The first signs of fetal hemolytic disease on ultrasound. Hemolytic disease of the fetus and newborn (HDN). Clinical recommendations. Hemolytic disease of the newborn. Treatment
One of the most severe childhood pathologies is hemolytic disease of newborns (HDN), which occurs when the immune systems of mother and child conflict, which is accompanied by massive destruction of red blood cells. Therefore, this disease of the fetus and newborn is also known as erystoblastosis - This is a sad result of the categorical differences in the blood of mother and baby according to the Rh or ABO system.
The main cause of erythroblastosis in an infant is the opposite difference in the blood of mother and baby, often in the Rh factor. More rarely, the culprits are blood group antigens (in the ABO system), and less often they encounter opposition of a different nature.
What is the predisposition to Rh conflict between mother and baby? When a mother with minus rhesus is pregnant with a baby with plus rhesus. Most often, this is why hemolytic disease of newborns manifests itself, starting development already in the womb.
The reason for the clash of immunities in the ABO system is a mismatch in blood groups: O(1) blood group in the mother and A(2) or B(3) in the fetus.
It is worth noting that a child is not always born sick. And only when the mother had previously experienced so-called sensitization, that is, increased sensitivity to foreign blood components that she encountered for one reason or another.

Maternal sensitization can have different sources. For example, a mother who is Rh negative becomes sensitized after receiving a transfusion of Rh positive blood (this could have happened a long time ago, even when she was a child). In addition, sensitization occurs during a miscarriage, and if there was an induced abortion. Also, the main culprits of maternal sensitization are childbirth. Therefore, with each subsequent child the risk increases.
If we are talking about immune incompatibility according to the ABO system, it does not matter what kind of pregnancy a woman has, since we are faced with sensitization to antigens every day - when eating, with vaccinations, during some infections.
In addition to the above-mentioned discrepancies in the Rh factor and the ABO system, the placenta occupies a special place, since it provides direct contact between the organisms of the mother and the baby when he is in the womb. When the barrier itself is broken, the exchange of antibodies and antigens in the bloodstreams of mother and baby occurs more easily.
During the prenatal period, hostile blood bodies penetrate inside along with red blood cells. These bodies (Rh factor, antigens A and B) promote the formation of antibodies in the blood, and they then penetrate the protective barrier into the bloodstream of the pregnant baby. The result of this exchange is the combination of antigens and antibodies, causing pathological destruction of red blood cells.
The consequences of such destruction with the participation of hostile bodies have a detrimental effect on the development of the fetus. One of the consequences of this breakdown is an increase in the concentration of toxic bilirubin and the development of anemia (anemia).
Bilirubin that has not passed through the liver is toxic to humans, and even more so to an infant. It has the ability to overcome the obstacle separating the circulatory system and the central nervous system, and also causes damage to the subcortical nuclei and cerebral cortex, which is the cause of “kernicterus.”
If it has developed, then as a result of the destruction of red blood cells, new blood cells are formed - erythroblasts. Therefore, this disease is also called erythroblastosis.
Forms
Depending on the type of immunological conflict, the following forms are distinguished:
- Hemolytic disease of newborns due to Rh factor conflict;
- Hemolytic disease of newborns due to blood group conflict (ABO incompatibility);
- More rare forms (conflict with other antigenic systems).
Clinical forms:
- Edema;
- Jaundice;
- Anemic.
Based on severity, the following forms of the disease are distinguished:
- Mild: symptoms are moderate or there are only laboratory indicators.
- Moderate: bilirubin in the blood is increased, but intoxication and complications have not been identified. In the first 5–11 hours after the birth of the baby, it appears (depending on the Rh or ABO conflict), in the 1st hour of life it is less than 140 g/l, bilirubin in the blood from the umbilical cord exceeds 60 µmol/l, the liver and spleen are enlarged in size.
- Severe: edematous form of the disease, symptoms of kernicterus, respiratory and cardiac function disorders.
Symptoms
Clinical symptoms vary depending on one form or another of pathology: edematous, anemic or icteric.
Edema
The edematous form, similarly called hydrops fetalis, is the most rare, and is superior to all others in the severity of the disease. Here are its signs and symptoms:
- The beginning of development is intrauterine;
- High probability of miscarriage in the first trimester of pregnancy;
- Less commonly, later fetal death or birth in an aggravated position with edema characteristic of this form, a profound deficiency of hemoglobin and red blood cells in the bloodstream, with oxygen starvation and heart failure;
- Intense, almost waxy, paleness of the baby's skin;
- Sharp muscle strengthening, reflex inhibition;
- Large belly due to enlarged liver and spleen;
- Extensive tissue swelling.
Anemic
The anemic form is the mildest possible. Its symptoms:
- Can be recognized in the near future (up to four to five days) after the birth of the child;
- Anemia gradually develops, the skin and mucous membranes turn pale, the abdomen enlarges;
- In general, it does not greatly affect the child’s well-being.
Jaundice
The icteric form is the most common. Its symptoms:
- The tissues acquire a pronounced yellow tint due to the hyperaccumulation of bilirubin pigment and its derivatives in the bloodstream;
- Deficiency of coloring pigment and red cells per unit volume of blood;
- Significant increase in size of the spleen and liver.
Jaundice develops soon after the baby is born, sometimes within 24 hours. It progresses over time.
The baby's skin and mucous membranes become yellow, even orange. The severity of the disease depends on how early it appears. The more bilirubin accumulates in the blood, the more lethargic and drowsiness the child develops. There is suppression of reflexes and a decrease in muscle tone.
On days 3–4, the concentration of toxic bilirubin becomes critical - more than 300 micromol per liter.
Jaundice takes on a nuclear form when the subcortical nuclei of the brain are affected. This can be understood by stiff neck and opisthotonus, the “setting sun” symptom, a high-pitched cerebral scream. By the end of the week, the skin becomes greenish, the stool becomes colorless, and the level of direct bilirubin increases.
Diagnostics
It is necessary to carry out prenatal diagnosis of the conflict between the immune system of the mother and the fetus. At risk are women with miscarriages, stillbirths, or children who died on the first day from jaundice if the mothers received a blood transfusion without taking into account the Rh factor.
- It is necessary to determine the Rh and ABO group of the child’s parents. A mother with negative and a fetus with positive Rh are at risk. The father's genotype is checked to predict the Rh factor of future children. Women with blood group I are also in a dangerous situation.
- If the woman is Rh negative, the dynamics of the titer of anti-Rh antibodies are checked at least three times during pregnancy.
- Amniotic fluid is collected at 34 weeks if there is a risk.
- An ultrasound examination is required to check for thickening of the placenta and polyhydramnios.
Postpartum diagnostics are also carried out based on clinically manifested symptoms during and immediately after childbirth, as well as laboratory indicators of the disease. A consultation with a pediatric hematologist is scheduled, who will supervise treatment if a pathology is identified.
Treatment
In severe forms of the disease, treatment is as follows:
- A blood transfusion is performed with replacement (the “bad” blood is released and the donor blood is transfused);
- Hemosorption is carried out - blood is passed through or resins capable of absorbing toxic substances;
- A certain amount of blood is taken and plasma containing toxic components is removed from it.
Exchange transfusion helps remove indirect bilirubin and harmful antibodies from the baby's blood and increase the number of red blood cells.

- Be sure to read:
To carry out such a transfusion, blood with a negative Rh and the same ABO group as that of the baby is used. Now they are trying not to transfuse whole blood, so as not to reduce the risk of transmitting HIV or hepatitis, but to use a mass of Rh-negative red blood cells or plasma, depending on the ABO group.
If the disease is mild or surgical treatment was performed, do the following:
- Glucose and protein-based drugs are infused intravenously;
- Inducers of microsomal liver enzymes are prescribed;
- Vitamins C, E, group B, cocarboxylase, which improve liver functioning and normalize metabolic processes.
If syndromic thickening of bile is observed, choleretic drugs are prescribed internally. If anemia is severe, a red blood cell transfusion is given. At the same time, phototherapy is prescribed, that is, the child’s body is irradiated with a fluorescent lamp of white or blue light. Indirect bilirubin found in the skin is oxidized, forming water-soluble components that are excreted naturally.
