are placed on the eye, previously soaked in a solution of pigment dye. Afterwards, the print obtained on a sheet of white paper is examined. The higher the indicator, the less paint is washed off from the records.
- Goldmann tonometer. The slit lamp releases a measured volume of air at a predetermined pressure. At this time, a special sensor reads the voltage of the cornea, which changes shape under the influence air flow. The diagnostic method is complex and is carried out only in a hospital.
- Icare tonometer. Diagnosis is painless, even for children. The innovative device has a special forehead rest. The working part of the tonometer is located opposite the center of the cornea. For getting reliable result you need to press the button and wait a few seconds.
- Scholz method. A special weight is applied to the eyeball, which is acted upon from the inside by intraocular pressure. As a result, the instrument needle begins to deviate. The resulting value is compared with the data from the calibration table. The procedure causes internal discomfort.
- Pneumotonometry. The required measurement is carried out using an air stream, and the procedure is painless and lasts a few seconds. Doctors use modern equipment.

Why is it important to monitor your eye pressure? The normal eye pressure at 60 years of age should not exceed 23 mm Hg. Indicators above these numbers may indicate incipient glaucoma.
Eyes are the most important organ human feelings, therefore it is important to monitor such indicators as eye pressure. The norm for 60 years differs little from that of younger people. If problems arise before sixty, there is still an opportunity to restore the functions of this sense organ. When the age exceeds sixty years, it is almost impossible to restore eye health. This is unlikely even with the help of surgery.
Why does vision deteriorate? One of the reasons is increased eye pressure. The organ of vision does not produce enough fluid to moisturize the membrane. As a result, the ability to see decreases significantly, which can lead to blindness. You can avoid problems by choosing the right medicine. In this case, self-medication is inappropriate, and to avoid more serious problems, it is best to seek advice from a specialist.
In humans, elevated IOP is more common. Deterioration occurs from many reasons: excessive work at the computer, poor nutrition, lack of vitamins, external factors. It is less likely to encounter a problem too low pressure. The initial symptoms of the disease are almost impossible to notice. However, the consequences low blood pressure fluid inside the eyes - loss of vision.
The risk of developing the disease increases with a person's age. After all, the body’s ability to recover gradually decreases, therefore the risk of such pathologies increases every year:
- glaucoma;
- farsightedness;
- myopia.
The disease is a consequence high pressure. People who are diagnosed with glaucoma can also suffer from diabetes, atherosclerosis. Sometimes the disease is inherited - from parents, grandparents. The onset of the disease is characterized by the following symptoms:
- blurred vision;
- general appearance, as if in fog;
- a person looks at the light and sees a halo;
- periodic excessive visual impairment;
- nausea.
What is the danger of glaucoma? The disease can be cured only at the initial stage. And then only if you choose the right suitable drops.
To avoid possible problems and prevent the occurrence of practically incurable diseases, it is recommended to undergo regular examinations with a doctor. Young people should be examined at least once a year. Those who have reached the age of forty – twice. After sixty - more three times throughout the year.
But it’s not enough to go and get checked. It is also important to monitor nutrition - it affects a person’s health in general, and the state of vision separately. You cannot read in poor light, work at the computer for a long time, or watch TV. All these factors negatively affect the condition of the eyes. For example, when a person sits in front of a computer screen for a long time, he begins to blink less often and his eyes gradually dry out.
And if you regularly work in front of a screen, after a few years your ability to see will deteriorate.
Of course, you can take vitamins, eat pomegranate, carrots, cranberries. However, if you overstrain your eyes, this will not solve the problem.
Normal eye pressure after 60 years
With age, the cornea and eyeball change, and the flush of fluid inside the organ worsens. As a result, ophthalmotonus increases.
Of course, it's important to know. Usually it can vary within twelve to twenty-five millimeters of mercury. However, for those over sixty, the standard increases to twenty-three millimeters of mercury. In a person with glaucoma, the indicator increases to twenty-seven conventional units - this is at the initial stage.

If the disease progresses - from twenty-seven to thirty-two millimeters of mercury. The pressure indicator for deep glaucoma exceeds thirty-three mm Hg.
Symptoms of abnormal eye pressure
If a person has reduced rate, the symptoms of the disease are:
- blurred vision;
- the apple is atrophied;
- change in shape, sinking;
- the person rarely blinks;
- lack of shine on the cornea.
Symptoms of high blood pressure include:
- headache;
- eyes hurt;
- blurred vision;
- deterioration of lateral vision;
- narrowing fields of visibility;
- spots flash before my eyes.
In addition, the eyes often become red, watery, and painful. Fluctuations in pressure negatively affect not only the level of vision, but also the state of human health. After all, when an organ is sick, the whole body suffers. When the eyes hurt, not only the body suffers, but it also worsens psychological condition person. Who will be calm when there is fog in front of their eyes?
Why is unstable blood pressure dangerous?
Both high and low ophthalmotonus are dangerous for vision. A high rate, as mentioned above, contributes to the development of glaucoma. In addition, it is the cause of death of the optic nerve. And it can cause loss of vision.
As a result of a low indicator, the eyeball atrophies and the regulatory system in the vitreous body is disrupted. And eye health deteriorates sharply, sometimes pressure changes lead to blindness.
Conclusion
Of course, you need to take a responsible approach to your health: visit doctors regularly, eat right, don’t spend too much time at the computer (if you can’t do without this, you need to work only in good lighting in the room), and so on. After all, it’s easy to spoil the ability to see, but to preserve normal vision, you need to keep an eye on him.
Iphthalmotonus is created by intraocular fluid and vitreous(internal contents of the eyeball) onto the fibrous membrane, which includes the cornea and sclera. This pathology manifests itself as a pressing feeling and “bloating” in the eyes with colds, glaucoma, headaches, inflammation in the eyes.
What is eye pressure
A certain elasticity and density are inherent in the human visual organs. The functions of the optical system are ensured due to ophthalmotonus, which is created by aqueous humor. Its formation occurs through filtration of the liquid part of the blood in the processes of the ciliary body. From the posterior chamber, moisture penetrates through the pupil, lens and cornea into the anterior chamber into the vessels. Increased fundus pressure is called ocular hypertension and is divided into:
pseudohypertension;
symptomatic hypertension.
How is eye pressure measured?
A tonometer measures eye pressure in medicine. Verification procedure intraocular fluid called tonometry and is performed to identify dangerous disease organs of vision - glaucoma. The tonometer device records the degree of elasticity of the eye shell. Before the procedure, the patient is instilled with eye drops containing an anesthetic to avoid discomfort. There are several types of tonometry:
direct palpation or through the eyelids;
transpalpebral tonometry;
Goldman method;
electrotonography;
applanation tonometry according to Maklakov;
corneometry or pachymetry (measurement of corneal thickness).
Why is eye pressure dangerous?
A prolonged state of tension leads to atrophy of the optic nerve and blindness. Why is eye pressure dangerous? With increased IOP, cataracts and glaucoma develop, which sharply reduces vision. If treatment is not carried out, you can stop seeing. Women and men over 40 years of age, elderly people, and those with a genetic predisposition to glaucoma are at risk. The child may develop congenital glaucoma. Symptoms of a slight decrease in visual acuity occur almost unnoticed until the eye begins to see poorly.
