Scheme of drug therapy for nonspecific ulcerative colitis in children. Discussion of treatment of ulcerative colitis. Is it possible to be cured forever?
Suppositories for intestinal colitis are an effective means of improving the patient’s condition. The inflammatory process in the intestines often covers the entire body and can be associated with a number of other diseases characterized by swelling and damage. The suspected cause of this phenomenon is often an autoimmune reaction of the human body.
Among the types of inflammatory diseases intestinal tract highlight:- ulcerative colitis;
- Crohn's disease.
Using suppositories for intestinal colitis helps relieve inflammation and improves the patient's condition.
Any disease of the rectum occurs in a variety of ways, all indicators are personal and depend on:- difficulties ulcerative lesion intestinal tract;
- patient's age;
- other existing diseases.
When the intestines are damaged, the signs can be both very noticeable and mild. In some patients long time the disease does not show itself in any way, only from time to time an exacerbation may manifest itself as blood in the stool. With all this, the patient will be able to associate this indicator with the manifestation of hemorrhoids, and often delays visiting the doctor and conducting a diagnostic examination.
X-ray examination is very important not only for diagnosing the disease, but also for preventing its severe complications.
If the intestinal tract is affected, the patient is hospitalized with the following symptoms:
- fecal incontinence;
- bloody diarrhea;
- temperature;
- weakness;
- pain.
For colitis, treatment should be carried out in medical institution. If the infectious component of the disease is revealed, then in special infectious diseases departments. In this condition, doctors prescribe individual drug treatment. Prescribed drugs often have a huge number of adverse effects and contraindications. They must be used only under medical supervision - these are suppositories, enemas, tablets.
At the moment of choice optimal treatment Colitis of the rectum provides for the specificity of the disease, the degree of damage to the intestinal tract, and the presence of other unfavorable conditions of the digestive system.
To combat harmful organisms that multiply in the intestines, broad-spectrum antibiotics are often prescribed.
The lesion usually affects only colon, and with Crohn's disease, different parts of it can be affected. These diseases manifest themselves as periodic relapses.
Suppositories are perfect for restoring and treating damaged rectal tissue, which will help:
- Accelerate the tissue healing process.
- Stimulate protection at the cellular level.
- Stop the bleeding.
- Reduce inflammation, which is of great importance during illness.
- elimination of inflammation;
- restoration of damaged tissues;
- maintaining remission.
Inexpensive treatment of intestinal diseases takes place in several steps. The first healing period is short, during which time various pharmaceuticals– less aggressive, with the least side effects. If relief does not come, they resort to stronger medications.
In medicine, patients with colon colitis are offered suppositories with different composition and action, therefore, when choosing more effective substances, you can easily get confused. Better to necessary funds prescribed by the attending doctor based on the patient’s medical history and taking into account various side factors.
Suppositories are used rectally, so they have direct action on the inflamed parts of the mucous membrane. The good thing about their use is that they cannot cause the patient to vomit, unlike tablets. Suppositories are also prescribed for lesions in the area anus, hemorrhoids and to ease the act of defecation during constipation.
Medications such as suppositories used to effectively treat colitis usually contain antibiotics that act on infectious inflammation. The suppositories also contain pain-relieving components. Suppositories are produced in the shape of a cone. When used, the required amount of the active drug substance enters the patient’s body.
Suppositories for colitis of the large intestine:
- Salofalk.
- Ultraproct.
- Methyluracil.
- With propolis.
The list of suppositories (their name is above) that have healing properties is unlimited by all the listed medications. To a greater extent, patients will easily find those medications that are suitable for each certain case and not only on the medical advice of the doctor.
But, one way or another, it is worth knowing that even best remedy Although it can simplify the problem, it is not able to completely eliminate the problem of the rectum.
To effectively treat rectal colitis and prevent the occurrence of new ulcerative lesions, it is necessary to use anesthetic rectal suppositories with an analgesic effect, full complex therapeutic measures, and sometimes the most radical methods are needed. Incorrect treatment Intestinal colitis can lead to unpleasant results.
The uncomplicated form of the disease has a good prognosis - almost always the disease can simply be treated with suppositories and goes away without a trace. Medicines used to treat diseases of the intestinal tract play an important role. Using traditional remedies without consulting a doctor can worsen clinical picture and make diagnosis difficult severe form diseases.
Today in pharmacies you can find a large variety of rectal suppositories against colitis with excellent anti-inflammatory effect. They are used to treat the disease. Their action is based on active components that have a positive effect on the body. One of the main components in the treatment and prevention of colitis is diet and consumption of the required amount of vitamins and minerals.
To prevent the onset of the disease, you need to do the following:- to drink a lot of water;
- Healthy food;
- chew food thoroughly;
- follow the doctor's instructions.
If symptoms of the disease occur, the first thing you should do is seek help from a doctor. Only with his approval should you use any treatment methods for this inflammatory disease.
Intestinal colitis is a complex pathology that can lead to the development of serious complications. Therefore, it is important to promptly consult a doctor at the clinic for diagnosis. correct diagnosis and early initiation of treatment.
In any case, treatment should be prescribed by a doctor, since self-medication can be harmful and complicate the condition.
Nonspecific ulcerative colitis (UC) is a chronic inflammatory bowel disease, the etiology of which remains unknown to date. Frequency of nonspecific ulcerative colitis, according to foreign researchers, is 4-10 per 100 thousand children. Difficulties in selecting therapy for UC are associated with a lack of knowledge about the etiology and some links in the pathogenesis of the disease.
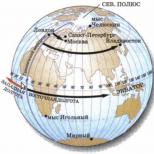
Determining the degree of activity primarily helps in choosing the most optimal treatment regimen for nonspecific ulcerative colitis inflammatory process and its localization. According to the literature, with nonspecific ulcerative colitis, the inflammatory process in 54% of cases is localized in the direct and sigmoid colon, in 28% of cases there is left-sided damage to the colon, and in 18% of patients pancolitis occurs. In children early age(up to three years) the right-sided parts of the colon are predominantly affected.