Complications and consequences
If the disease is severe, complications can be the most disappointing, despite treatment:
- The fetus may die during pregnancy or in the first week after birth;
- The child may become disabled, including cerebral palsy;
- May completely lose hearing or go blind;
- Psychomotor impairment may occur;
- May develop due to stagnation of bile;
- Mental disorders are often observed.
The baby's red blood cells may have different properties from those of the mother. If the placenta allows such red blood cells to pass through, they turn into foreign antigens, and the response is the production of antibodies by the mother’s body. The penetration of antibodies into the fetus can cause:
- Hemolysis (decomposition of red blood cells);
- Extremely dangerous jaundice.
Prevention
Prevention of hemolytic disease is divided into specific and nonspecific:
- For nonspecific prophylaxis, transfusion is performed taking into account the group and Rh factor and pregnancies are maintained;
- For specific prevention, anti-D immunoglobulin is administered on the first or second day immediately after childbirth (if there is a Rh conflict between mother and child) or abortion.
If the concentration of antibodies in the blood increases during pregnancy, the following is used:
- Hemosorption;
- 3-4 times intrauterine replacement blood transfusion at the 27th week using washed O(I) group O(I) Rh-negative red blood cells and subsequent delivery from the 29th week of pregnancy.

Hemolytic disease of the fetus and newborn is a dangerous disease that can and must be prevented in time, even in the early stages of pregnancy, and observed by specialists.
Often, in the first few days after birth, the baby’s skin begins to rapidly turn yellow. This phenomenon is familiar to neonatologists, who immediately prescribe an examination of the baby and appropriate treatment.
However, not all young parents know how to properly respond to such a symptom and how it is dangerous for the child. Let's consider what the diagnosis of hemolytic disease means, what are the causes of jaundice and what should parents of a newborn do?
Hemolytic disease is a serious childhood diseaseWhat is hemolytic disease and why is it dangerous?
Hemolytic disease is a rather serious condition of a newborn, in which a massive breakdown of red blood cells called hemolysis is observed in the baby’s blood. Scientists explain this phenomenon by the difference in the composition of the blood of the mother and child.
There are several varieties of this disease, but the most dangerous condition is caused by blood incompatibility according to the Rh factor. This problem occurs in almost one hundred percent of cases in women who are Rh negative. If the disease develops due to differences in the blood groups of the mother and baby (according to the AB0 system), its course is less complicated.
More often, hemolytic disease of newborns is manifested by a change in skin color - it acquires a yellow tint. However, this is only one of the symptoms of the development of the disease. The most dangerous manifestations can be determined only by the results of laboratory tests, ultrasound, Doppler sonography, and reflex disorders.
A mild form of the disease may pass without consequences, however, it also requires specialist intervention. If moderate to severe hemolytic jaundice of newborns is not treated, the baby may die. Today, there is a fully developed mechanism for the prevention and treatment of this dangerous condition, and therefore the disease scenario is favorable in most cases.
Causes of the disease in newborns
Why does pathology occur? Let's look at its main reasons. All people have a certain blood type. There are four of them - 0, A, B and AB (in domestic medicine the designations I, II, III, IV are used). The group is assigned based on the composition of the blood in which antigens are present.
In addition to antigens, in the blood of most of the Caucasian population of the planet (about 85%) there are special red blood cell proteins (D antigens) that determine the Rh factor. If this protein is not detected in the patient, his blood belongs to the Rh-negative group.
The blood composition of a newborn may differ from that of the parents (according to genetic probability). If the mother and fetus have a different group or Rh factor, prerequisites for an immunological conflict arise.
What is this contradiction? The woman's body perceives the fetal blood cells as foreign to it and begins to fight them, producing antibodies. These particles enter the baby's bloodstream, penetrating the placenta.
The described process can begin as early as the 8th week of pregnancy, when the Rh factor and blood type are formed in the fetus. However, more often mass penetration of antigens through the placenta occurs at the time of birth. As a result of this, the process of breakdown of red blood cells in the baby’s blood begins – hemolysis.

This breakdown of red blood cells causes the accumulation of bile pigment - bilirubin - in the tissues of the child’s body, which provokes damage to vital organs - the liver, spleen, and bone marrow. This component of bile is especially dangerous because it can penetrate the blood-brain barrier and disrupt brain function.
In addition, hemolysis significantly reduces the level of hemoglobin in the blood, and the baby becomes anemic. Anemia is a rather dangerous condition for a newborn, as it contributes to oxygen starvation of tissues and organs.
Blood mismatch according to the ABO system (that is, group) usually does not lead to serious consequences. However, if during pregnancy a woman suffered from ARVI, influenza or other infectious diseases, this increases the permeability of the placenta, which leads to the development of dangerous forms of the disease.
According to statistics, the disease more often occurs in babies whose Rh factor does not match the maternal blood. However, some experts are confident that an immunological conflict in the ABO system is not a rare phenomenon, but its symptoms can be blurred and a diagnosis is often not made.
Classification and symptoms of hemolytic disease of newborns
As we mentioned, hemolytic disease has several varieties. More precisely, there are four of them.
 Jaundice form of hemolytic disease
Jaundice form of hemolytic disease Let's take a closer look at these types:
- The icteric form of hemolytic disease occurs especially often in newborns. This is a moderately severe type of disease. It is characterized by the appearance of initial symptoms only on the next day after birth. The child is born with normal skin color and without visible pathologies. Then the baby’s skin acquires a yellowish tint, which gradually becomes brighter. The child's reflexes may be depressed, the liver and spleen may become enlarged.
- Kernicterus or bilirubin encephalopathy is a dangerous intoxication of the brain. The disease occurs with delayed treatment of the icteric type of disease. Kernicterus occurs in two stages. The initial phase is characterized by a relaxed baby’s posture and weak reactions to stimuli. The skin becomes bluish, convulsions occur, and the baby’s eyes are wide open (we recommend reading:). The next stage is spastic. The child screams, his muscles are tense, his breathing is labored. This disease can lead to cerebral palsy, deafness, and speech disorders.
- The anemic form is the most harmless. In this condition, the child has reduced hemoglobin in the blood, the baby is lethargic, weakened, and does not breastfeed well. This type of disease occurs in every 10 sick newborns and has a favorable scenario.
- The edematous variety is the most dangerous case of the disease. A child is born with characteristic edema in all cavities of the body - the heart sac, pleural region, and abdominal cavity. The skin has a yellow tint and pallor. The liver and spleen are enlarged, a blood test shows profound anemia (we recommend reading:). Such symptoms can cause the development of heart failure and lead to death while still in the womb or immediately after birth.
All types of the disease have similar symptoms - yellowing of the skin, dark urine, lethargy of the child. However, the most accurate diagnosis can be made only on the basis of laboratory tests.
Diagnostic methods
Diagnosis of the disease is carried out at the stage of intrauterine development of the fetus and after birth. Let's consider methods of natal and postnatal diagnostics.
If the mother’s blood is Rh negative, even during pregnancy the doctor collects data to create a picture of possible pathologies. A lot of information is taken into account: incompatibility of the parents’ blood, abortions, miscarriages, previous births of the mother.
At least three times during pregnancy, a woman has a titer of anti-Rhesus antibodies. Alarming symptoms - abrupt values, their stable increase, as well as a decrease in the level shortly before birth - may indicate the penetration of antibodies through the placenta.
If there is a risk of an immune conflict, the doctor prescribes a test of the amniotic fluid (bilirubin, levels of protein, iron, glucose, etc. are determined). The results of ultrasound and Doppler sonography are certainly taken into account - thickening of the placenta, polyhydramnios, blood flow velocity in the cerebral artery, etc.
 If a pregnant woman’s blood is Rh negative, doctors will most likely insist on analyzing the amniotic fluid.
If a pregnant woman’s blood is Rh negative, doctors will most likely insist on analyzing the amniotic fluid. Postnatal diagnosis is made on the basis of examination of the baby after birth. These are the presence of jaundice, control of bilirubin over time, erythroblastosis, hemoglobin level in the blood, etc. All indications are considered in complex. An immunological conflict in the ABO system, despite a favorable prognosis, also requires the attention of a doctor.