Normal eye pressure
Ophthalmologists say that the norm of intraocular pressure or ophthalmotonus in an adult should be within the range of 10-23 mm Hg. Art. At this level of elasticity of the intraocular fluid, the optical properties of the retina are supported and metabolic and microcirculatory processes in the organs of vision are regulated. It is necessary to take measures to normalize the indicator immediately, and not lead to glaucoma, which forms with an increased value. The rate decreases less frequently.
Increased intraocular pressure
An increased value is considered to be one that rises to 30-35 mmHg. Art. For early diagnosis undergo prophylaxis annually. It happens that increased intraocular pressure occurs due to diseases of the endocrine system, while taking medications or under the influence of other factors. In this case, after deciphering the study, ophthalmologists do not carry out intensive treatment, limiting themselves to eliminating the cause and monitoring the patient’s further condition.
What causes eye pressure to increase?
With normal indicators, the eye is not subject to stress and the person feels normal without any symptoms. When malfunctions occur in the body, when the secretion of natural fluids of the organs of vision increases, the work is disrupted of cardio-vascular system. This leads to jumps in the indicator. The cause of symptoms may be anatomical changes in the organs of vision.

Other causes of increased intraocular pressure:
the presence of atherosclerosis;
farsightedness;
disruption of the heart and blood vessels;
hereditary factor;
emotional stress;
severe mental or physical stress.
Symptoms of eye pressure
A person may not feel symptoms at the initial stage of the disease, which is manifested by heaviness in the eyes and increased fatigue. Such signs are explained by lack of sleep or overwork of the body, but if after rest the symptoms remain, then treatment is necessary. As the disease progresses, it becomes noticeable, causing discomfort to the person. The signs of eye pressure described below will help determine an increase in the indicator:
a sharp decrease in visual acuity;
the appearance of bradycardia;
cloudiness, hazy vision;
rainbow circles before the eyes;
severe headaches in the temples or around the eyes;
dizziness;
corneal edema;
lack of pupil reaction to light.
Eye pressure - the symptoms and treatment of which can be suggested by a doctor, is characterized not only by an increase, but also by a decrease in ophthalmotonus. Low reading is less than 10 mm Hg. Art. called ocular hypotony. Symptoms of intraocular pressure due to infection, inflammation and dehydration:
stop shining;
sometimes the eyeballs sink;
gradual deterioration of vision.
Treatment of eye pressure
Minor fluctuations in ophthalmotonus do not require treatment, since they do not affect visual acuity. When serious symptoms The question arises, how to treat eye pressure? The doctor prescribes medications, during which it is necessary to adhere to preventive measures, for example: sleep on high pillows, do not be exposed to prolonged stress, take brisk walks. You can get rid of the disease and treat eye pressure at home, using folk remedies, or resort to laser therapy.

Medicine for eye pressure
Therapeutic techniques that cannot be prescribed to yourself will help reduce ophthalmotonus. Medicinal medicine for eye pressure can only be prescribed by an ophthalmologist. During the consultation, you will undergo an examination that will help determine the type of disease and select effective drugs, normalizing indicators. There are 3 types of medications that are used to treat high IOP in adults:
Medicines that can be used to open other pathways for the outflow of fluid.
Medicines that help reduce fluid production inside the eye.
Preparations to improve the circulation of ocular fluid (tablets, drops).
How to lower eye pressure at home
How to relieve eye pressure at home without resorting to medications? If the pathology has just begun to manifest itself, then performing simple preventive measures, you can eliminate the risk of complications. To do this, you need to avoid wearing clothes that block the flow of blood from the veins of the head (do not wear ties, do not wear tight collars). In addition to restrictions on physical and mental activity, you can lower eye pressure at home in the following ways:

do not tilt your body down;
give up alcohol and cigarettes;
exclude coffee, tea, salt;
do not drink a lot of liquid;
light massage along the upper eyelids.
How to relieve eye pressure with folk remedies
After consulting an ophthalmologist, treatment with folk remedies can be carried out in conjunction with the main one, but only at the initial stage of the disease. How to reduce eye pressure? For effective treatment you will need patience and compliance. preventive measures. Folk remedies from eye pressure are contraindicated in case of individual intolerance and allergic reactions. List of proven recipes for adults for high IOP:
An infusion of nettle, sleep herb and wild pear shoots. Drink 3 times a day before meals.
Drops of mint oil (1 drop), distilled water (100 ml).
Use aloe vera liquid (pour 3 leaves with a glass of boiling water, cook for 6 minutes) to rinse your eyes 4 times daily.
Oral remedy: motherwort herb (15 g), hot water 250 ml. Leave for an hour, strain through cheesecloth, take 1 tbsp. l. 3 times.
You can make eyelid ointment from crushed dandelion and honey (proportions 1:1).
Video: increased eye pressure
Intraocular pressure is the pressure under which the ocular fluid is in the cavity of the eyeball. Ideally, IOP does not change, which creates stable physiological conditions for all eye structures. Normal pressure inside the eyes provides normal level microcirculation and metabolism in eye tissues.
When pressure decreases or increases, it poses a danger to the normal functioning of the visual apparatus. A persistent decrease in intraocular pressure is called hypotension; persistent increased pressure is characteristic of the development of glaucoma.
Unfortunately, even today, in the age of developed medical technologies, many people cannot boast that they have checked their intraocular pressure at least once in their lives. It is this behavior that leads to the fact that approximately 50% of patients come to the doctor too late, when treatment options are already very limited.
Normally, intraocular pressure in adults should be within the range of 10-23 mm. rt. Art. This level of pressure allows you to maintain microcirculatory and metabolic processes in the eyes, and also maintains the normal optical properties of the retina.
IN ophthalmological practice most often there is an increase in IOP. Basic clinical form Increased intraocular pressure is glaucoma.
The causes of this disease are:
- increased tone of arterioles of the ciliary body;
- disruption of the innervation of the vessels of the eye by the optic nerve;
- disruption of IOP outflow through Schlemm's canal;
- high pressure in the scleral veins;
- anatomical defects in the structure of the eye chambers;
- inflammatory lesions of the iris and choroid eyes – iritis and uveitis.
In addition, increased pressure inside the eye comes in three types:
- Stable - IOP is constantly above normal. This pressure inside the eyes is the first sign of glaucoma.
- Labile - IOP periodically increases, and then returns to normal normal indicators.
- Transient - IOP increases once and is short-term in nature, and then returns to normal.
Increased ophthalmotonus can be caused by fluid retention in certain kidney diseases and heart failure. In addition, it is caused by Graves' disease(diffuse toxic goiter), hypothyroidism (disease thyroid gland), menopause in women, poisoning by certain medicines, chemicals, tumor processes and inflammatory diseases eyes, eye injuries.
All of the above reasons contribute to the periodic appearance of increased intraocular pressure. If the disease lasts long enough, it can contribute to the development of glaucoma, which will require long and complex treatment.
Another common complication of increased intraocular pressure is optic nerve atrophy. Most often it is noted general decline vision, up to its complete loss. The affected eye becomes blind. Sometimes, if only part of the nerve bundles atrophies, the field of vision changes, and entire fragments may fall out of it.
Low eye pressure
Low eye pressure is much less common, but poses a much greater threat to eye health. The causes of low intraocular pressure can be:
- surgical interventions;
- eye injuries;
- underdeveloped eyeball;
- retinal disinsertion;
- lowering blood pressure;
- detachment of the choroid;
- underdevelopment of the eyeball.
If left untreated, decreased internal pressure in the eyes can lead to significant visual impairment. If atrophy of the eyeball occurs, pathological disorders become irreversible.