The degree of activity of nonspecific ulcerative colitis is determined based on the severity of clinical and laboratory parameters. The most pronounced clinical indicators are: diarrhea, blood in the stool, intensity of abdominal pain, weight loss and fever. Laboratory indicators of ulcerative colitis include changes in hemoglobin, albumin, increase in ESR. Currently, there are three degrees of activity of ulcerative colitis: mild, moderate and high (see).
Among the main directions in the treatment of nonspecific ulcerative colitis, nutrition correction and diet therapy should be mentioned. Principles rational nutrition suggest avoiding fried, fatty, salty, spicy foods, milk and dairy products.
Chocolate should not be included in the diet of a sick child. legume products, mushrooms, fruits and vegetables that stimulate peristalsis (plums, kiwi, dried apricots, beets). During periods of exacerbation, the consumption of fiber, sweets, and juices is limited. With long-term remission, the diet can be significantly expanded, but milk and dairy products are contraindicated for the patient throughout his life.
Drug therapy as the main method of treating ulcerative colitis involves the use of:
- preparations of 5-aminosalicylic acid (5-ASA);
- corticosteroids;
- immunosuppressants (cytostatics).
Symptomatic and antibacterial therapy is prescribed to restore the structure of the mucous membrane, normalize peristalsis, restore digestive processes and eubiosis of the colon, and increase the overall immunoreactivity of the body. If diet therapy is ineffective and drug therapy surgical treatment is indicated.
5-ASA drugs are basic in the treatment of ulcerative colitis. In 1942, the drug sulfasalazine was first used in patients with combined damage to the intestines and large joints, which gave a pronounced positive effect: arthralgia and hemocolitis were relieved. Sulfasalazine has been used in the treatment of ulcerative colitis to this day. However, its use is limited due to large quantity side effects such as hemolytic anemia, neutropenia, drug-induced hepatitis, Steven-Johnson syndrome, pericarditis, interstitial nephritis, pancreatitis. The frequency of side effects, according to various authors, ranges from 5 to 55%. Sulfasalazine contains mesalazine (5-aminosalicylic acid), which has an anti-inflammatory effect, and sulfapyridine, which ensures the delivery of mesalazine to the colon,
to the site of localization of the main inflammatory process in nonspecific ulcerative colitis. Sulfapyridine contributes to the development of a large number of side effects. Numerous studies conducted to develop drugs containing mesalazine made it possible in the late 70s and early 80s. create drugs that did not contain sulfapyridine. This has led to a significant reduction in side effects, which in turn has made it possible to use higher doses of mesalazine and, in some cases, eliminate the use of corticosteroids. Mesalazine is active upon local contact with the intestinal mucosa, and its therapeutic efficacy is correlated with the concentration in the intestinal lumen. These features of mesalazine made it possible to develop drugs based on it and successfully use them both in the acute period and for maintenance therapy. local action, such as suppositories, microenemas.
For proctosigmoiditis of moderate and high activity, in addition to local therapy, oral administration of mesalazine or prednisolone in age-specific dosages is indicated. The treatment regimen for proctosigmoiditis is given in.
Pancolitis, or total intestinal damage, usually has a moderate or high degree of activity. In the treatment of pancolitis, mesalazine or sulfasalazine orally and prednisolone in large doses orally or parenterally are used; in the presence of rectal damage, local therapy is indicated (see tables 3 and 4). The treatment regimen for pancolitis in nonspecific ulcerative colitis is presented in Doses of 5-ASA drugs are given for children over 12 years of age. For children under 12 years of age, the dosage of drugs is calculated based on body weight: sulfasalazine - 60 mg/kg/day, mesalazine - 30-40 mg/kg/day.
Tactics for monitoring children with nonspecific ulcerative colitis in the active stage include conducting control blood tests to determine the level of hemoglobin, ESR, leukocytes, total protein and protein fractions once a week active stage and 1 time per month during remission. Colonoscopy and morphological examination are carried out 3 months after the appointment of therapy during exacerbation of the disease, once every 2-3 years - during remission, once a year - when the disease history is more than 8-10 years. Children with inflammatory diseases intestines require long-term medical supervision. If there is remission in spring and autumn, preventive courses of 5-ASA drugs in maintenance doses for 3 months are indicated.
Thus, treatment of nonspecific ulcerative colitis is based on determining the localization of the inflammatory process and the degree of its activity. With a mild degree of activity, the prescription of mesalazine is indicated; moderate and high degrees of activity require the appointment of corticosteroid therapy. If there is no effect from therapy with 5-ASA drugs and steroids and the development of hormonal dependence, immunosuppressive therapy is used. If drug therapy is ineffective, surgical treatment is indicated.
Literature
- Diseases of the digestive system in children (small and large intestines) / Ed. A. A. Baranova, E. V. Klimanskaya. M., 1999. pp. 240-250.
- Shcherbakov P. L. Inflammatory bowel diseases in children: Crohn's disease and ulcerative colitis/ Children's doctor. 2000. No. 4. P. 22-26.
- Beattie RM and others, Endoscopic assessment of colonic response to corticosteroids in children with ulcerative colitis/ /J Pediatr Gastroenterol Nutr. 1996. No. 22. P. 373-379.
- Truelove S. C., Witts L. J. Cortisone in ulcerative colitis: final report on therapeutic trial//Br Med J. 1987. No. 295. P. 517-519.
- Griffiths A. M., Buller H. B. Inflammatopy Bowel Disease. 613-653
- Surikova O. A. Nonspecific ulcerative colitis in children // Children's doctor. 2000. No. 1. P. 45-49.
- Kanshina O. A. Experience in the treatment of nonspecific ulcerative colitis in children and adolescents // Pediatrics. 1992 No. 1. P. 78-82.
- Barden M. E., Lipson A., Pert P., Walker-Smith J. A. Mesalasin in childhood inflammatopy bowel disease//Aliment Pharmacol Ther. 1989. No. 3. P. 597-603.
- Tolia V., Massoud N., Klotz U. Oral 5-aminosalycilic acid in children with colonic chromic inflammatopy bowel disease: clinical and pharmacokinetic experience//Aliment Pharmacol Ther. No. 6. P. 1012-1014.