Differential diagnosis is carried out with such conditions as hereditary hemolytic jaundice, sepsis, hemorrhages, which can cause anemia. Cytamegalovirus infections and toxoplasmosis are also eliminated.
Jaundice in newborns can be purely physiological in nature. Its occurrence is due to insufficient maturity of liver enzymes and replacement of hemoglobin cells. As soon as enzymes begin to be produced in the required quantities, the baby’s skin color acquires a normal shade. The described condition does not require treatment.
 Hemolytic disease requires blood transfusion, hemosorption or plasmapheresis
Hemolytic disease requires blood transfusion, hemosorption or plasmapheresis In difficult cases, a blood transfusion is indicated, which is given to the fetus in utero or after birth. Other ways to eliminate symptoms are hemosorption (passing blood through special filters) and plasmapheresis (removing plasma containing toxins from a limited volume of blood). However, replacement blood transfusions and other interventions have clear indications:
- if indirect bilirubin in the umbilical cord blood exceeds 60 µmol/l or increases at a rate of more than 10 similar units per hour;
- the baby’s hemoglobin level is critical – less than 100 g/l;
- jaundice appeared immediately after birth or in the first 12 hours.
It should be remembered that blood transfusions often carry complications, most of which are associated with violations of the procedure technique. Only fresh blood, stored for no more than 2 days, and a low transfusion rate are used. In addition, it is important that the red blood cell mass is close to body temperature to avoid cardiac arrest.
Also, glucocorticoids are administered to newborns who are in serious condition. This therapy is possible within a week after birth.
For babies with milder symptoms, conservative treatment is indicated. Typically this is:
- intravenous administration of glucose, protein;
- use of liver enzyme activators;
- the appointment of absorbents that help bind and remove toxins from the body;
- the use of vitamins and medications that stimulate liver function and accelerate metabolic processes in the baby’s body.
All children with signs of yellowing of the skin are prescribed phototherapy. This procedure involves exposing the skin to tiny pieces of fluorescent light (white or blue). Such measures remove indirect bilirubin from the body, transforming it into water-soluble substances.
Phototherapy is also carried out to prevent the occurrence of hyperbilirubinemia, if fetal hypoxia has occurred, and thermoregulation disorders. The procedure is often prescribed for premature babies.
You can start lactation with hemolytic disease only after the permission of your doctor. As a rule, breastfeeding occurs only three weeks after birth. During this period, antibodies are completely removed from the mother's milk, but for now the baby is fed formula or donor milk.
 If you have HDN, you may not be able to put your baby to the breast right away; as a rule, lactation can begin 3-4 weeks after birth
If you have HDN, you may not be able to put your baby to the breast right away; as a rule, lactation can begin 3-4 weeks after birth Vaccinations, which are usually done in the maternity hospital, can be postponed in case of jaundice. In particular, BCG is done a little later.
Consequences of hemolytic disease for a child
The consequences of hemolytic disease of newborns may be absent at all, or they may be quite significant. It all depends on the form of the disease, as well as the timeliness and adequacy of therapy. If a mild form of hemolytic disease is diagnosed, by the end of the second week all the child’s health indicators return to normal. Subsequently, the baby will grow well and develop according to his age.
If the bilirubin level exceeds the critical value of 340 µmol/l, negative consequences are possible in the future. Short-term ones include the development of the nuclear form of the disease, when the baby’s brain suffers from toxins. This form can lead to various mental disorders, the development of cerebral palsy, and hearing loss.
The development of the nuclear form can be judged by muscle rigidity at the back of the head, protrusion of the fontanelle, muscle twitching, and signs of suffocation. There are also other symptoms of this condition that neonatologists are aware of.
 Babies who have suffered a severe form of HDN are registered with a neurologist, ophthalmologist and pediatrician
Babies who have suffered a severe form of HDN are registered with a neurologist, ophthalmologist and pediatrician High levels of bilirubin can affect later. According to statistics, every third child with similar symptoms is diagnosed with neuropsychic disorders. In this regard, children with a severe form of hemolytic disease, after stabilization of their condition, are registered with a neurologist, ophthalmologist and pediatrician.
Some of the children require a long period of rehabilitation, while others only need a couple of months for final recovery. However, observation by specialists is indicated for both.
Preventive actions
Preventive measures include special monitoring of the condition of a pregnant woman who is at risk.
Patients with a negative Rh factor are subject to separate registration in the antenatal clinic.
The following activities are carried out:
- Anamnesis collection - previous pregnancy blood transfusions, miscarriages, stillborn children, abortions. This information will help estimate the likely level of antigens in the patient's blood. The most vulnerable of them are those who have already given birth or with a history of abortion, since in these cases the body is already ready to “fight back” and the likelihood of an immune conflict is high.
- In critical cases, the doctor recommends an injection of anti-Rhesus immunoglobulin to suppress the production of antibodies. Such an injection will prevent problems with a new pregnancy.
- Systematic monitoring of a pregnant woman’s blood for the presence of Rh antibodies. If their concentration increases, the patient is referred for preventive treatment.
- Often, the doctor prescribes stimulation of labor after 36 weeks of pregnancy. Premature birth is caused due to the high risk of hemolytic disease of the newborn, since it is in the last month of gestation that the permeability of the placenta increases and the exchange of blood cells between mother and child is activated.
Hemolytic disease in newborns (HDN) is a pathology that occurs during fetal development or during the first hours after birth. The cause of this pathology is incompatibility between the blood of the fetus and its mother, when the woman begins to produce antibodies to the child’s red blood cells (immunological conflict). The development of the disease occurs due to the fact that antibodies from the female body enter the child’s body. In this way, active destruction of the baby’s red blood cells occurs... in addition, HDN is almost the first on the list of reasons that cause kernicterus in babies and anemia.
It is worth noting that in recent years, cases of hemolytic disease have increased significantly - approximately one case per 250-300 births. As a rule, this pathology occurs due to Rh conflict between a woman and a child. If we talk about blood group incompatibility, then there are several times fewer such cases. Incompatibility with other erythrocyte antigens is generally considered rare, because such cases are isolated.
If hemolytic disease develops according to the Rh factor, then in 3-6% of cases it proceeds quite mildly, but at the same time it is very difficult to diagnose. There are cases when a hemolytic disease of this type was discovered in a newborn already in an advanced stage, when treatment does not bring a noticeable result.
When a newborn begins to develop hemolysis or destruction of red blood cells, the level of bilirubin in his blood very quickly increases and provokes the development of anemia. When the level of bilirubin is too high and exceeds a critical level, it begins to release toxins that affect the brain and many other organs of the child. In addition, anemia begins to progress very quickly and the body begins to do everything possible to compensate for the lack of oxygen. Thus, the liver begins to increase in size, followed by the spleen.
Clinical forms of hemolytic anemia in a newborn baby
Today, doctors distinguish the following clinical forms of hemolytic anemia:- Edematous form of HDN. This form is the most severe and begins to develop in utero. As a result of the destruction of red blood cells, the child develops a severe form of anemia, metabolism is disrupted, tissues swell and protein levels decrease. If HDN begins to develop early in pregnancy, then it can end in miscarriage. If the child still survives, he will be born very pale, with pronounced swelling.
- Jaundice form of HDN. This form can be found most often. The main symptoms are the early development of jaundice, anemia and a significant enlargement of the liver and spleen. Jaundice may appear immediately after birth or after about 1-2 days, which is not typical for physiological jaundice. The earlier it appears, the more severe HDN will be. Signs of the disease include greenish skin color, dark urine and colorless feces.
- Anemic form of HDN. This form is the most gentle and easiest. It appears within seven days after the birth of the child. It is not always possible to immediately notice the appearance of pale skin, and therefore HDN can be diagnosed at 2-3 weeks of the baby’s life. Externally, the child remains the same, but the liver and spleen begin to increase in size. Bilirubin levels will be elevated, but only slightly. This form of the disease can be easily cured without harmful consequences for the baby’s health.