Symptoms of eye pressure
Here are the symptoms of increased intraocular pressure:
- Impaired twilight vision.
- Vision deterioration is actively progressing.
- The field of view is significantly reduced.
- The eyes get tired too quickly.
- Redness of the eyes is observed.
- Intense headaches in the suprafrontal arches, eyes and temporal area.
- Midges or rainbow circles flash before your eyes when you look at the light.
- Discomfort when reading, watching TV or working on a computer.
Now in more detail about the manifestations of low intraocular pressure. They are not as obvious and noticeable as with promotion. Often a person does not notice any changes at all and only after a year or several years does he discover that his vision has deteriorated. And yet, there are some possible symptoms that are more related to concomitant problems and pathologies that may allow one to suspect a decrease:
- Decreased visual acuity;
- Visible dryness of the cornea and sclera;
- Decreased density of the eyeball to the touch;
- Retraction of the eyeball in the socket.
In the absence of medical correction, this condition can cause subatrophy of the eye and complete loss of vision.
How is intraocular pressure measured?
Preventative checks of intraocular pressure are recommended as needed, and for persons over 40 years of age every three years.
A specialist can measure intraocular pressure without using any devices. This method is called palpation. The person looks down, covering his eyes with his eyelids, and the doctor presses his fingers on the upper eyelids of the eyes. This is how the doctor checks the density of the eyes and also compares their density. The fact is that in this way it is also possible to diagnose primary glaucoma, in which the pressure in the eyes varies.
For more accurate diagnosis A tonometer is used to measure intraocular pressure. During the procedure, special colored weights are placed on the center of the patient's cornea, the imprint of which is later measured and deciphered. To ensure that the procedure is painless, the patient is local anesthesia. The norm of intraocular pressure is different for each device. If the procedure is carried out using a Maklakov tonometer, then the normal intraocular pressure is up to 24 mm. rt. Art., but normal pneumotonometer readings are within 15-16 mm. rt. Art.
Diagnostics
To figure out how to treat intraocular pressure, the doctor must not only diagnose it, but also determine the cause of its development.
An ophthalmologist is involved in the diagnosis and treatment of conditions associated with increased or decreased intraocular pressure.
In parallel, depending on the cause of the violations, consultations with the following doctors may be prescribed:
- therapist;
- neurologist and neurosurgeon;
- traumatologist;
- cardiologist;
- endocrinologist;
- nephrologist.
The doctor asks the patient in detail about his symptoms, and then conducts an examination of the fundus. If there are appropriate indications, the patient will be sent for a procedure to measure intraocular pressure.
Treatment of intraocular pressure
The choice of treatment tactics depends on the cause that provoked a decrease or increase in intraocular pressure in an adult.
With increased intraocular pressure, the following conservative measures can be used as treatment:
- Drops that improve nutrition of eye tissue and fluid outflow.
- Treatment of the underlying disease if the increase in intraocular pressure is symptomatic.
- If drug methods are ineffective, laser treatment is used.
Here's what you can do to reduce intraocular pressure:
- Oxygen therapy (use of oxygen).
- Vitamin B1 injections.
- Drops based on atropine sulfate.
- Injections (subconjunctival) of atropine sulfate, dexamethasone or sodium chloride solution.
In general, treatment for low intraocular pressure consists of treating the underlying disease that led to the disorder.
Most radical method treatment of intraocular pressure - microsurgical technologies: goniotomy with or without goniopuncture, as well as trabeculotomy. During goniotomy, the iridocorneal angle of the anterior chamber of the eye is dissected. Trabeculotomy, in turn, is a dissection of the trabcular meshwork of the eye - the tissue connecting the ciliary edge of the iris to the posterior plane of the cornea.
Prevention
To avoid discomfort in the eye organs, it is necessary to avoid stress and not overwork. If you need to spend a lot of time in front of a monitor screen, you should take five-minute breaks every hour. Closing your eyes, you need to massage your eyelids and walk around the room.
Nutrition is also important. Products should be fresh and healthy; you should avoid those products that can lead to the accumulation of cholesterol. In autumn and winter, it is advisable to take vitamins.
The fluid localized inside the eye puts pressure on its membrane. In medicine, this phenomenon is called ophthalmotonus. Under the influence of external or internal factors, it can change upward or downward. There is a deviation in the blood supply to the eyeball, which disrupts its functioning. The patient begins to suffer from severe headaches and blurred vision. To prevent the development of the pathological process, you will need to consult an ophthalmologist. The specialist will measure the eye pressure, identify the cause of the malfunction and draw up a treatment regimen.
Features of ophthalmotonus
Intraocular pressure (IOP) is an indicator of the strength of fluid (blood and aqueous humor) to the outer shell. It directly affects all processes in visual organ. An increase or decrease in ophthalmotonus occurs due to disruptions in internal circulation.
Fundus pressure is included in general concept intraocular pressure. The definition refers to the force of the latter's influence on the back of the shell. The concepts are not considered separately.
Normally, every minute 2 mm³ of fluid enters the eye and a similar volume should exit it. If the outflow does not occur fully, then the eye pressure increases, which leads to deformation of the capillaries and a decrease in visual acuity. The increase in tone is classified as follows:
- Transient temporary increase. It is mainly a consequence of stress and overwork. Goes away on its own after rest.
- Labile growth of tone is more stable. The problem occurs periodically. Normalization occurs independently.
- Persistently high eye pressure is called glaucoma. It does not return to normal on its own and leads to blindness.
If high ophthalmotonus does not decrease for a long time, then the risk of consequences increases. The patient's optic nerve gradually atrophies, cataracts and glaucoma develop. Without undergoing a course of treatment, the voiced pathological processes will lead to blindness. People over 40 years of age are most susceptible to high eye pressure. In children, only the congenital form of glaucoma occurs. The main problem of early diagnosis is mild symptoms at the beginning of development. They consult a doctor mainly at an advanced stage.
A decrease in ophthalmotonus occurs extremely rarely. The development of such a pathological process is dangerous due to its hidden course. People turn to a specialist mainly when it is no longer possible to fully restore vision. The early symptom is often just dry eye.
Acceptable standards
Intraocular pressure is measured, like blood pressure, in mm Hg. Art. In children and adults, the indicator ranges from 9-23 units. Measurements of the strength of tone are carried out throughout the day. After waking up, the measurement result will be the highest, and before going to bed - the lowest. The difference in indicators mainly does not exceed 5 mm Hg. Art. Such a deviation is not considered a pathology and is often only an individual feature. There is no need to reduce ophthalmotonus.
Mature people (over 40-45 years old) are at risk of developing glaucoma, especially if there are several exposure factors. They are recommended to undergo an annual examination for timely detection of abnormalities in ophthalmotonus. Acceptable rate in mature people it reaches 26 mm Hg. Art. It is increased due to age-related changes that affect the entire body, including the eyes.
If ophthalmotonus is measured using the Maklakov method, the norm increases by 4-6 units. The changes are associated with the pressure exerted by the weight on the surface of the eyeball.
Pressure in glaucoma
Increased intraocular pressure gradually leads to the development of glaucoma. It is divided into 4 stages:
- basic (up to 27);
- pronounced (from 27 to 32);
- neglected (over 33);
- terminal (significantly more than 33).