- Khalif I. L. The use of salicylates in the treatment of nonspecific ulcerative colitis / Attending Physician. 2000. No. 5-6. P. 52.
- Loginov A. S., Parfenov A. I. Intestinal diseases. M., 2000. P. 32.
- Paykov V. L. Pharmacotherapy in pediatric gastroenterology. St. Petersburg, 1998. pp. 188-189.
- Laursen Ls and others: Disposition of 5-aminosalicylic acid by olsalasin and three mesalasin preparation in patients with ulcerative colitis//Gut, 1990. No. 31. P. 1271-1276.
- Rijk MCM and others: Disposition of 5-aminosalicylic acid delivering drugs during accelerated untestinal transit in healthy volunteers // Scand J Gastroenterol, 1989. No. 24. P. 1179-1185.
- Colllins J. R. Adverse reaction to salicylasosulfapyridine in the treatment of ulcerative colitis//South Med J. 1968. No. 61. P. 354-358.
- Loginov A. S., Parfenov A. I., Ruchkina I. N., Krums L. M. The use of salosinal in the treatment of inflammatory diseases of the colon.
- Courtney M. G. and others Randomized comparison of olsalazin in prevention of relapses in ulcerative colitis//Lancet. 1992. No. 339. P. 1079-1281.
- Hardy J. G., Harvey W. J., Sparrow R. A. et al. Localization of drug release sites from an oral sustained formulation of 5-ASA (Pentasa(r)) in the gastrointestinal tract using gamma scintigraphy//J Clin Pharmacol. 1993. No. 3. P. 712-718.
- Stein R. B., Hanauer S. B. Medical therapy for inflammatopy bowel disease//Gastroenterol Clin North Am. 1999. No. 28. P. 297-321.
- Azad Khan AK and others. Optimun dose of sulphasalasine for maintenance treatment in ulcerative colitis//Gut. 1980. No. 21. P. 232-240.
- Baron J.H., Connell A.M., Lennard-Jones J.E. Sulphasalasine and salicylasosulfapyridine in ulcerative colitis/ Lancet. 1962. P. 1094-1096.
- Hanacur S. B. Inflammatopy bowel disease // N Engl J Med. 1996. No. 334. P. 841-848.
- Sutherland L. R., May G. R., Shaffer E. A. Sulphasalasine revisited: a meta-analysis of 5-aminosalicylic acid in the treatment of ulcerative colitis // Ann Inten Ned. 1993. No. 118. P. 540-549.
- Zlatkina A. R. Treatment of chronic diseases of the digestive system. M., 1994. pp. 163-217.
- Belaiehe J., Louis E. Corticosteroids treatment in active Crohn's disease//Asta Gastroenteerol Belg. 1998. No. 61(2). P. 153-157.
- Kusunoki M. and others. Steroid complications in patients with ulcerative colitis//Dis Colon Rectum. 1992. No. 35. P. 1003-1009.
- Alieva E. I., Khalif I. L., Mazankova L. N. Conservative treatment of nonspecific ulcerative colitis in children // Children's doctor. 2001. No. 2. P. 36-42.
- Kopeikin V.N. Mechanisms of formation and optimization system for the treatment of nonspecific ulcerative colitis in children: Abstract of thesis. dis. ... doc. honey. Sciences, M., 1996.
- Compston J. E. Corticosteroids and growth//J Pediatr. 1998. No. 113. P. 249-254.
- Verhave M., Winter H. S., Grand R. J. Azathioprine in treatment of inflammatopy bowel disease//J Pediatr. 1998. No. 117. pp. 809-814.
- Egan L. J., Sandorn W. J. Metotrexate for inflammatopy bowel disease//Mayo Clin Proc. 1996. No. 71. P. 69-80.
- Treem W. R. and others. Cyclosporine for the treatment of fulminant ulcerative colitis in children//Dis Colon Rectum. 1995. No. 38. P. 474-479.
- Aranda R., Horgan K. Immunosuppressive drugs in the treatment of inflammatopy bowel disease//Semin Gastrointest Dis. 1998. No. 9. P. 29.
E. G. Tsimbalova, Candidate of Medical Sciences
A. S. Potapov
P. L. Shcherbakov, Doctor of Medical Sciences
SCCD RAMS, Moscow
Suppositories for colitis are a popular dosage form due to the direct effect of medicinal components on inflammatory foci. Suppositories have a minimum of contraindications, are practically not absorbed into the systemic bloodstream, and do not directly affect the functionality of internal organs.
All drugs in the form of suppositories for colitis and intestinal inflammation have anti-inflammatory, antimicrobial and regenerating effects, which significantly facilitates the course of the disease and quickly reduces the intensity of symptomatic manifestations. Correct Application rectal suppositories relieve the patient’s condition within a few days.
Rectal suppositories are easily inserted into the rectal space and begin to act almost immediately after dissolution
Benefits of rectal suppositories
Unlike local and systemic drugs for proctitis and colitis, rectal suppositories are effective against any form of inflammation of various parts of the intestine, due to the targeted effect of active medicinal components.
The drugs directly affect the affected area, disinfect and create a protective film on the mucous membranes. The main advantages of rectal suppositories are:
- absence negative influence on gastrointestinal microflora;
- maintaining the therapeutic effectiveness of the drug components inside the intestine;
- speed of directed influence;
- ease of use in children and adults;
- dosage accuracy.
Suppositories for treating the intestines are easily inserted into the anus without causing any discomfort.
Important! Despite the absence absolute contraindications, independent use of drugs is unacceptable. Inadequate dosage can contribute to traumatization of mucous membranes, persistent diarrhea and complicate the recovery process.
Popular and effective means
So, which intestinal suppositories should you choose to relieve inflammation and speed up the healing of affected areas of the mucous membranes? The choice of drugs for the treatment of colon colitis is usually determined by the form, severity and stage of the disease, and the symptomatic complex. At inflammatory lesion intestines the most effective are the following medications:
- Suppositories Relief. The drug copes well with pain, eliminates bleeding in ulcerative colitis of the intestine, paraproctitis. The suppositories contain shark liver oil, which has a beneficial effect on the intestinal mucosa, promotes rapid regeneration, restoration and healing.