Diagnosis and treatment of hemolytic disease of newborns
Today, medicine is more developed and it is possible to diagnose the presence of hemolytic disease in advance, as well as begin to treat it on time. After all, timely detection and treatment is the key to a child’s quick recovery. It is worth noting that today there are two types of diagnosis of tension-type headache: antenatal and postnatal diagnosis.Antenatal diagnosis is carried out during pregnancy in women who are at risk. If a woman is Rh negative, she must be tested three times for the presence of antibodies in her blood during pregnancy. It is very important to take into account the results over time, because they can show a high risk of a child’s disease. In order to finally make sure of the diagnosis, you need to examine the amniotic fluid for the presence of levels of bilirubin, iron, glucose and protein. In addition, changes in fetal development, which can be detected by ultrasound, may cause suspicion.
Postnatal diagnosis is carried out after the birth of the child and consists entirely of studying the clinical symptoms of the disease in the child. In this case, it is necessary to study absolutely all the data, both in complex and in dynamics.
How to treat hemolytic disease in a newborn baby
If a severe form of hemolytic disease is detected in a child, then doctors resort to extreme treatment measures: replacement blood transfusion, hemosorption, or plasmaphoresis. Thanks to blood transfusion, excess bilirubin can be removed from the body, as well as red blood cells and hemoglobin can be replenished. Today, doctors have stopped transfusing whole blood, and for transfusion they use red blood cells and fresh frozen plasma.Indications for blood transfusion if the baby is premature
- The level of indirect bilirubin exceeds the critical value;
- bilirubin level increases every hour by approximately 6-10 µmol/l;
- a severe form of anemia is observed.
In addition, vitamins B2, B6, C, activated carbon, prednisone, cocarboxylase or phenobarbital can be used to treat hemolytic disease. It is worth noting that previously it was believed that if a child had a more hemolytic disease, then he should not be put to the breast. Today it has been proven that the antibodies that are in a woman’s milk do not enter the baby’s blood and are completely destroyed under the influence of hydrochloric acid in the baby’s stomach. Therefore, there is no need to be afraid of anything and put your baby to your breast as often as possible. This will help him get stronger faster and begin to fight the disease on his own.
Prevention of hemolytic disease in a newborn baby
First of all, those women who have Rh negative need to worry about prevention. As a preventive measure, anti-rhesus administration is used during the first days after the birth of a healthy child or after abortions and miscarriages. This blocks the production of antibodies by the mother's body. It is also worth remembering such specific prevention as preventing abortions or blood transfusion of only blood of one group and rhesus.Human blood is the same tissue as bone or cartilage, only in the form of a suspension. Like other tissues, it is protected from the entry of other blood that has a different structure. Antibodies are dissolved in the liquid part of this tissue, whose task is to attack foreign red blood cells that enter here if the proteins on them differ from those on one’s own cells. Such an “attack” on the body that served as the source of “wrong red blood cells” is called hemolytic disease.
When a pregnant woman's blood antibodies destroy the red blood cells of the baby developing in the uterus, this is a hemolytic disease of the fetus. If such a reaction begins in the body of a newly born baby (antibodies were acquired during childbirth), it is called hemolytic disease of the newborn. Both diseases develop according to a similar mechanism and are life-threatening for children. They occur in a mother with Rh negative, when the child is Rh positive, or if the maternal blood type is 1, and the fetus has formed 2 or 3.
What are blood groups
The body carefully protects blood from other blood that is not similar to its own. He placed some proteins (antigens) on red blood cells, and others in the blood plasma (they are called antibodies). If red blood cells against which there are antibodies in the plasma enter the main blood mass (in this case, the maternal blood mass), then such red blood cells are destroyed.
So, if we consider blood groups according to the system familiar to us, in which there are 4 groups, red blood cells can have either antigen A, or antigen B, or both antigens at once (AB), or none of them. At the same time, antibodies “float” in the plasma that cannot attack their own antigens: anti-A (called alpha) or anti-B (called beta).
For example:
- If a person has group 2, his red blood cells show antigen A, and the β antibody “floats” in the plasma.
- In group 3, red cells show protein B, and in the plasma - antibody ɑ.
- Group 4: there are 2 antigens located on red blood cells (A and B), but there are no antigens in plasma.
- Group 1 - red blood cells do not carry antigens, but in the plasma there are 2 antibodies at once - both ɑ and β. It is group I, when the mother has it, that can become a source of damage to the fetus if it has developed blood group II or III (the formation of group IV in a child from a mother with group I is impossible).
The Rh factor is also a kind of blood group. This is a protein that is located on the inner membrane of red blood cells and, unlike proteins A and B discussed above, are located only on red blood cells (proteins A and B are also found on all fetal tissues, the lining of the placenta, and in amniotic fluid). When the Rh factor (Rh factor) is present on the erythrocyte membranes, the blood will be Rh-positive; if it is not there, it will be Rh-negative.
There are no antibodies against Rhesus (as in the case of the ABO group) in the plasma. Only if a person lacking the Rh factor is given a transfusion of red blood cells containing such a protein, antibodies will be produced in the blood against them. And the next time Rh-positive erythrocytes are introduced, these antibodies begin to attack them. Consequently, in a Rh-negative woman, when her child has developed Rh-positive, hemolytic disease in the first pregnancy is practically impossible (more on this below).
There are other blood types, but they have a weaker ability to induce the formation of antibodies.
The process of destruction of red blood cells is called hemolysis, from which the name of the disorder in question comes - hemolytic disease of the fetus and newborn. With the destruction of red blood cells, the amount of hemoglobin that carries oxygen decreases. Hemoglobin, when released into the plasma, is converted into bilirubin.
How a fetus's blood type is formed
Both groups - according to the AB0 system (A, B, zero) and according to the Rh factor - are formed at 5-6 weeks of fetal life. They are encoded in a specific pair of chromosomes, and such a region is present on both one and the other chromosome. They may have the same form of the same gene (homozygosity), or it may happen that on one chromosome this gene is dominant (it dictates its trait), on the other it is recessive.
Rh factor is inherited from father and mother, and is encoded by 6 antigens. These are genes D, C and E. The main one among them is gene D: it is present in 85% of people (gene C in 70%, gene E in 30%) and “dictates” whether the blood will be Rh+ or Rh-. If there is DD in both chromosomes, this is Rh-positive blood, if Dd is also, but the combination of two recessive genes (dd) codes for Rh-negativity.
If the mother has a dd genome and the father has DD genes, then the chance that the child will have Rh- is 0% (all 100% will carry Dd), but if the father has Rh+ (Dd), then the chance of having an Rh-negative child is – 50%.
The blood group according to the ABO system also has this feature, only here the genes encoding proteins A and B are considered dominant, and the gene encoding the absence of protein (0, zero) is recessive. If the mother is with group 1, then she can be written as 00, and if the child’s father has group 2, then he can be either AA or A0. That is, the probability that the baby will inherit group 2 in the first case (when the father is AA) is 100%, and in the second – 50%. The same is with the third group, only instead of antigen A there will be antigen B. And in these cases, if the fetus develops a blood type that differs from the mother, there is a probability (but only 10%) that the mother’s body will “bomb” red blood cells and fetal tissue.

AB0 blood group inheritance table
Now about why the fourth blood group does not cause incompatibility in a mother with group 1: such a group cannot be formed in a child of parents where the mother has a set of 00. In this case, a child with a father with group 4 or with group 2 (A0) may appear. or with group 3 (B0). If the father has group 2, then the child will be either group 1 or 2. If the father has group 3, then the fetus’ group is formed as 1 or 3.
Causes of the disease
Depending on which antibodies damaged the red blood cells, the causes of hemolytic disease of the fetus are:
- in 85-90% of cases – incompatibility according to the Rh factor;
- 10% of diseases are a mismatch in the “usual” (1 to 4) blood group;
- in 1% of situations – incompatibility with other, rare blood groups;
- in a small percentage of cases there is a mismatch for several antigens.