Methods for determining pressure
IN hospital conditions To determine ophthalmotonus, doctors use the most accurate and proven procedures:
- Palpation. The doctor will press lightly with their fingers on the eyelids to assess the degree of elasticity of the eyeballs. If they are too soft, then the pressure is low, and if they are too hard, they indicate increased tone.
- Maklakov method. A weight weighing up to 10 g, painted with harmless paint, is applied to the cornea. With its weight, it pushes the liquid out of the chambers. The pressure force is determined by the size of the resulting imprint on the load. It is applied to paper previously moistened with alcohol. To prevent discomfort, before starting the measurement procedure, the doctor will administer local anesthesia, and after it is completed, drop a disinfectant solution into the eyes.
- Contactless method. The surface of the eye is exposed to air supplied under a certain pressure. Based on the result obtained, the specialist calculates ophthalmotonus. The technique is used if glaucoma is suspected. Among its advantages, the absence of contact with the surface of the eye and the accuracy of measurement clearly stand out.
Causes of fluctuations in ophthalmotonus
Jumps in eye pressure are predominantly observed in people at risk. It includes patients with the following problems:
- pathologies of the heart and blood vessels;
- eye diseases;
- atherosclerosis;
- genetic predisposition.
Increased eye pressure is the most common. Its growth is influenced by the following factors:
- mental illness;
- nervous breakdowns;
- constant exposure to stressful situations;
- eye strain from computers, phones and other gadgets;
- the impact of hypertension;
- chronic kidney pathologies;
- diseases of the heart and blood vessels;
- problems with the thyroid gland;
- poisoning of the body with chemical elements.
For the reasons stated, intraocular pressure will increase for a certain period of time. On an ongoing basis, high tone remains with the development of glaucoma.
Low eye pressure is much less common. Deviation occurs for the following reasons:
- low blood pressure;
- head and eye injuries;
- advanced form of diabetes mellitus;
- development inflammatory process in the eyeball;
- liver pathologies;
- dehydration due to the development of an infectious disease;
- retinal detachment.
Clinical picture
In most cases, the cause of surges in eye pressure cannot be identified in time. It will be virtually impossible to completely restore vision. The problem is associated with mild symptoms on early stages.
A clear sign of a decrease in ophthalmotonus is a decrease in visual acuity. If the patient does not undergo a course of treatment, then over time the eyes will become dry, begin to sink, atrophy and change shape. If tone drops due to infection in the body or its severe dehydration, loss of shine and rare blinking are added to the main symptoms.
High eye pressure initially also occurs sluggishly. Gradually, the patient begins to notice the development of the following clinical picture:
- redness of the eyes;
- pain in the temple area;
- constant feeling of heaviness and fatigue of the eyeballs;
- drop in visual acuity;
- the appearance of “flies” before the eyes;
- noticeable deterioration of vision in the dark;
- migraine attacks with pain radiating to the eyes;
- areas falling out of sight;
- decreased lateral visual acuity.
Course of therapy
After identifying an increase or decrease in ophthalmotonus, the doctor will select a treatment regimen based on the reason for the deviation from acceptable values. In mild cases and as a complement to more advanced forms of pathology, the following remedies are used:
- classes therapeutic exercises for eyes;
- wearing special glasses, for example, Professor Pankov;
- reducing the time spent on processes that strain the eyes.
It is advisable for the patient to walk in the fresh air more often and follow the rules healthy image life. The most important thing is to give your eyes more time to rest. If the cause of the jump in ophthalmotonus is other pathological processes, then they must be eliminated.
Drug treatment
In more difficult cases application will be required special drops. They provide:
- improving fluid outflow;
- reduction in moisture production;
- a combination of both actions.
The most common groups of drops are:
- Beta-blockers (Timol, Aritel, Tirez) help reduce the synthesis of fluid in the eyeball and reduce its volume.
- Cholinomimetics (Pilocarpine, Carbachol) constrict the pupil and stimulate the outflow of moisture.
- Latanprost-based drugs (Gluprost, Xalatamax, Latanomol) improve fluid outflow and are prescribed mainly for glaucoma. The progression of the disease is significantly reduced and its symptoms are relieved.
The drugs have their own contraindications, dosages and combination features. If used incorrectly, there is a risk of worsening the condition. The choice of drops should be entrusted to an ophthalmologist. He will examine the patient and draw up an effective medication regimen treatment. If possible, it is recommended to use products with a combined effect (Fotil, Xalacom). The price of such drugs is higher, but with their help you can achieve the desired result much faster.
Surgery
Constant jumps in ophthalmotonus lead to severe damage to the eyeball. Simple treatments and pills will not solve the problem. You will need to contact an experienced surgeon. The most relevant types of surgical intervention performed using a laser are:
- excision of the iris;
- trabecular extension.
A successful operation will improve the outflow of fluid inside the eye, thereby stabilizing the pressure. It is not always possible to completely eliminate the consequences, but you can increase visual acuity and stop or slow down the development of the pathological process.
There are generally accepted standards for ophthalmotonus by age. If deviations from them are detected, the patient is sent for examination to determine the causative factor. After its detection, the doctor draws up a treatment regimen, taking into account individual characteristics patient and the presence of other diseases. In mild cases, it is enough to change your lifestyle and do eye exercises. Launched forms pathologies require drug treatment and even surgery.
Ocular pressure, intraocular pressure (IOP) or ophthalmotonus, is the pressure of the fluid contained inside the eyeball on the walls of the eye. Intraocular pressure is now determined for all persons who have crossed the 40-year mark, regardless of whether the person makes complaints or not. This is due to the fact that increased eye pressure is the main prerequisite for the development of a disease such as glaucoma, which, if left untreated, leads to complete blindness.
Intraocular pressure is measured using a special tonometer, and the results are expressed in millimeters of mercury (mmHg). True, ophthalmologists of the 19th century judged the hardness of the eyeball by pressing on the eye with their fingers. In other cases, in the absence of equipment, a similar method is used today as a preliminary assessment of the condition of the visual organs.
Why is it important to know IOP?
The attention paid to such an indicator of health status as intraocular pressure is due to the role played by IOP:
- Maintains the spherical shape of the eyeball;
- Creates favorable conditions to save anatomical structure the eye and its structures;
- Maintains blood circulation in the microvasculature and metabolic processes in the tissues of the eyeball at a normal level.
The statistical norm of eye pressure measured by tonometric method is within 10 mmHg Art.(lower limit) - 21 mmHg Art. (upper limit) and has average values in adults and children are about 15 – 16 mm Hg. Art., although after 60 years there is a slight increase in IOP due to the aging of the body, and the norm of eye pressure for such persons is set differently - up to 26 mm Hg. Art. (tonometry according to Maklakov). It should be noted that IOP is not particularly constant and changes its values (by 3-5 mm Hg) depending on the time of day.
It would seem that at night, when the eyes are resting, eye pressure should decrease, but this does not happen in all people, despite the fact that the secretion of aqueous humor slows down at night. Closer to the morning, eye pressure begins to increase and reaches its maximum, while in the evening, on the contrary, it decreases, so in adults healthy people the most high performance IOPs are observed early in the morning and are lowest in the evening. Fluctuations in ophthalmotonus in glaucoma are more significant and amount to 6 or more mm Hg. Art.
Measuring intraocular pressure
It should be noted that not all people referred for annual preventive examinations to an ophthalmologist are enthusiastic about the upcoming measurement of intraocular pressure. Women may be afraid of ruining carefully applied makeup; men will refer to the absence of any complaints about their own organs of vision. Meanwhile, measuring intraocular pressure is a mandatory procedure for people who have turned 40 or older, even if they assure the doctor that they are in perfect health.