- Salofalk. The drug is used for severe inflammation of the walls intestinal sections, reducing swelling, painful syndrome, bleeding. The components of the product protect the mucous membranes from damage, creating a protective film on the affected area. Candles are used 3 times a day, laying cotton swab into the anus after inserting a suppository.
- Ultraproct. Hormonal suppositories for intestines against inflammation with the active ingredient - fluocortolone. The drug reduces pain, swelling, eliminates severe itching, relieves problems with bowel movements, especially colitis with constipation. Being hormonal agent, the drug should be taken under the mandatory supervision of the attending physician.
- Viburkol. Homeopathic medicine for administration in colitis with constipation and defecation disorders. The product perfectly restores intestinal function in case of colitis and hemorrhoids. Viburkol has antipyretic, antispasmodic, analgesic effects. Due to the natural nature of the drug, suppositories can be used by young children, pregnant and lactating women.
- . The suppository contains the analgesic Lidocaine, bismuth, titanium dioxide and bufexamac. The analgesic and anti-inflammatory effect for colitis is achieved in any form of the disease. All these components have a drying effect astringent action, anti-inflammatory effect. After using Proctosan suppositories, the first results are felt on days 3-5 of regular use. 2 suppositories per day are enough.
- Diclofenac. A well-known pain reliever that eliminates not only painful syndrome, but also improves the condition of the intestinal mucous membranes. Contains suppository active substance diclofenac and solid fats. Prescribed when acute colitis intestines of any form and for the treatment of ulcerative colitis during an exacerbation. The drug is effective against ulcerative colitis with signs of bleeding.
- Natalsid. Suppositories for stopping bleeding in all forms of colitis. The drug is effective for colitis with stool disorders. The hemostatic drug is based on brown seaweed, which not only affects the source of bleeding, but also stimulates the regeneration of mucous tissues, reducing the inflammatory focus.
- Papaverine. Antispasmodic suppositories to eliminate pain in acute colitis against the background of increased muscle contractility. The use of the drug is symptomatic only. Papaverine not only eliminates spasms, but also has a pronounced analgesic effect.
Important! All anti-inflammatory suppositories for inflammation of the rectum should be prescribed only after consultation with a doctor. Given the diversity of manifestations of colitis, symptomatic manifestations differ in each case.
Other effective remedies
Other medicines for colitis include inexpensive and effective suppositories for colitis based on natural ingredients, as well as those that have found their use in various areas medicine and cosmetology. Among the wide-profile medicinal suppositories highlight:
- Ichthyol candles. Contains anti-inflammatory rectal suppositories the natural component is ichthammol, and vitepsol is considered an auxiliary component. Ichthyol suppositories for colitis have a healing and restorative effect on the affected areas of the intestine. Two suppositories per day are enough to eliminate unpleasant symptoms associated with colitis.
- Methyluracil suppositories. A drug from the sulfonamide group, they are sulfonamide suppositories. The action of the active components of the drug is aimed at suppressing the inflammatory focus and activating metabolic processes in the affected mucous membranes. Methyluracil suppositories for intestinal colitis stimulate the regenerative activity of mucosal cells and accelerate the synthesis of red blood cells. After just a few days, bleeding decreases, swelling and pain decrease.
- Propolis based suppositories. Natural components in propolis suppositories accelerate the restoration of mucous membranes, soften the intestinal lining, relieve pain and eliminate pathological processes. Despite absolute safety, the use of propolis suppositories for colitis can cause allergic reactions, especially in young children.
- Sea buckthorn candles. Sea buckthorn oil in the composition of the drug has an excellent disinfecting and anti-inflammatory effect. Sea buckthorn absorbs fatty acids, thereby accelerating the restoration of the mucous epithelium. The use of suppositories with sea buckthorn oil eliminates swelling, itching, and improves vascular conductivity in the affected area. The course of use is 14 days, 2 suppositories per day.
About drugs for the treatment of hemorrhoids and intestinal inflammation in E. Malysheva’s program on health:
Colitis is an inflammatory disease that affects the mucous membrane of the intestinal canal.
The symptoms of the disease are very similar to many ailments. But its signs must be determined as soon as possible, otherwise complications will arise. One of the treatment methods is the use of suppositories.
What drugs can be used for intestinal colitis?
Advantages of using suppositories for colitis
Suppositories are a popular form medicines. When using them, it is possible to obtain a quick positive result. In addition to all this, they have a minimum of contraindications, since they do not enter the systemic bloodstream and do not affect the functioning of internal organs.
They are prescribed for intestinal colitis in children and breastfeeding. The suppositories are absolutely safe and act directly on the source of the inflammatory process.
Medicines used to treat intestinal colitis have a regenerating and healing effect, which is aimed at relieving tissue swelling and painful sensations, elimination pathological process, facilitating the process of defecation.
Anti-inflammatory drugs
Nowadays, there are a wide variety of treatment methods. One of the safest and most popular is the use of candles. Colon disease is a disease that can affect a person at any age and position.
To prevent the development of further pathological process, patients are advised to use suppositories with an anti-inflammatory effect.
There are several effective means.
Viburkol
A drug from the homeopathic group, which is used to eliminate dyspeptic symptoms when the intestinal canal is disrupted. The medication also has sedative, anesthetic, antispasmodic and antipyretic properties.

When using Viburkol suppositories, the load on neighboring organs is reduced. Symptoms of intoxication quickly disappear and the acute course of the disease passes.
This drug is approved for use in children from birth, women during pregnancy and breastfeeding.
The average cost of suppositories ranges from three hundred and fifty rubles.
Fitor
To treat the inflammatory process of the rectum, Fitor suppositories are often prescribed. The drug is considered a biologically active complex that has wide range impact.