For hemolytic disease to develop, at least 0.5 ml of fetal blood must enter the mother's blood. Since this happens mainly during childbirth, especially during pregnancy, the likelihood of developing the disease during the first pregnancy is low. Even if the first pregnancy occurs with damage to the placenta, due to which the blood of her child begins to reach the mother even before birth, the chance of hemolytic disease occurring is still small.

The most common cause of the disease is Rh factor incompatibility
Initially, only antibodies appear in the mother’s body that are large in size and do not pass through the placenta. Immunoglobulins of the size that will allow them to reach the fetus are formed only after 3-5 months.
Thus, the risk of hemolytic disease is high in the second and subsequent pregnancies (in the first pregnancy - 9-10%, in the second, if the first birth was 42-47%, and if the first pregnancy ended in miscarriage or abortion - 96%). The following dependence is also observed: the less time has passed between pregnancies, the higher the chance of developing hemolysis.
The above is especially true: a mismatch in blood type can also occur during the first pregnancy, since a woman in everyday life encounters A- and B-antigens early (for example, when administering vaccinations).
Although there are only 15% of Rh-negative people, incompatibility for the Rh factor is observed more often than for the group: in 13% versus 10% of cases, respectively. This is due to the fact that the rhesus protein is water-insoluble, and it is not neutralized by either the amniotic fluid system or blood plasma proteins.
Hemolytic disease due to a mismatch of Rh factors of the mother and fetus will occur more quickly (even during the first pregnancy) if at least one such factor occurs:
- have already had medical abortions or spontaneous miscarriages;
- was accidentally transfused with Rh-positive blood or blood in which the Rh on red blood cells is so weak that it is determined by all laboratories as negative;
- organ transplants were performed;
- was ;
- children have already been born with signs of hemolytic disease of the fetus;
- invasive diagnostics were carried out during pregnancy: blood sampling from the umbilical cord or chorionic villi;
- a hematoma has formed behind the placenta;
- there was bleeding due to low or central placenta previa;
- , threat of premature birth.
However, only 4 out of 100 Rh-negative women develop hemolytic disease. The reasons for this: protection of the placenta (if it is not infected and gestosis has not developed, then the placenta allows no more than 0.1-0.2 ml of fetal blood to pass through), suppression of the woman’s immune system, which is normal during pregnancy.
The risk is also reduced in women who were born from Rh-positive mothers with the Dd genotype and in those whose blood is of the first group. In the latter case, the fetal red blood cells have a high chance of not reaching the mother’s blood, but being destroyed by alpha and beta antibodies.
In 20-35% of people, the immune system will not respond to the D-antigen at all.
Forms of the disease
Based on the main manifestations, there are 4 forms of hemolytic disease of the fetus:
- Intrauterine death with tissue changes (delamination), characteristic of prolonged exposure to water (this is called maceration). In this case, the child dies without being born, but he has no edema or jaundice.
- Anemic form. The main problem is a lack of oxygen due to the fact that the fetal red blood cells are disintegrating, attacked by maternal antibodies.
- The icteric form, when the main symptoms arise due to the massive breakdown of hemoglobin in red blood cells, when a large amount of bilirubin is released into the blood and tissues. It stains tissue yellow and is also very toxic to the fetal or infant brain.
- Edema form. In this case, the level of protein in the blood decreases. Fluids in the blood, which were retained in the vessels only due to the attraction of proteins, have to leave the vessels and permeate the tissues, causing swelling. The latter can have varying severity: from appearing only in the skin to sweating fluid in the body cavity: in the stomach, between the layers of the pleura (“film” that wraps the lungs), between the heart and pericardium, between the membranes of the brain.
How does hemolytic disease manifest?

Jaundice form of the disease in a newborn
The disease is registered in 3-6% of newborns. It develops in 3.5% of pregnancies that occur after spontaneous miscarriage and in 5.5% after abortion.
Symptoms of fetal hemolytic disease may not be observed from the first week, but only when blood group proteins appear on the fetus’s red blood cells and tissues, that is, from 5-6 gestational weeks. The pregnant woman herself practically does not feel a conflict regarding the group or Rh factor. In some cases, symptoms similar to gestosis develop: swelling of the feet or an increase in interstitial fluid also in the legs, thighs, abdomen (in severe cases, the arms and face swell; fluid may also appear in the body cavities), increased pressure, decreased amount of urine.
The main signs of the disease can be seen using a test such as an ultrasound. With the edematous variant, ultrasound shows that the fetus has a large mass (up to its increase by 2 times), its liver, spleen, and heart are enlarged. An ultrasound doctor can also see fluid leaking into the pleural, abdominal cavities, and also into the pericardium.
Intrauterine fetal death is diagnosed from the 20th to the 30th week of gestation, so at this time the pregnant woman should pay special attention to its movements and her own well-being. Deterioration of the condition, the appearance of nausea, vomiting, and an increase in temperature may indicate the death of the fetus and the entry of particles of its decaying tissue into the mother’s bloodstream.
The icteric and anemic forms are detected only after childbirth. In the first case, the baby is often born with normal skin color, but after a few hours his skin and sclera turn yellow. If the bilirubin released during the breakdown of red blood cells affects the central nervous system, especially the brain, the newborn sleeps all the time, his limbs hang sluggishly and are not in good shape. The baby sucks sluggishly, often spits up, and may develop seizures. If the bilirubin level is high, and the child often vomits and is very lethargic, then he may die on the 5-7th day of life.
In the case of the anemic variant of the disease, the newborn’s skin is pale, breathing is rapid, he sucks well, but gets tired quickly.
The more severe the severity of the disease, the greater the degree of prematurity of the baby. A more severe course is typical for Rh conflict, and for the reaction between maternal group 1 and group 3 in the fetus.
How is the disease diagnosed?
As soon as a woman registers with the antenatal clinic, she is prescribed various examinations, and, in particular, determination of her blood type. In addition, her medical history is ascertained: blood transfusions, birth of children with hemolytic disease, and, if possible, the group and Rh of the child’s father are determined.
Next, the direct diagnosis of hemolytic disease of the fetus begins: the mother donates blood monthly to determine antibodies to Rhesus or group antigens, if the titer (it is written as a fraction, for example, 1:16 and so on) increases (that is, the second digit increases) quickly, similar tests should give up more often. Ultrasound diagnostics are mandatory (they look at the development of the fetus, the condition of its internal organs, placenta, amniotic fluid) and, with the help of which the condition of the vessels between the uterus and placenta is determined.
If necessary, under ultrasound control, the umbilical cord vessel is punctured, and the blood type of the fetus, antibodies to erythrocyte proteins, hemoglobin, bilirubin, and the state of blood cells are determined. From the 23rd week, CTG is performed at a determined individual frequency, listening to the fetal heartbeat.
As soon as a child with hemolytic disease is born, blood is immediately taken from a vein to determine the level of bilirubin, hemoglobin and other indicators.
Therapy

If the antibody titer increases, or ultrasound detects a change in the size of the internal organs of the fetus, it is necessary to treat hemolytic disease. Before this, the woman is prescribed sorbents, vitamin E, and hemostatic drugs.
If minor disorders are diagnosed in utero, treatment may be started after birth. The newborn is given replacement blood transfusions (blood of group 1 with the same Rh as the child’s is needed), phototherapy, and solutions of glucose, vitamin C and E are administered.
Consequences and prevention
The consequences of hemolytic disease in most cases are dangerous to the life and health of the child. Although effective methods of early diagnosis and treatment are now used, mortality from this disease occurs in every 40 fetuses or newborn children. If a patient with the icteric form survives, he may have significant delay in psychomotor development, seizures, and even more profound disorders.
Only the anemic variant of the disease is favorable: in this case, self-healing can be observed. In this case, the child may experience frequent colds, allergies, and complications after vaccination.
Prevention
Prevention of hemolytic disease consists of injections of anti-Rhesus immunoglobulin to women after abortion, childbirth with an Rh+ fetus, manipulation of the uterus, or ectopic pregnancy. Blood transfusions and abortions for Rh-negative patients should be performed only according to strict indications.
Hemolytic disease (HD) of the fetus and newborn is a pathological condition that occurs as a result of incompatibility of the blood of the mother and fetus for certain antigens, in which hemolysis of fetal red blood cells occurs under the influence of isoantibodies mothers penetrating the placental barrier.