Measuring intraocular pressure is carried out using special equipment and instruments, and in general, modern ophthalmology uses 3 main types of measuring intraocular pressure:
- Pneumotonometry, very similar to Maklakov tonometry, but different in that it uses an air jet. Unfortunately, this study not particularly accurate;
- Electronography is the most modern method, successfully replacing the previous two. It is used mainly in specialized institutions (not all clinics can yet afford expensive ophthalmological equipment). The method is classified as non-contact, highly accurate and safe research.
tonometry according to Maklakov
The above-mentioned method according to Maklakov - many patients remember it, know it and most of all dislike it, since drops are dropped into the eyes, providing local anesthesia, and “weights” are installed (very a short time), which are quickly removed and lowered onto a clean sheet of paper to leave prints indicating the value of IOP. This method is more than 100 years old, but it still has not lost its relevance;
Most often in the Russian Federation and neighboring countries, Maklakov tonometry or non-contact tonometry using an electronograph are used.
Increased intraocular pressure
Increased eye pressure (ophthalmohypertension) is not necessarily the result of age-related changes, as many people think.
The reasons for increased IOP can be very diverse, for example:
- Constant tension on the organs of vision, leading to fatigue;
- Atherosclerosis;
- Persistent arterial hypertension(periodic surges in blood pressure are usually not dangerous for the eyes);
- Vegetative-vascular dystonia;
- Psycho-emotional stress, chronic stress;
- Fluid retention in the body due to cardiovascular pathology;
- Intracranial hypertension often causes increased fundus pressure;
- Professional activities (wind musicians);
- Individual (strength) physical exercises;
- Medicines used locally;
- Strong tea or coffee (due to caffeine);
- Heart rhythm disturbances, respiratory arrhythmia;
- Features of the anatomical structure of the eye;
- Intoxication;
- An inflammatory process localized in the organ of vision;
- Diencephalic pathology;
- Traumatic brain injuries;
- Diabetes;
- Menopause;
- Hereditary pathology;
- Side effects of certain medications, treatment with corticosteroid hormones.
Increased intraocular pressure is often a sign of glaucoma, the risk of developing which increases markedly after 40 years.
Warning symptoms of increased IOP
Increased eye pressure may not show any particular signs of trouble for a long time. A person continues to live in a normal rhythm, unaware of the impending danger, because the real symptoms are pathological condition eyes appear only when the IOP changes significantly towards an increase. And here are some signs of illness that may suggest that, putting everything aside, you need to immediately visit an ophthalmologist to check your vision and measure intraocular pressure:
- Pain in the eyes, in the eyebrow area, in the frontal and temporal areas (or on one side of the head);
- “Fog” before the eyes;
- Multi-colored circles when looking at a burning lamp or lantern;
- Feeling of heaviness, fullness and tiredness of the eyes at the end of the day;
- Attacks of unmotivated lacrimation;
- Change in corneal color (redness);
- Decreased visual acuity, lack of image clarity (with glaucoma, patients often change glasses).
An increase in IOP and the development of glaucoma can be suspected if a person often changes glasses because he begins to be unable to see in the “old” ones, and also if this disease was diagnosed in close relatives.
For starters, drops for eye pressure
If pathological process has not gone too far, but the risk of developing glaucoma is quite high, then treatment usually begins with direct action on high level IOP, and for this purpose the doctor prescribes eye pressure drops, which:
- Promote fluid outflow;
- Reduce the pressing effect on the eye capsule;
- Normalize tissue metabolism.
By the way, eye pressure drops can cover different pharmacological groups, This:
- F2α prostaglandin analogues (Travoprost, Xalatan, Latanoprost);
- Beta-blockers (selective - Betaxolol, and - non-selective - Timolol);
- M-cholinomimetics (Pilocarpine);
- Carbonic anhydrase inhibitors (local - Bronzopt, and in addition to drops for eye pressure: systemic - Diacarb in capsules and tablets).
In this regard, it is very important to correctly assess how drugs will affect the hydrodynamics of the organ of vision, whether it will be possible to quickly obtain a hypotensive effect, calculate how often a person will depend on drops, and also take into account contraindications and individual tolerance of individual drugs. If during the prescribed treatment everything did not go very smoothly, that is, special effect monotherapy with antihypertensive drugs is not obtained, you have to turn to combined treatment using:
- Travapress Plus, Azarga, Fotil-forte;
- α and β-adrenergic agonists (Adrenaline, Clonidine).
However, even in such cases, it is not at all advisable to use more than two different drugs in parallel.
In addition to the listed medications for glaucoma ( acute attack) osmotic agents are prescribed orally (Glycerol) and intravenously (Mannitol, Urea).
Of course, examples of eye pressure drops are not given so that the patient goes and buys them at the pharmacy on his own initiative. Data medicines and are prescribed and prescribed exclusively by an ophthalmologist.
When treating high eye pressure, in order to adequately assess the results achieved, the patient is regularly IOP measurement, visual acuity and the condition of the optic discs are checked, that is, during treatment the patient works closely with the attending physician and is under his control. To obtain the maximum effect from treatment and prevent addiction to the drugs, ophthalmologists recommend periodically changing eye pressure drops.
The use of drops and other medications that reduce IOP involves treatment at home. For glaucoma, treatment depends on the form of the disease and the stage of the glaucomatous process. If conservative therapy did not give the expected effect, laser treatment is used (iridoplasty, trabeculoplasty, etc.), which allows the operation to be performed without a hospital stay. Minimal trauma and small rehabilitation period They also provide the opportunity to continue treatment at home after the intervention.
In advanced cases, when there is no other way out, it is indicated for glaucoma surgery(iridectomy, fistulizing placements, operations using drains, etc.) with a stay in a specialized clinic under the supervision of doctors. IN in this case The rehabilitation period is somewhat delayed.
Decreased fundus pressure
Doctors involved in the treatment of eye diseases are aware of another phenomenon that is opposite to increased IOP -
ophthalmic hypotension
Hypotony of the eyes or decreased fundus pressure.
This pathology develops quite rarely, but this does not make it any less dangerous.
Unfortunately, patients with eye hypotony reach the ophthalmologist's office when a significant percentage of their vision has already been lost.
This late presentation is explained by the fact that there are no obvious signs of the disease; the initial stage proceeds almost without symptoms, except for a not very pronounced decrease in visual acuity, which people attribute to eye strain or age-related changes. The only symptom that appears later and can already alert the patient is considered dry eyes and loss of natural shine.
Factors that contribute to a decrease in intraocular pressure are not as diverse as the prerequisites that increase it. These include:
- Injury to the organs of vision in the past;
- Purulent infections;
- Diabetes;
- Dehydration
- Arterial hypotension;
- Alcoholic drinks and drugs (marijuana);
- Glycerin (if consumed orally).
Meanwhile, a person who pays as much attention to the eyes as other organs can prevent undesirable consequences lowering IOP by visiting an ophthalmologist and talking about the above-mentioned “minor” symptoms. But if you do not notice the signs of eye health in a timely manner, you may face the development of an irreversible process - atrophy of the eyeball.
Home treatment involves using eye drops: Trimecaine, Leocaine, Dicaine, Collargol, etc. Products with aloe extract, as well as B vitamins (B1), are useful.