The composition of the medicine includes tanning components, flavonoids, vitamins and acids. Thanks to such substances, they have bactericidal, biostimulating, antioxidant, wound-healing and antiprotective properties.
Phytor suppositories allow you to quickly and painlessly remove all poisons and toxic components from the body.

The medication has no restrictions, and therefore is prescribed to expectant mothers, nursing women and children at any age. Duration therapeutic therapy ranges from ten to twenty days.
What is noteworthy is that these suppositories are quite inexpensive, around one hundred and fifty rubles. Therefore, they are available to every patient.
Proctosan
To treat the rectum, suppositories in the form of Proctosan are often prescribed. The medication has a local anesthetic, drying, astringent and anti-inflammatory effect.
The basis of the drug is bufexamac, titanium dioxide, bismuth, lidocaine. To ensure that the suppositories quickly dissolve in the rectum, liquid paraffin, lanolin and water are added to them.

Duration treatment course ranges from eight to ten days.
But the medicine has a number of limitations such as:
- childhood;
- period of pregnancy and breastfeeding;
- the presence of inflammatory processes in the body in the form of tuberculosis and syphilis;
- increased sensitivity to the components of the product.
According to patient reviews, symptomatic relief occurs within three to five days. A average cost is four hundred rubles.
Suppositories with analgesic effects
When the intestinal canal is affected, patients always feel a strong painful feeling. These symptoms have a negative impact on general condition the patient and his ability to work.
That is why prescribed suppositories for intestinal colitis should have an analgesic effect.
In pharmacology, several names of medications are offered.
Diclofenac
Drugs that have a good analgesic effect. Allows you to quickly eliminate pain in the rectal area. The drug contains only two components: diclofenac and solid fat.

The product belongs to the group of inexpensive, but fast-acting. Recommended in case of acute illness. In this case, the duration of the treatment course should not exceed three days.
It has a number of limitations such as:
- ulcerative colitis of the intestinal canal;
- kidney diseases;
- gestation period in the first and second trimester;
- children under fourteen years of age;
- increased susceptibility to the components of the drug;
- development of hypokalemia;
- liver diseases.
Diclofenac should be administered with extreme caution in cases of severely weakened immune function and in old age. They should be used only after consulting a doctor.
To treat the disease in the acute phase in the presence of spasms, it is recommended to use Papaverine suppositories. The medicine is inexpensive, but has a good analgesic and antispasmodic effect.

Papaverine has a minimum of contraindications and can be used in babies older than six months, pregnant and lactating women. Its effect is compared with No-Shpa and Drotaverine, but the suppositories act much faster on the source of pain.
It has a number of limitations such as:
- increased sensitivity to the components of the drug:
- glaucoma;
- severe liver failure.
The duration of the treatment course should not exceed three days.
Glucocorticosteroid suppositories
Often, suppositories based on glucocorticosteroids are prescribed for the treatment of the rectum. An effective remedy This group is represented by Ultraprokt.
The main component of the medication is fluocortolone. It has anti-inflammatory, local anesthetic, antipruritic and antiallergic properties.

Since the main substance is a hormonal substance, it is prohibited to use it for:
- the presence of viral diseases;
- the presence of syphilis or tuberculosis;
- children under eighteen years of age;
- first trimester of pregnancy;
- increased sensitivity to the components of the drug.
The medicine is prescribed with extreme caution in the second and third trimester of pregnancy and during breastfeeding.
Other medicines
If colitis occurs in children under the age of ten, during pregnancy or breastfeeding, then doctors prescribe safer products based on natural ingredients.
Natalsid
Suppositories with a hemostatic effect. They are prescribed for severe damage to the intestinal canal, which is accompanied by bleeding.
The main component is brown seaweed, which has anti-inflammatory, hemostatic and reparative effects.

They are effective for colitis chronic type, which is characterized by periodic exacerbations.
There are a number of restrictions in the form of children under fourteen years of age and increased susceptibility to the components of the medication.
Methyluracil suppositories
A drug that allows you to instantly activate metabolism in affected tissue structures and stimulate regenerative processes.
The effect of the drug is aimed at accelerating the formation of red blood cells, due to which bleeding stops and the inflammatory process disappears.
It is not recommended to insert suppositories into the rectum if:
- the presence of malignant tumors in the bone marrow;
- leukemia;
- hemoblastoses;
- lymphogranulomatosis;
- children under three years of age;
- increased sensitivity to the components of the drug.
During pregnancy and breastfeeding this type suppositories can be used, but the dosage should only be prescribed by a doctor, assessing the risks to fetal development.

To the very safe means can be attributed:
- Propolis based candles. The main component of the drug is a beekeeping product. Although they are safe, they can cause allergic reactions. Their effect is aimed at pain relief, accelerating regeneration, and relieving the pathological process.
- Candles based on sea buckthorn. The main component of the medicine is sea buckthorn oil. It has good anti-inflammatory, antibacterial and healing properties. Treatment with this drug consists of resorption fatty acids, which are necessary during recovery stage. In addition to all this, suppositories allow you to resume the functioning of the vascular system, relieve swelling, relieve itching and speed up the healing of cracks.
This type of suppositories can be purchased independently, as they have no contraindications and can be used by children, pregnant and nursing mothers.
Suppositories for ulcerative colitis
If a patient has ulcerative colitis, then the damage is observed not only in the large intestine, but also in small intestine. In this case, the inflammatory process can spread further to other organs of the digestive system.

The treatment process in this situation is:
- suppression of the pathological process;
- elimination of disease symptoms;
- restoration of intestinal tissues.
For ulcerative colitis, therapeutic measures must be carried out not only during the period of exacerbation, but also during remission. This process is called chronic.
So that relief comes much faster doctors strong medications are prescribed.
This may include:
- aminosalicylates. This type of suppository belongs to the aspirin group. These include Pentaza, Asokol, Dipentum;
- immunomodulatory agents. Their effect is aimed at lowering the level of lymphocytes in the blood. The effect of such drugs occurs within two to four weeks. Therefore, they should be taken for quite a long time. This includes Imuran;
- suppositories based on bifidobacteria. They restore the microflora of the intestinal canal. These include Bifidumbacterin suppositories. In some cases, experts advise giving enemas with solutions that contain lactobacilli.