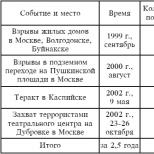
Most often the disease develops as a result Rhesus conflict or conflict according to the ABO system(1 case in 250-300 births). The share of HD in the structure of perinatal mortality is 3.5%.
Types of Rh factor and Hr antigen
There are three main types of R h - factors: antigens D (Rh),
C (Rhj) and E (Rhn) and
three different types of antigen Hr: d, s, e.
Factor D has the most pronounced antigenic properties.
Of the Ng factors, factor c has a greater ability to cause formation.
ETHIOLOGY AND PATHOGENESIS
Conflict due to isoserological
incompatibility between mother and fetus most often develops due to erythrocyte antigens Rh-Hr and AB0.
Depending on ethnicity, frequency of Rh negative blood affiliation in the population varies from less than 1% in the Chinese, to 30% or more in the Basques. In Europeans, the average frequency is 15%.
Isoimmunization can result from two main reasons: - the first, fortunately, is becoming less and less common - iatrogenic. She
associated with the introduction into a woman’s body Rh positive blood when she received blood transfusions in the past or when autohemotherapy;
- the second is the main one - this is the fetal-maternal transplacental transfer of the fetus into the mother’s bloodstream during pregnancy and childbirth.
Rh isoimmunization- this is the immune response of the mother’s body to the ingress of foreign substances located on the fetal membrane. The sizes and shapes of the fetus and adult are different, therefore, by quantifying red blood cells in the maternal circulation
the fetus can indirectly judge the volume of fetal-maternal transplacental bleeding. Their frequency and volume increase significantly as pregnancy progresses. If during the first trimester of pregnancy they
are registered only in 3% of pregnant women (their volume is about 0.03 ml), then in the third trimester they are detected in 45% of pregnant women and the estimated volume of transplacental bleeding reaches 25 ml.
The primary immune response after the D-antigen enters the mother's bloodstream appears after a certain time - from 6 weeks to 12 months.
It consists in the appearance of class M, whose molecules are large and do not penetrate the placental barrier to the fetus. This explains the absence of hemolytic disease in the fetuses of most primigravidas
Rh negative women.
The entry of D-antigen into the mother's bloodstream during repeated pregnancy causes a rapid secondary immune response in the form of the formation of small size class G, which, freely penetrating the placental barrier, are deposited on the membrane of the erythrocytes of the Rh-positive fetus, leading to their hemolysis.
Rh antigens are found on the fetal red blood cell membrane by the 30th day of pregnancy. Anti-B antibodies (G) circulating during repeated pregnancy penetrate the placental barrier and bind to
corresponding antigens on the membrane of erythrocytes, which causes accelerated destruction of the latter in the organs of the reticuloendothelial system.
Massive destruction of red blood cells leads to the development of anemia in the fetus (anemic form), the appearance of which causes an increase in the concentration of erythropoietin in the bloodstream of the fetus. Erythropoietin, in turn, stimulates hematopoiesis, as a result of which foci of extramedullary hematopoiesis appear, mainly in the liver and spleen of the fetus, which increase significantly.
Extramedullary hematopoiesis is characterized by incomplete development of red blood cells and the appearance in the circulation erythroblasts.
Although indirect (unbound) bilirubin, formed during hemolysis of fetal red blood cells, is intensively excreted through the placenta, an increase in its concentration disrupts protein synthesis in the fetal liver, which has already been altered due to the appearance of extramedullary hematopoiesis. The consequence of this pathological process is
hypoproteinemia, decreased oncotic pressure of fetal blood plasma and portal. The development of anemia in the fetus leads to a decrease in the oxygen capacity of its blood. This, in turn, entails increased anaerobic glycolysis in tissues, acidosis, decreased blood buffer reserves, damage to the capillary endothelium and the development of chronic hypoxia.
Against the background of chronic hypoxia and acidosis, a compensatory increase in cardiac output and cardiac output occurs, leading to myocardial hypertrophy and the gradual development of heart failure, and as a consequence, to an increase in central venous pressure ( CVP).
Promotion CVP complicates the flow of lymph through the main lymphatic vessels, causing disruption of the outflow of interstitial fluid and an increase in its oncotic pressure. The whole complex of ongoing pathological processes causes the accumulation of fluid in the tissues and serous cavities of the fetus, which is clinically manifested by the development of generalized edema. (edematous form of GB) and in the absence of appropriate treatment leads to intrauterine fetal death.
Understanding the pathophysiology of the development of hemolytic disease of the fetus has made it possible to develop methods for preventing isoimmunization of Rh-negative pregnant women, methods for diagnosing and treating hemolytic disease of the fetus and newborn.
All pregnant women, at their first visit to the doctor, should have their blood type and R h factor tested, as well as a determination n t i r e s u n s . If Rh-negative blood is detected in a pregnant woman who has an Rh-positive factor in her husband, repeated determination of anti-Rhesus drugs is indicated every 4 weeks until
childbirth It should be remembered that Rh-positive individuals can be homozygous or heterozygous, while Rh-negative individuals can only be homozygous. This has practical implications because the offspring of a homozygous Rh positive father and Rh negative mother will be Rh positive 100% of the time. If the father is heterozygous, the fetus has only a 50% chance of being Rh positive.
The history of an Rh-isoimmunized pregnant woman is of great importance in assessing the risk of developing severe forms of hemolytic disease.
The antibody titer in the blood of a pregnant woman and its dynamics can be used to assess the severity of hemolytic disease. At the same time, the boundary after which development is possible clinically significant forms of hemolytic disease of the fetus is titer 1: 8.
In subsequent pregnancies the value
The titer of Rh antibodies in the mother's blood does not correlate with the severity of hemolytic disease of the fetus and, in addition, edema in the fetus can develop with a minimum antibody titer of 1:2.
Ultrasound scan for diagnosing hemolytic disease
The experience of using ultrasound scanning for diagnosing and determining the severity of hemolytic disease of the fetus shows its high sensitivity and specificity in the development of only heavy -
edematous form of the disease, as evidenced by the determination of free fluid in its serous cavities. For other forms of hemolytic disease
The sensitivity and specificity of a single fetal ultrasound examination are low. However, the value of ultrasound examination can be increased by dynamic monitoring of the fetal condition by the same investigator. At the same time, attention is paid to the size of the liver, spleen, thickness of the placenta and echogenicity of the intestine, which is of particular importance for identifying the very initial stages of the development of edema in the fetus and its resolution against the background
intrauterine treatment.
In addition, an indirect indicator of the presence of anemia
in a fetus that does not have edema, an increase in blood flow velocity in the middle cerebral artery and aorta, determined by Doppler metry and using color Doppler mapping, may serve as an indication. Changes in blood circulation speed are associated with the formation of a hyperdynamic type of circulation
in the fetus, which forms against the background of developing anemia, as well as due to an increase in cardiac output against the background of an increase in venous return, which is a consequence of a decrease in blood viscosity.
This criterion, assessed at
dynamics, can be used as an additional marker to determine the optimal timing of the start of infusions and their repetitions in the anemic form of hemolytic disease.
Tactics of pregnancy management during Rh-isoimmunization of a pregnant woman
The management tactics for a woman depend on the Rh status of the fetus.
It is possible to determine the Rh genotype of the fetus using molecular genetic methods using any cells of fetal origin, which provides a unique opportunity to determine the management tactics of Rh-immunized women already at the beginning of pregnancy.
Polymerase chain reaction() has 100% sensitivity and specificity in determining the Rh genotype of the fetus.
Amniocentesis is the safest invasive intervention for the fetus between the 14th and 18th weeks of pregnancy, as this is the best time for Rh typing of fetuses in Rh-immunized pregnant women.
Obviously, in the near future, the improvement of methods for isolating fetal blood cells in the peripheral blood of the mother (and fetal blood cells are always present in the maternal bloodstream due to fetal-uterine transfusions) will gradually replace invasive interventions during pregnancy to determine the Rh genotype of the fetus from clinical practice.