Patients suffering from increased IOP, which threatens the development of the glaucomatous process, are recommended to follow some rules of prevention:
- Try to avoid hypothermia, stress and excessive physical stress(hard work, lifting heavy objects, tilting the head and body, causing blood to flow in larger quantities than the brain needs;
- Stop light activities athletics, but do not shy away from walking (away from city noise and gas pollution), feasible gymnastics for the respiratory system and the whole body, hardening the body;
- Treat chronic concomitant diseases;
- Once and for all, regulate the regime of work, night sleep, rest and nutrition (a lactic acid diet enriched with vitamins and minerals is preferable);
- On sunny summer days, when going outside, make it a rule not to forget glasses at home that provide eye comfort and protection (glasses should be purchased at Optics, and not at the market where they sell sunglasses, which can further increase EDC ).
As for low blood pressure, as mentioned earlier, it is a rare case, so patients who experience suspicious signs (dull, dry eyes) can be advised to contact a specialist as soon as possible, who will tell you what to do next.
Video: about increased intraocular pressure and glaucoma
Video: about low intraocular pressure and its causes
Step 1: pay for the consultation using the form → Step 2: after payment, ask your question in the form below ↓ Step 3: You can additionally thank the specialist with another payment for an arbitrary amount
Eye pressure helps maintain the stable functioning of the retina and the processes of microcirculation of metabolic substances in it. A decrease or decrease in this indicator may indicate the development of serious pathologies that can affect the acuity and quality of vision.
A decrease or increase in IOP indicates the development of pathologies
Eye pressure standards
Ocular monotonus or intraocular pressure (IOP) contributes to the normal nutrition of the eye shell and maintenance of its spherical shape. This is the result of the process of outflow and inflow of intraocular fluid. The amount of this very liquid determines the level of IOP.
Normal intraocular pressure
During the day, intraocular pressure can vary - in the morning it is higher, in the late afternoon it is lower. Ophthalmonormotension or normal IOP, regardless of age and gender, ranges from 10 to 25 mmHg. Considering the time of day, deviations from the reference values are allowed in the amount of no more than 3 mmHg.
Symptoms of intraocular pressure
Disorders of blood microcirculation inside the eye, as well as deviations in the optical properties of the retina, occur after 40 years. In women, IOP surges are observed more often than in men, which is associated with hormonal characteristics body (lack of estrogen during menopause).
The pressure inside the eye rarely decreases. A common problem is increasing this indicator. In any case, pathologies do not occur hidden, but are accompanied by specific signs.
Increased IOP
High pressure inside the eyes can occur in several forms:
- stable (values above normal on an ongoing basis);
- labile (periodic upward pressure surges);
- transient (there is a one-time and short-term increase in ophthalmotonus).
Stable IOP is the first sign of the development of glaucoma. Pathology occurs as a result of changes in the body that occur with age, or is a consequence of concomitant diseases, and appears in men and women after 43–45 years.
Symptoms of high eye pressure (glaucoma):
- the appearance of goosebumps or rainbow circles before the eyes when looking at the light;
- Red eyes;
- feeling of fatigue and pain;
- discomfort when watching TV, reading, working on a computer (tablet, laptop);
- decreased visibility at dusk;
- narrowing of the field of view;
- pain in the forehead, temples.
Eyes turn red when IOP increases
In addition to glaucoma, pressure depends on inflammatory diseases of the corresponding part of the brain, endocrine disorders, eye pathologies(iridocyclitis, iritis, keratoiridocyclitis) or from long-term treatment certain medications. This is ocular hypertension. The disease does not affect optic nerve and does not affect the visual field, but if left untreated it can develop into cataracts and secondary glaucoma.
Ocular hypertension is manifested by symptoms such as:
- headache;
- aching discomfort in the eyes;
- feeling of distension of the eyeball;
- blinking is accompanied by pain;
- constant feeling of tiredness in the eyes.
Unlike glaucoma, which develops after 43 years of age, ocular hypertension can develop in children and adults, and can be especially aggressive in women. Reduced pressure in the eyes
Ocular hypotension is rare and dangerous phenomenon in ophthalmology. With gradual development, the signs are mild (except for a gradual decrease in vision, the patient does not feel other abnormalities), which does not always make it possible to identify the pathology in the early stages and often leads to blindness (partial or complete).
At sharp decline IOP symptoms are more expressive:
- eyes lose their healthy shine;
- dryness of the mucous membrane appears;
- eyeballs may fall through.
To avoid loss of vision due to low pressure inside the eyes, it is necessary to undergo examination by a specialist at least once every 5-6 months.
Reasons for deviation from the norm
Lability of eye pressure may be the result of age-related changes, external irritants, congenital pathologies or disruption of internal systems.
Why does eye pressure increase?
The cause of a one-time (transient) increase in ophthalmotonus is the development of hypertension in humans. This also includes stressful situations and extreme fatigue. In such cases, simultaneously with IOP, intracranial pressure also increases.
Provoking factors for increased ophthalmotonus (with glaucoma) may be:
- severe dysfunction of the liver or heart;
- deviations in the functioning of the nervous system;
- endocrine pathologies (Bazedow's disease, hypothyroidism);
- severe menopause;
- severe intoxication of the body.
Hypothyroidism can cause high eye pressure
Ocular hypertension, unlike glaucoma, can develop not only in adults, but also in children. There are 2 types of pathology – essential and symptomatic. Both types are not independent diseases, but a consequence of serious pathologies of the eyes or vital systems.
The provoking factor of the essential form of high eye pressure is an imbalance between the production of intraocular fluid (increases) and its outflow (slows down). This condition often occurs due to age-related changes in the body and occurs in people after 50 years of age.
Symptomatic ocular hypertension occurs as a result of:
- eye pathologies – iridocyclitis, iritis, keratoiridocyclitis, glaucomocyclitic crises;
- long-term treatment with corticosteroid medications;
- endocrine (Cushing's syndrome, hypothyroidism) or hormonal (severe menopause) disorders;
- inflammatory processes in specific areas of the brain (hypothalamus).
Chronic intoxication can cause symptomatic ocular hypertension strong poisons(tetraethyl lead, furfural). Why is eye pressure low?
A decrease in eye pressure is observed less frequently than an increase, but is no less dangerous pathology.
The reasons for this condition are:
- inflammatory changes in the eyeballs – uveitis, iritis;
- foreign objects (squeaks, glass, metal shavings) or corneal bruise;
- intense loss of fluid from the body (occurs with peritonitis, dysentery);
- kidney disease;
- complications after operations;
- congenital anomalies (underdevelopment of the eyeball);
- retinal detachment.
Most often, reduced IOP occurs hidden, gradually worsening vision, up to blindness (if not treated).
IOP often decreases in kidney disease
Different pressure in the eyes
It is not uncommon for the pressure in the right and left eyes to differ by 4–6 mmHg. Art. This is normal. If the difference exceeds valid values, we are talking about development pathological changes. The cause of this condition may be the development of primary or secondary glaucoma. The disease can develop in one eye or in both eyes at the same time. In order to prevent negative consequences, it is important not to hesitate to consult a doctor at the slightest deviation in vision.
A strong difference in eye pressure indicates the development of pathological changes
Ocular pressure measurement
Eye pressure can be determined using daily tonometry. Analysis is carried out special techniques- study according to Goldman or using a Maklakov tonometer. The devices are shown in the photo. Both methods accurately test the eyes and guarantee a painless procedure.