Medicines in the form of suppositories are not limited in choice. They are produced for any type of symptomatology, and many of them have practically no restrictions.
Side effects
When using suppositories in some situations, side effects may occur in the form of:
- development of painful sensations in the head;
- dizziness;
- diarrhea or constipation;
- irritability skin around the anus;
- development of pancreatitis or hepatitis;
- increased heart rate.
If there is increased sensitivity to the components of the product, the patient may develop allergic reactions in the form of redness, rashes, itching and burning.
Suppositories are among the safest and fastest methods of treatment. They act directly on the intestinal canal and cause minimal side effects and have virtually no restrictions. But in any case, you need to consult a specialist.
Therapeutic tactics for ulcerative colitis are determined by the localization of the pathological process in the colon, its extent, the severity of the attack, and the presence of local and/or systemic complications. Conservative therapy is aimed at stopping the attack as quickly as possible, preventing relapse of the disease and progression of the process. Distal forms of ulcerative colitis - proctitis or proctosigmoiditis - are characterized by more light current Therefore, they are most often treated on an outpatient basis. Patients with left-sided and total lesions are usually treated in a hospital, since the course of the disease in them is more severe clinical symptoms and major organic changes.
The food of patients should be high in calories and include foods rich in proteins, vitamins, with a limitation of animal fats and the exclusion of coarse vegetable fiber. Recommended low-fat varieties fish, meat (beef, chicken, turkey, rabbit), boiled or steamed, pureed cereals, potatoes, eggs, dried bread, walnuts. Raw vegetables and fruits are excluded from the diet, as they contribute to the development of diarrhea. Patients often have lactase deficiency, so dairy products are added only if they are well tolerated. These recommendations correspond to diets 4, 4B, 4B of the Institute of Nutrition of the Russian Academy of Medical Sciences.
All medications used in treatment regimens for ulcerative colitis can be divided into two large groups. The first combines basic anti-inflammatory drugs and includes aminosalicylates, i.e. drugs containing 5-aminosalicylic acid (5-ASA, mesalazine), corticosteroids and immunosuppressants. All other drugs play either an auxiliary role in the treatment of ulcerative colitis or are at the stage of clinical study.
The first drug containing 5-ASA was sulfasalazine (salazosulfapyridine), which was introduced into clinical practice in 1942. Sulfasalazine consists of two components linked by a nitrogen bond - sulfapyridine sulfanilamide and 5-ASA. It has been proven that only 5-ASA has an anti-inflammatory effect. Sulfapyridine was forced into the composition of the sulfasalazine molecule, since “pure” 5-ASA is well absorbed in the small intestine, and in the mucous membrane it turns into an inactive metabolite - N-acetyl-5-ASA. In sulfasalazine, sulfapyridine acts solely as a “carrier” that allows delivery of 5-ASA to the affected areas of the colon. Under the influence of colonic microflora, the nitrogen bond is destroyed. Sulfapyridine is absorbed in the colon, undergoes detoxification in the liver through acetylation and is excreted in the urine, and 5-ASA, in contact with the mucous membrane, has an anti-inflammatory effect.
The mechanisms by which 5-ASA exerts its anti-inflammatory effect are not fully understood. Nevertheless, numerous effects are known due to which mesalazine inhibits the development of inflammation. Thus, by inhibiting cyclooxygenase, mesalazine inhibits the formation of prostaglandins. The lipoxygenase pathway of arachidonic acid metabolism is also suppressed, and the release of leukotriene B4 and leukotriene sulfopeptide is inhibited.
At high concentrations, mesalazine can inhibit certain functions of neutrophil granulocytes in humans (eg, migration, degranulation, phagocytosis, and the formation of toxic oxygen free radicals). In addition, mesalazine inhibits the synthesis of platelet-activating factor. Due to its antioxidant properties, mesalazine is able to scavenge free oxygen radicals.
Mesalazine effectively inhibits the formation of cytokines - interleukin-1 and interleukin-6 (IL-1, IL-6) - in the intestinal mucosa, and also suppresses the formation of IL-2 receptors. Thus, mesalazine interferes directly with immune processes.
The "bullet" component sulfapyridine has been shown to be primarily responsible for the overall incidence of sulfasalazine side effects. Literature data on the frequency of side effects caused by sulfasalazine range from 5 to 55%, averaging 21%. In addition to nausea, headache, male infertility, anorexia, dyspeptic disorders, hematological reactions (leukopenia and hemolytic anemia) and hypersensitivity reactions with multiple organ lesions occur.
In order to maintain the anti-inflammatory activity inherent in sulfasalazine and avoid the side effects associated with the sulfapyridine component, preparations containing “pure” 5-ASA have been developed in recent years. An example of a new generation of aminosalicylates is the drug salofalk, developed by the German pharmaceutical company Doctor Falk Pharma. The drug is available in three dosage forms: tablets, suppositories and microenemas. In tablets, mesalazine is protected from contact with gastric contents using a special acid-resistant polymer shell, which dissolves at pH levels above 6.5. These are the pH values that are usually recorded in the lumen ileum. After dissolution of the membrane, a high concentration of the active anti-inflammatory component (mesalazine) is created in the ileum. Selecting a specific dosage form Salofalk is determined by the extent of the zone of inflammation in the large intestine. For proctitis, it is advisable to use suppositories, for left-sided lesions - microenemas, and for total colitis - tablets.
Pentasa, which recently appeared in Russia, while being just as effective, has a number of features. It differs from other mesalazine preparations in its microgranular structure and the nature of its coating. Pentasa tablets consist of microgranules in an ethylcellulose coating, the dissolution of which does not depend on the pH level in the gastrointestinal tract. This ensures a slow, gradual and uniform release of 5-ASA throughout the intestinal tube, starting from duodenum. The uniformity of release contributes to a constant concentration of the drug in different departments intestines, which does not depend not only on pH, but also on the transit rate, so pentasa can be successfully used for inflammatory bowel diseases with diarrhea with virtually no losses. These features make it possible to use the drug not only for ulcerative colitis and Crohn's disease with damage to the colon and ileum, but also, most importantly, in patients with high-intestinal localization of Crohn's disease.