Currently, assessment of the severity of fetal hemolytic disease is based on invasive interventions.
Since 1961, analysis of the optical density of amniotic fluid,
obtained by amniocentesis was the main method for diagnosing the severity of hemolytic disease. However, this method has obvious disadvantages. We are talking, first of all, about a very high frequency of false positive and
false negative results, especially in the second trimester of pregnancy, and
the need for repeated, 2-4-fold amniocentesis operations. All this to the ambassador
led to the search for methods for obtaining fetal blood and its direct study
dovaniya.
Development in 1983 of a method for obtaining fetal blood using cor-
assistant professor - puncture of umbilical cord vessels under ultrasound control -
opened a new page in the diagnosis and treatment of hemolytic disease
fetus This method can be used already at the end of the first half
pregnancy, which is of fundamental importance when it is necessary to diagnose
tics of early development of severe forms of hemolytic disease of the fetus
Analysis of hematological parameters in fetuses with uncomplicated course
pregnancy made it possible to determine the boundaries of normal distribution
the rank of all blood parameters depending on the stage of pregnancy. All major
indicators that allow assessing the degree of anemia in the fetus, such as
hemoglobin and hematocrit, as well as the content of red blood cells, increase according to
as pregnancy progresses. Moreover, at the beginning of the second half
physiologically proceeding pregnancy, the hemoglobin level is
120 g/l and increases by the 37th week to 140 g/l. Average hematocrit level
blood increases from 36 to 43%.
Classification of the severity of fetal hemolytic disease depends on
values of hematocrit and hemoglobin of his blood obtained during cordocentesis.
Assessing the severity allows you to determine the tactics for managing isoimmunity.
tioned pregnancy, justify the need for intrauterine treatment
and optimal time for early delivery.
The content of total protein and albumin in fetal blood plasma increases as
gestational age increases in uncomplicated pregnancies.
Albumin concentration increases by almost one and a half from the 20th to the 37th week
times, reaching 35 g/l by the end of pregnancy. During development in fetuses
severe anemia, especially with the formation of edema, albumin content in
fetal blood is reduced, which made it possible to develop a new pathogenetic
method of treating severe forms of hemolytic disease of the fetus using
albumin drug.
The edematous form of hemolytic disease can develop within
II trimester of pregnancy, and, in this case, almost 100% of such fetuses
die antenatally before the 30th week of pregnancy. However, even with
edematous form of the fetus, red blood counts can be successfully corrected
rovana. However, when transfusing only washed red blood cells until
nora, despite the complete normalization of blood counts in the fetus, swelling is
occurs after the first transfusion in only 33% of fetuses. Therefore, at present
a method of combined transfusion of washed red blood cells into the fetus was developed
donor and 20% albumin solution in a ratio of 5: 1. This therapy leads
to the disappearance of pronounced edema in all fetuses. In this case, the norm occurs
lization of both red blood parameters and serum al
boomina.
Since until now etiopathogenetic methods of treating hemo
There is no lytic disease of the fetus in the initial stage of development (no
convincing data on the positive effect on the course of the disease in patients
and any medications or procedures), then today you can
to believe that the main method of treating severe forms of hemolytic disease
the fetus is to carry out intrauterine transfusions of washed erythro
donor cytoplasm in combination with albumin under ultrasound guidance.
For example, in the absence of edema in the fetus after transfusion, sex
normalization of his blood parameters, in particular, hematocrit increases
on average 1.9 times. Even with severe hemolytic anemia against the background
developed edema in the fetus, this method allows for complete correction
tion of anemia with an increase in hematocrit values by 3 times.
In the treatment of early developed severe forms of hemolytic disease
nor is repeated intravascular transfusion required for the fetus. AT NIIAG
them. D. O. Otta RAMS has his own experience of 5-fold transfusions to one
fetus and 10-fold in one pregnant woman with a twin pregnancy. Experience
transfusions of washed donor erythrocytes and at the same time 20% al solution
Bumina indicates that their timely implementation allows
significantly prolong the course of pregnancy against the background of satisfactory
high fetal blood parameters and perform delivery close to the due date
childbirth When managing such patients, one should strive for delivery
at a gestational age of 36-37 weeks.
For successful intrauterine treatment of severe forms of hemolytic tumor
fetal illness, timely treatment of pregnant women with high
risk for the development of this disease in a specialized perinatal
center. There is well-known data that shows: when wives contact
Shchin to the center until 18 weeks of pregnancy, all intrauterine transfusions were
taken before fetal edema develops. If you apply late - after 24 hours
during pregnancy, 81% of women began treatment against the background of existing
fetal edema. Thus, a special role in ensuring good results
therapy for hemolytic disease belongs to the antenatal clinic.
Risk of complications directly related to diagnostic interventions
when performing only cordocentesis, slightly exceeds 1%.
Total fetal losses during pregnancy and the early neonatal period are not
exceed the population level. When carrying out long-term internal
uterine interventions - namely transfusions - risk, eu
naturally increases. This is due to three main reasons:
1. Interventions are carried out against the background of the initial pathological condition
fetus
2. There is a significant load on the fetal cardiovascular system
by introducing volumes of blood comparable and sometimes exceeding the total
fetoplacental volume of circulating blood.
3. The motor activity of the fetus significantly complicates the performance of tasks.
telny intrauterine manipulations.
Monitoring the condition of the fetus during the intervention to avoid
load on his cardiovascular system and the development of severe bradycardia, about
is determined by constant cardiac monitoring of cardiac rhythm
mom. If signs of disturbances in the functional state of the fetus appear
the rate of transfusion should be reduced until it stops completely. This
is especially important in the edematous form of hemolytic disease, since it develops
the swelling is due to cardiovascular insufficiency developing
against the background of impaired fetal-placental circulation.
The motor activity of the fetus significantly complicates the conditions for performing
transfusions and can cause severe damage to the vessels of the umbilical cord
us and fetal organs. To immobilize the fetus, myo-
relaxant pipecuronium (Arduan). Arduan has no effect on the frequency of sulfur
daily contractions of the fetus and at a dose of 0.1 mg per 1 kg of estimated fetal weight
causes complete immobilization within 40-50 minutes. Immobilization
fetus allows to reduce the duration of intrauterine interventions, meaning
significantly reduce the incidence of cases where the end of the puncture needle comes out of the lumen
umbilical cord vessel and therefore avoid transfusion of donor blood into the amnio
tic cavity and the need to perform repeated cordocentesis in the center
to continue the transfusion.
Pregnancy pregnancy during isoserological conflict. Bank current
scarcity is characterized by a large number of complications, which include:
sewing due to an increase in the frequency of spontaneous miscarriages (13%) and
premature birth (up to 10%), anemia, OPG-gestosis, bleeding in the
the subsequent and early postpartum periods. The number of purulent septa increases
logical diseases in mothers and newborns.
Hemolytic disease of the newborn. Significant hemolysis of erythro
fetal cytoplasm usually leads to the development of a severe form of hemolytic
any disease that ends in antenatal fetal death or child death
ka in the first hours of life due to cardiopulmonary failure. However, in
In most cases, the disease develops quickly after birth, which is why
promotes the entry of a large number of antibodies into the child’s blood when
violation of the integrity of the placental vessels, as well as increased conglutination
onic activity of the child’s blood. Plays a significant role in the pathogenesis of hypertension
decreased enzymatic activity of the newborn’s liver. Normal in
reticuloendothelial cells as a result of hemolysis of red blood cells from hemo
globin produces free (or indirect) bilirubin, which is then
liver with the participation of a system of enzymes, of which the main one is gluten-
curonyltransferase, combines with glucuronic acid and turns into
conjugated (or direct) bilirubin. The latter dissolves well in
water and is excreted by liver cells into the bile ducts and then removed
with urine and feces.
In newborns in the first days of life, the activity of liver enzymes is still
low, and even physiological hemolysis leads to accumulation in the blood of
increased amount of free bilirubin (physiological hyperbilirubin
binemia) and to the so-called physiological jaundice of newborns. At
hemolytic disease, when intense hemolysis is layered with decreased
the liver’s ability to transform bilirubin occurs in pathological
chemical accumulation of free indirect bilirubin in the blood of a newborn.