Measuring IOP using a Goldmann tonometer
Maklakov tonometer - a device for measuring intraocular pressure
In the first case, an anesthetic substance and a contrast liquid are dripped into the patient's eyes, he is seated at a slit lamp on which a tonometer is installed, and the examination begins. The doctor places the prism on the eye and adjusts its pressure on the cornea. Using a blue filter, the specialist determines the right moment and deciphers the IOP using a special scale.
Monitoring intraocular pressure using the Maklakov method requires the patient to lie down.
The procedure takes place in several stages:
- An anesthetic liquid is dropped into the patient's eyes.
- A contrast liquid is placed on the prepared glass plates and the device is carefully lowered onto the cornea so that the colored parts come into contact with it.
- The pressure of a metal object slightly deforms the convex part of the eyeball.
- Similar actions are carried out with the second eye.
- The resulting circle prints are placed on damp paper and measured with a ruler.
To obtain accurate results, it is recommended to perform tonometry 2 times a day. This is explained by the fact that in different time days the values may vary slightly.
Which doctor should I contact?
An ophthalmologist can help solve vision problems.
The specialist conducts tonometry, studies the medical history and, if necessary, prescribes additional consultations with other doctors:
- neurosurgeon;
- neurologist;
- therapist;
- endocrinologist.
The need for examination by a specific specialist depends on the reason that led to changes in eye pressure.
What are the dangers of deviations from the norm?
Long-term untreated high or low eye pressure can lead to dangerous consequences:
- increased intracranial pressure;
- removal of the eye (with constant pain discomfort);
- complete or partial (only dark silhouettes are visible) loss of vision;
- constant severe pain in the frontal and temporal parts of the head.
It is important to understand that deviation in IOP is serious problem, which must be resolved quickly, otherwise there is a high probability of dangerous complications.
If IOP deviations are left untreated for a long time, severe pain in the temples and forehead may occur.
Treatment of eye pressure
To normalize IOP, improve metabolism and microcirculation, they are used medications. It is recommended to use traditional medicine methods as an aid.
Medicines
Drug therapy for abnormalities in eye pressure involves the use of drugs in the form of tablets and drops. Which medications are more effective depends on the stage of the disease, cause and type (increased or decreased ophthalmotonus).
Table “The best medications for intraocular pressure disorders”
The ophthalmologist selects all medications individually, based on the source of the disease, its severity and the characteristics of the patient’s body. Therefore, choosing medications on your own can greatly aggravate the existing problem.
Traditional medicine
You can normalize IOP at home using folk recipes.
Alcohol tincture of golden mustache
Grind the plant (100 g), place in a glass container and pour in 0.5 liters of vodka or alcohol. Leave for at least 12 days (shake regularly). Drink the prepared liquid in the morning on an empty stomach. Dose – 2 tsp. The product makes it possible to quickly reduce eye pressure and relieve unpleasant symptoms.
Golden mustache tincture helps normalize eye pressure
Red clover infusion
Brew 1 tsp in 250 ml of boiling water. chopped herbs, cover and let stand until completely cool. You need to drink the strained liquid half an hour before bedtime. Duration of treatment – 1 month.
Drink red clover infusion before bed
Healing lotions
Grind 1 apple, 1 cucumber and 100 g sorrel (horse) until mushy. Place the resulting mass on 2 pieces of gauze and apply to the eyes for 10–15 minutes once a day.
Apple and cucumber lotions are useful for IOP deviations
Dandelion and honey
Grind dandelion stems (2 tsp) and add 1 tbsp. honey, mix. Apply the creamy mixture to your eyelids in the morning and evening for 3-5 minutes, then rinse with warm water.
Apply a mixture of dandelion and honey to your eyelids 2 times a day
Motherwort decoction
Pour 1 tbsp into an enamel bowl. l. motherwort herbs, pour in 500 ml of water and simmer over low heat for 7 minutes (after boiling). Take the cooled drink 1 tbsp. l. morning, afternoon and evening.
Motherwort decoction normalizes IOP
Mint drops
Dilute 1 drop of mint oil in 100 ml of distilled liquid. Apply the prepared solution to the eyes once a day.
Dilute mint drops in water before instillation
Aloe decoction for washing eyes
Pour aloe (5 sheets) hot water(300 ml), simmer over low heat for 3-5 minutes. Use the cooled solution to rinse your eyes at least 4 times a day at equal intervals.
Wash your eyes with aloe vera decoction 4 times a day
Nettle and lily of the valley lotions
Add 3 tbsp to 200 ml of boiling water. l. nettle and 2 tsp. lily of the valley, leave to infuse for 8–10 hours in a dark place. Soak cotton pads in the herbal liquid and apply to eyes for 5–7 minutes.
Nettle and lily of the valley infuse for 10-12 hours
Potato compresses
Pass peeled potatoes (2 pcs.) through a meat grinder, pour in 10 ml of table vinegar (9%). Stir and leave to steep for 25–35 minutes. Place the resulting mixture on gauze and place on the eyelids and area around the eyes.
To normalize eye pressure, make eye lotions from potatoes
Dill infusion
Pour crushed dill seeds (1 tbsp) into 500 ml of boiling water, boil for 2-3 minutes, cool. Take 50 ml of herbal liquid before meals.
Take a decoction of dill seeds before meals
It is necessary to understand that traditional medicine recipes are, first of all, aid to normalize eye pressure. Cannot be replaced alternative medicine basic drug therapy, otherwise it is possible to worsen the course of the disease.
Eye exercises
Special eye exercises will relieve fatigue and tension and normalize IOP. It consists of simple exercises.
- Relaxation and stress relief. Blinking at a fixed time interval (4–5 seconds). You need to close your eyes with your palm, relax and blink a couple of times. Perform for 2 minutes.
- Strengthening and increasing flexibility of the eye muscles. Imagine an infinity sign (an inverted figure eight) and mentally draw it for 2 minutes, moving only your eyeballs (do not turn your head).
- Strengthening muscles and improving vision. First, focus your gaze on an object that is no more than 30 cm away. After 1–1.5 minutes, look at a more distant object. You need to move your gaze from one object to another at least 10 times, lingering on each for at least a minute.
- Improved focus. Extend your hand in front of you with your finger raised up. Smoothly bring the phalanges closer to the nose. Stop at a distance of 8 cm from your face and move your finger back. Do the exercise for 2–3 minutes, while keeping your eyes on your finger.
Warming up helps improve vision, normalize the balance between the secretion of tear fluid and its outflow, and reduce the load on the optic nerve.
- Monitor your sleep schedule. You need to sleep at least 8 hours a day.
- Take short breaks while working at the computer. Every 2 hours you need to give your eyes a rest for at least 10-15 minutes. At this time, you can do special exercises.
- News active image life. Spend more time outdoors, limit computer work and spend less time watching TV.
- Review your diet. Avoid drinking alcohol, limit coffee, tea, salt, sugar. Lean on fruits, vegetables, vitamin complexes, fish products.
- Visit an ophthalmologist once every 6 months and do not neglect any identified abnormalities.
- Do not self-medicate, strictly follow all recommendations of specialists.
If you have problems with IOP, exclude tea and coffee from your diet
It is important to understand that increased or decreased IOP can negatively affect eye health. It is important to carry out preventive measures on time and monitor your vision.