Daily dose aminosalicylates is determined by the severity of the attack of ulcerative colitis and the nature of the clinical response to the drug. To stop an acute and moderate attack, 4-6 g of sulfasalazine or 3-3.5 g of mesalazine per day are prescribed, divided into 3-4 doses. In the absence of a good clinical response, the daily dose of mesalazine can be increased to 4.0-4.5 g, however, it is usually not possible to increase the daily dose of sulfasalazine due to the development of severe side effects.
Sulfasalazine blocks folic acid conjugation in the brush border jejunum, inhibits the transport of this vitamin, inhibits the activity of the enzymatic systems associated with it in the liver. Therefore, the treatment complex for patients with ulcerative colitis receiving treatment with sulfasalazine must include folic acid at a dose of 0.002 g 3 times a day.
It usually takes 3 to 6 weeks to stop an attack of ulcerative colitis. After this, anti-relapse treatment is carried out with sulfasalazine (3 g/day) or mesalazine (2 g/day).
Of the modern drugs for the treatment of proctosigmoiditis and left-sided colitis, the suspension of salofalk is most often used. Disposable containers contain 4 g of mesalazine in 60 ml of suspension or 2 g of mesalazine in 30 ml of suspension. The drug is administered into the rectum 1-2 times a day. The daily dose is 2-4 g, depending on the severity of the process in the intestine. If the extent of the inflammatory process in the rectum is no more than 12 cm from the edge of the anus, it is advisable to use salofalk suppositories. The usual daily dose in these cases is 1.5-2 g.
When using aminosalicylates, it is possible to achieve remission in 75-80% of cases of ulcerative colitis.
The most effective anti-inflammatory drugs in the treatment of ulcerative colitis remain steroid hormones, which in severe forms of the disease are superior in activity to aminosalicylates. Corticosteroids accumulate in inflammatory tissue and block the release of arachidonic acid, preventing the formation of prostaglandins and leukotrienes, which cause the inflammatory process. By blocking chemotaxis, steroid hormones indirectly exhibit an immunomodulatory effect. The effect on tissue fibrinolysis leads to a decrease in bleeding.
Acute severe and moderate forms of the disease and the presence of extraintestinal complications;
Left-sided and total forms of ulcerative colitis with severe and moderate course if present III degree activity of inflammatory changes in the intestine (according to endoscopic examination);
Lack of effect from other treatment methods for chronic forms of ulcerative colitis.
In acute severe form of ulcerative colitis or severe attack of chronic forms of the disease, treatment should begin with intravenous administration prednisolone at least 120 mg/day, evenly distributed over 4-6 injections with simultaneous correction water and electrolyte disturbances, administration of blood and blood substitutes and (if possible) hemosorption in order to quickly eliminate endotoxemia. The hydrocortisone suspension should be administered intramuscularly, but the duration of such administration is limited to 5-7 days due to the likely development of abscesses at the injection sites and possible fluid retention. After 5-7 days, you should switch to oral prednisolone. During this time, a gastroscopy is performed to exclude peptic ulcer stomach and duodenum. In case of moderate form and absence of clinical signs, as well as anamnestic indications of gastroduodenal ulcers, treatment should begin immediately with oral administration prednisone. Typically, prednisolone is prescribed at a dose of 1.5-2 mg/kg body weight per day. A dose of 100 mg should be considered the maximum.
If hormonal drugs are well tolerated, it is recommended to take the prescribed dose until stable positive result- within 10-14 days. After this, a reduction is carried out according to the so-called stepwise scheme - by 10 mg every 10 days. Starting from 30-40 mg, a single dose of prednisolone in the morning is recommended, which practically does not cause serious complications. At the same time, mesalazine or sulfasalazine is included in the treatment regimen, which should be taken until the hormones are completely withdrawn. Starting from 30 mg, prednisolone is withdrawn more slowly - 5 mg per week. Thus, full course Hormonal therapy lasts from 8 to 12 weeks. depending on the form of ulcerative colitis.
In distal forms of the lesion and I-II degrees of process activity according to sigmoidoscopy data, hydrocortisone should be prescribed rectally by drip or in microenemas. Moreover, if patients have difficulty maintaining large volumes, then the administration of hydrocortisone (65-125 mg) should be started in 50 ml of isotonic sodium chloride solution and, as the inflammation subsides and the frequency of false urges decreases, gradually increase the volume to 200-250 ml per therapeutic enema. The drug is usually administered after bowel movements in the morning or before bed.
For ulcerative proctitis and sphincteritis, suppositories with prednisolone (5 mg), administered 3-4 times a day, have a fairly good effect. In more severe distal forms, accompanied by increased body temperature, general weakness, anemia and III-IV degrees of activity according to rectoscopy, in cases of no effect from sulfasalazine or mesalazine, treatment with oral prednisolone at a dose of 30-50 mg/day is indicated.
In middle-aged and elderly patients, the dose of prednisolone should not exceed 60 mg, since they are characterized by the presence concomitant diseases: atherosclerosis, hypertonic disease, diabetes mellitus, etc. In cases where ulcerative colitis occurs against the background of atherosclerotic lesions of the mesenteric arteries, it should be included in the treatment complex vascular drugs: trental, prodectin, etc.
Hormone therapy is associated with the development of side effects: retention of fluid, chlorides and sodium in tissues (swelling is possible), arterial hypertension, hypokalemia, calcium loss, osteoporosis, various autonomic disorders, violation carbohydrate metabolism, adrenal insufficiency, stomach ulcers, gastrointestinal bleeding. In these cases, it is recommended to prescribe adequate symptomatic therapy: antihypertensive drugs, diuretics, calcium supplements, antacids. If carbohydrate metabolism is impaired, a diet with limited carbohydrates is necessary; according to indications, fractional administration of insulin (according to glycemia) or oral antidiabetic drugs. To prevent the development of thrombosis in patients with severe forms of ulcerative colitis receiving hormonal treatment, should be carried out constant control blood coagulation system and simultaneously prescribe antiplatelet agents: chimes, prodectin, etc.