Free bilirubin circulates in the blood in the form of complexes with albumin
However, in this state it does not penetrate cell membranes. If you know
significant accumulation of direct bilirubin, its connection with albumin is disrupted
xia, and it easily penetrates from the vascular bed through cell membranes into
tissues, especially tissues rich in lipids - adipose, nervous. Transition
bilirubin in the tissue is promoted by an insufficient amount of albumin, a shift
acid-base state towards acidosis, the presence in the blood is increased
a large number of substances that compete with bilirubin when binding to albumin
min (hormones, free fatty acids, salicylates, sulfonamides, etc.).
In the cells of the nervous system, bilirubin exhibits its toxic effect,
disrupting the processes of cellular respiration. This leads to dysfunction
central nervous system, i.e. to the development of clinical symptoms of biliru-
bin encephalopathy (nuclear), which may result in
or death of the child, or persistent neurological impairment that persists
for life.
CLINICAL CARD. Hemolytic disease of the newborn
has the following flow options:
1) hemolytic anemia without jaundice and dropsy;
2) hemolytic anemia with jaundice;
3) hemolytic anemia with jaundice and dropsy.
Hemolytic anemia without jaundice and dropsy
ma) is rarely found in its pure form. Anemia is usually detected on the 2nd
and 3 weeks of life and progresses rapidly. The number of red blood cells decreases
up to 2 x 1012/l, hemoglobin - up to 60-80 g/l. Anemia is not associated with increased
hemolysis of red blood cells, and with suppression of bone marrow function. With anemia
In the clinical form of the disease there is no reticulocytosis, erythroblastosis, hyperbilization
Binemia. Anemia is normochromic or hypochromic and relatively
microcytic. The prognosis is favorable.
Hemolytic anemia with jaundice (yellowish form) occurs
most often. It can have a mild course with moderate but prolonged
increased bilirubin levels without enlargement of the liver and spleen, but often with
subsequent moderate anemia.
A mild form of the disease is more often observed when the blood does not match the ma
mother and child based on group antigens of the ABO system.
Severe icteric form of hemolytic disease is sometimes detected already
at the birth of a child: his skin is pale icteric, liver and
enlarged ventricles, decreased muscle tone and reflexes, insufficiently active
scream. Even with a severe course of the disease, the child at birth may look
the baby is healthy and pink, but already in the first hours of life jaundice appears
tenderness of the skin, which quickly intensifies. The child becomes a dream
lethargic, lethargic, muscle tone and reflexes decrease, activity is impaired
sucking and further, if active treatment is not started, distinct
symptoms of bilirubin encephalopathy or kernicterus. First Sims
symptoms are a decrease in sucking activity and changes in muscle tone
SA - the appearance of stiff neck. Then hyperes join
thesia, restlessness, screaming, oculomotor disturbances (“symptom
setting sun"), respiratory distress, palpitations, sudden
temperature rise to 40-41 °C (pyrogenic effect of bilirubin) and
death is coming. In the agonal period, hemorrhagic phenomena are often noted.
niya - hemorrhages in the skin, intestines, lungs. Before death may develop
There is pulmonary edema and, more often, hemorrhagic in nature.
In some cases, recovery occurs after kernicterus, all
symptoms disappear, the baby becomes active, sucks well, increases
body weight varies. However, in most cases, it is later revealed
neurological consequences: from minor motor disorders (coordination
tion of movements, gait) to significant disorders combined with deafness
that and intellectual impairment.
In the clinical picture of severe icteric form of hemolytic disease
the degree of anemia of the child at the time of birth does not have a decisive prognosis
stical meaning. The main indicator of the severity of the disease is
the rate of increase in bilirubin in the blood.
For hemolytic anemia with jaundice and dropsy (edema form)
The fetus often dies in utero. This is the most severe form of the disease.
If the fetus does not die, then the child is born prematurely and has the character
New appearance: pale mucous membranes and skin, visible
petechiae and hemorrhages. Noteworthy is the large belly due to
ascites and enlarged liver and spleen. The number of red blood cells in the blood is not
higher than 1.5 x 1012/l, hemoglobin content up to 80 g/l, significantly increased
the number of nuclear forms of erythrocytes (“fetal erythroblastosis”).
A positive direct Coombs test helps in diagnosis, proving
the presence of blocking antibodies fixed by the child’s red blood cells, decrees
indicates Rh conflict. This is also evidenced by the level of bilirubin in
cord blood exceeding 51 m km ol/l (according to Van den Berg), the presence
anemia, normoblasts and reticulocytosis. To make a diagnosis it is very important
The mother has an anamnesis (indications of spontaneous abortions, death
birth, death of a child from jaundice in the first days after birth).
TREATMENT OF YELLOW FORM OF HEMOLYTIC DISEASE
aimed at combating hyperbilirubinemia and preventing the development of bilirubinemia
bin encephalopathy.
The most effective way to reduce bilirubin levels is
replacement blood transfusion. Indications for it in full-term babies are t
positive Coombs test, hemoglobin content below 90 g/l, biliru
bin 342 µmol/l, rate of increase (per hour) of bilirubin above 6.0 µmol/l and
its level in umbilical cord blood is 60 µmol/l. Its essence is
to replace the donor’s blood with the child’s blood containing defective,
hemolyzed red blood cells, sometimes free antibodies and, most importantly,
zom, breakdown products of hemoglobin (bilirubin). Donor's blood is temporarily
fulfills the normal function of blood. The child's own hematopoiesis for the first time
time is suppressed. For replacement blood transfusions, roofing felt was previously used.
to Rh-negative blood. It was further shown that in the child’s blood there is almost
does not contain free antibodies, they are predominantly associated with red blood cells
mi and, therefore, can be used for transfusion of less scarce
Rh positive blood. This has been tested and widely used, but in the most
in severe cases of the disease, it is preferable to use Rh-negative
blood. For ABO incompatibility, blood of group 0(1) is used, matching
with the child's blood according to the Rh factor. The number of blood transfusions determines
at the rate of 150-160 ml per 1 kg of body weight, on average it is administered during surgery
500 ml of donor blood, the same amount of child’s blood is removed (or
50 ml less). If after the first replacement blood transfusion
should increase, the bilirubin level rises again to values close to
to critical, repeated replacement blood transfusions are required.
To combat hyperbilirubinemia, the greatest
the effectiveness of which was noted when performed 12-24 hours after
regular blood transfusion in the amount of 2 bcc.
CONSERVATIVE TREATMENT OF HEMOLYTIC DISEASE OF NEWBORNS
includes intravenous drip administration of protein-containing solutions with glucose (albumin solution 10%, phenobarbital, zixorin, after 5-7 days - carbolene, vitamin E).
If the syndrome of “thickening of bile” develops, it is necessary to prescribe a 5-10% solution of magnesium sulfate, 5 ml, 2-3 times a day, and irradiate the child with fluorescent lamps.
Phototherapy - irradiation of a child with light sources with a length
waves of 450 nm, which leads to the formation of an isomer of bilirubin, soluble in water, and therefore easily eliminated from the child’s body.
Feeding children with hemolytic disease with mother's milk can begin no earlier than the 5-10th day of life. Children who receive timely treatment develop well in the future.
During development kernicterus subsequently, organic damage to the central nervous system and mental retardation are detected.
Prophylaxis of hemolytic disease of newborns
The need for prophylactic administration is now generally accepted anti-O-gammaglobulin and after delivery (postnatal) non-immunized Rh-negative women 300 mcg (1500 IU) for 48-72 hours, as well as after an artificial abortion, ectopic
pregnancy and invasive procedures during pregnancy. This tactic reduces the likelihood of immunization in postpartum women from 7.5% to 0.2%.
Development opportunity isoimmunization during pregnancy served as the basis for studying the effectiveness of antenatal use of anti-D immunoglobulin. Studies have shown that its prophylactic administration at 28 and 34 weeks of pregnancy at a dose of 150 mcg in combination with postpartum prophylaxis reduces the likelihood of isoimmunization to 0.06%.