High or low eye pressure may be a sign of the development of glaucoma or eyeball atrophy. Pathologies rarely occur as independent diseases, they are mainly a consequence of external stimuli - injuries, stress, overwork, age-related changes, or internal violations– endocrine, cardiovascular, eye diseases. To prevent serious complications, it is important to have a timely examination by an ophthalmologist, regularly perform eye exercises, and strictly monitor your lifestyle and diet.
Intraocular pressure is the pressure under which the ocular fluid is in the cavity of the eyeball. Ideally, IOP does not change, which creates stable physiological conditions for all eye structures. Normal pressure inside the eyes ensures a normal level of microcirculation and metabolism in the tissues of the eyes.
When pressure decreases or increases, it poses a danger to the normal functioning of the visual apparatus. A persistent decrease in intraocular pressure is called hypotension; persistent increased pressure is characteristic of the development of glaucoma.
Unfortunately, even today, in the age of advanced medical technologies, many people cannot boast of having their intraocular pressure checked at least once in their lives. It is this behavior that leads to the fact that approximately 50% of patients come to the doctor too late, when treatment options are already very limited.
Intraocular pressure is normal in adults
Intraocular pressure is usually measured in millimeters of mercury. During the day it can have different indicators. So, for example, during the day the numbers can be quite high, and in the evening they drop. The difference, as a rule, does not exceed 3 mmHg.
Normally, intraocular pressure in adults should be within the range of 10-23 mm. rt. Art. This level of pressure allows you to maintain microcirculatory and metabolic processes in the eyes, and also maintains the normal optical properties of the retina.
Increased intraocular pressure
In ophthalmological practice, an increase in IOP is most often observed. The main clinical form of increased intraocular pressure is glaucoma.
The causes of this disease are:
- increased tone of arterioles of the ciliary body;
- disruption of the innervation of the vessels of the eye by the optic nerve;
- disruption of IOP outflow through Schlemm's canal;
- high pressure in the scleral veins;
- anatomical defects in the structure of the eye chambers;
- inflammatory lesions of the iris and choroid - iritis and uveitis.
In addition, increased pressure inside the eye comes in three types:
- Stable - IOP is constantly above normal. This pressure inside the eyes is the first sign of glaucoma.
- Labile - IOP periodically increases, and then returns to normal values.
- Transient - IOP increases once and is short-term in nature, and then returns to normal.
Increased ophthalmotonus can be caused by fluid retention in certain kidney diseases and heart failure. In addition, its causes include Graves' disease (diffuse toxic goiter), hypothyroidism (thyroid disease), menopause in women, poisoning with certain medications, chemicals, tumor processes and inflammatory eye diseases, and eye injuries.
All of the above reasons contribute to the periodic appearance of increased intraocular pressure. If the disease lasts long enough, it can contribute to the development of glaucoma, which will require long and complex treatment.
Another common complication of increased intraocular pressure is optic nerve atrophy. Most often, there is a general decrease in vision, up to its complete loss. The affected eye becomes blind. Sometimes, if only part of the nerve bundles atrophies, the field of vision changes, and entire fragments may fall out of it.

Low eye pressure
Low eye pressure is much less common, but poses a much greater threat to eye health. The causes of low intraocular pressure can be:
- surgical interventions;
- eye injuries;
- underdeveloped eyeball;
- retinal disinsertion;
- lowering blood pressure;
- detachment of the choroid;
- underdevelopment of the eyeball.
If left untreated, decreased internal pressure in the eyes can lead to significant visual impairment. If atrophy of the eyeball occurs, pathological disorders become irreversible.
Symptoms of eye pressure
Let's list the symptoms increased intraocular pressure:
- Impaired twilight vision.
- Vision deterioration is actively progressing.
- The field of view is significantly reduced.
- The eyes get tired too quickly.
- Redness of the eyes is observed.
- Intense headaches in the suprafrontal arches, eyes and temporal area.
- Midges or rainbow circles flash before your eyes when you look at the light.
- Discomfort when reading, watching TV or working on a computer.
Now in more detail about the manifestations low intraocular pressure. They are not as obvious and noticeable as with promotion. Often a person does not notice any changes at all and only after a year or several years does he discover that his vision has deteriorated. And yet, there are some possible symptoms that are more related to concomitant problems and pathologies that may allow one to suspect a decrease:
- Decreased visual acuity;
- Visible dryness of the cornea and sclera;
- Decreased density of the eyeball to the touch;
- Retraction of the eyeball in the socket.
In the absence of medical correction, this condition can cause subatrophy of the eye and complete loss of vision.
How is intraocular pressure measured?
Preventative checks of intraocular pressure are recommended as needed, and for persons over 40 years of age every three years.
A specialist can measure intraocular pressure without using any devices. This method is called palpation. The person looks down, covering his eyes with his eyelids, and the doctor presses his fingers on the upper eyelids of the eyes. This is how the doctor checks the density of the eyes and also compares their density. The fact is that in this way it is also possible to diagnose primary glaucoma, in which the pressure in the eyes varies.
For a more accurate diagnosis of intraocular pressure, a tonometer is used. During the procedure, special colored weights are placed on the center of the patient's cornea, the imprint of which is later measured and deciphered. To ensure that the procedure is painless, the patient is given local anesthesia. The norm of intraocular pressure is different for each device. If the procedure is carried out using a Maklakov tonometer, then the normal intraocular pressure is up to 24 mm. rt. Art., but normal pneumotonometer readings are within 15-16 mm. rt. Art.

Diagnostics
To figure out how to treat intraocular pressure, the doctor must not only diagnose it, but also determine the cause of its development.
An ophthalmologist is involved in the diagnosis and treatment of conditions associated with increased or decreased intraocular pressure.
In parallel, depending on the cause of the violations, consultations with the following doctors may be prescribed:
- therapist;
- neurologist and neurosurgeon;
- traumatologist;
- cardiologist;
- endocrinologist;
- nephrologist.
The doctor asks the patient in detail about his symptoms, and then conducts an examination of the fundus. If there are appropriate indications, the patient will be sent for a procedure to measure intraocular pressure.
Treatment of intraocular pressure
The choice of treatment tactics depends on the cause that provoked a decrease or increase in intraocular pressure in an adult.
At increased intraocular pressure The following conservative measures can be used as treatment:
- Drops that improve nutrition of eye tissue and fluid outflow.
- Treatment of the underlying disease if the increase in intraocular pressure is symptomatic.
- If drug methods are ineffective, laser treatment is used.
Here's what you can do when decrease in intraocular pressure:
- Oxygen therapy (use of oxygen).
- Vitamin B1 injections.
- Drops based on atropine sulfate.
- Injections (subconjunctival) of atropine sulfate, dexamethasone or sodium chloride solution.
In general, treatment for low intraocular pressure consists of treating the underlying disease that led to the disorder.
The most radical method of treating intraocular pressure is microsurgical technology: goniotomy with or without goniopuncture, as well as trabeculotomy. During goniotomy, the iridocorneal angle of the anterior chamber of the eye is dissected. Trabeculotomy, in turn, is a dissection of the trabcular meshwork of the eye - the tissue connecting the ciliary edge of the iris to the posterior plane of the cornea.
Prevention
To avoid discomfort in the eye organs, it is necessary to avoid stress and not overwork. If you need to spend a lot of time in front of a monitor screen, you should take five-minute breaks every hour. Closing your eyes, you need to massage your eyelids and walk around the room.
Nutrition is also important. Products should be fresh and healthy; you should avoid those products that can lead to the accumulation of cholesterol. In autumn and winter, it is advisable to take vitamins.