ACTH-zinc phosphate is effective only in the acute form of ulcerative colitis, since its effect is mediated by the preserved function of the own adrenal glands. The drug is administered intramuscularly at a dose of 20-40 mg, depending on the severity of the attack.
In recent years, in the treatment of inflammatory bowel diseases, especially Crohn's disease, drugs containing active component glucocorticosteroid budesonide. Unlike traditional glucocorticosteroids, budesonide has a very high degree of affinity for receptors and high (about 90%) first-pass metabolism in the liver. Due to this, it has a very powerful local anti-inflammatory effect with a minimum number of systemic side effects. As an alternative to prednisolone and hydrocortisone, the drug budenofalk can be recommended. When developing the structure of budenofalk, the physiological characteristics of the gastrointestinal tract were taken into account. Each capsule of budenofalk contains about 350 microspheres consisting of budesonide coated with a polymer shell that is resistant to gastric juice. Release of budesonide from microspheres occurs in the ileum and colon at pH values above 6.4. Budenofalk is used to treat mild and moderate exacerbations of ulcerative colitis. The recommended daily dose is 1 capsule of budenofalk containing 3 mg of budesonide, 4-6 times a day.
The most serious problem in the treatment of ulcerative colitis is hormonal dependence and resistance. This group of patients has worst results conservative therapy and the highest surgical activity. According to the State Scientific Center for Cancer Research, hormonal dependence develops in 20-35% of patients with severe ulcerative colitis. Often, signs of dependence and resistance are observed simultaneously, forcing one to resort to unsafe and aggressive methods of influence.
Hormonal dependence is a reaction to glucocorticoid therapy, in which the positive therapeutic effect is replaced by reactivation of the inflammatory process due to dose reduction or withdrawal of corticosteroids. This is a special variant of refractory colitis. We believe that there are at least 4 different etiopathogenetic variants of hormonal dependence: true hormonal dependence, combined with steroid resistance, false, caused by inadequate treatment, chronic adrenal insufficiency itself, and a mixed or combined form.
Currently, the causes and mechanisms of the formation of hormonal dependence are completely unknown. Nevertheless, we believe that among the etiological factors, defects in hormonal therapy itself, persistent inflammatory activity, and a transient or persistent decrease in the function of the pituitary-adrenal system will undoubtedly find their place. Probably, in some cases, hormonal dependence and resistance are hereditary, in others they represent an acquired defect in hormonal receptors and an imbalance between proliferation and cell death, i.e., deregulation of apoptosis. The hypothesis of a low density of hormonal receptors in patients with inflammatory diseases of the colon, especially with refractory disease, has recently received convincing confirmation.
It is immunosuppressants that play a responsible role in the treatment of patients with inflammatory diseases of the colon with hormonal dependence and resistance. However, this role for various drugs is assessed ambiguously. First-line and long-term drugs include 6-mercaptopurine and azathioprine. They are excellent sparring partners for glucocorticoids. Purine analogues make it possible to reduce and cancel hormones in 60-70% of patients with hormonal dependence, subject to certain rules, namely: they must be prescribed simultaneously with hormones so that their effect has time to manifest itself. The daily dose of azathioprine should be no more than 150 mg. The effect can be expected only by the end of the 3rd month of continuous use. Purine analogues produce relatively few side effects, and they should be used in patients with hormonal dependence for as long as possible - 2-3 years or more.
The 2nd line drug for long-term therapy is methotrexate, which is used in cases of intolerance to azathioprine or the need to accelerate the effect. It is administered orally or intramuscularly at a dose of 30 mg/week. The result can be obtained in 2-4 weeks. Side effects are few. Unfortunately, like azathioprine, it does not provide a lasting effect. Exacerbations occur upon withdrawal. Outbreaks that are milder than before sometimes occur during therapy after 6 months. from the start of the reception.
Cyclosporine can be used orally, intravenously at a dose of 4-6 mg/kg body weight with good and quick effect, coming in 5-7 days. The action is short-lived. It is more often used to interrupt an attack with a subsequent transition to immunosuppressants suitable for prolonged use.
Violation barrier functions colon in ulcerative colitis may cause the development of toxemia syndrome. To correct it, it is necessary to prescribe an appropriate complex, restore eubiosis, antibacterial therapy, hemosorption, and ultraviolet irradiation of autologous blood.
Due to pronounced metabolic disorders and catabolic action of steroid hormones is advisable parenteral administration protein preparations: serum albumin, plasma protein, essential amino acids.
To improve the processes of microcirculation and transcapillary exchange, the administration of rheopolyglgine and hemodez (in normal dosages) is indicated.
In case of anemia (hemoglobin 90 g/l and below), which is a sign of a severe attack of ulcerative colitis, it is recommended to carry out blood transfusion of 250 ml of same-type blood with an interval of 3-4 days. When the level of iron in the blood serum decreases, it is necessary to include iron supplements in the treatment complex.
Taking into account the immunological disorders in ulcerative colitis, immunomodulators, levamisole, thymalin, etc. are used in the treatment of the disease. However, their role is not completely clear, the therapeutic effect of their use is short-term, so the activity of these drugs as basic agents is doubtful.
Vitamins of groups B, C, A, D, K are prescribed, which also help restore eubiosis in the intestines.
The treatment complex includes psychotropic drugs in usual dosages, focusing on individual tolerance.
Exacerbation of ulcerative colitis in in some cases accompanied by irritable bowel syndrome, most often manifested by constipation. In this case, the appointment is justified wheat bran or patented preparations containing ballast substances (mucofalk, etc.), which help normalize stool and at the same time act as enterosorbents.
Inpatient treatment ends when clinical-endoscopic remission is achieved, after which the patient is subject to dispensary observation in a clinic with a general practitioner, gastroenterologist or proctologist.
Articles on the topic
We will answer your questions and select a specialist