Causes of congenital pneumonia in a newborn. Pneumonia in newborns. Prevention of pneumonia in newborns
- Bilateral pneumonia in newborns
- Treatment of pneumonia in newborns
Pneumonia in a newborn is an inflammation of the lung tissue of an infectious nature. This disease is considered fatal to every baby. According to statistics, in 15% of cases premature babies are exposed to it, while only 2% of full-term children suffer from pneumonia.
There are several types of pneumonia:
- transplantacentral – congenital pneumonia in newborns;
- antenatal;
- intrapartum;
- postnatal.
Factors that cause the disease: toxoplasmosis, rubella, herpetic rashes, streptococcal and staphylococcal infections of various groups, listeriosis, the presence of bacterial, viral and fungal infections.
The causes of pulmonary inflammation can be very different. Quite often the disease appears as complications of acute respiratory diseases and sepsis. A special role can be played by underdevelopment of the respiratory system in infants, in which pneumonia occurs much more often. Pulmonary inflammation can be caused by prenatal hemorrhage, premature rupture of amniotic fluid, or the presence of acute or chronic diseases in the mother.
In medical practice, pathology occurs when pneumonia begins to develop in utero, that is, before the birth of the child. The causes of pneumonia are usually considered to be illnesses of the expectant mother during pregnancy. Viruses and infections enter through the blood and amniotic fluid. In some cases, the occurrence of pneumonia occurs under the influence of not one, but several factors at once. At this stage, it is possible to distinguish two methods of infection:
- bronchogenic method;
- hematogenous method.
The first method involves the entry of pathogenic microflora through the lungs, which most often occurs during childbirth. As for the second route, infection occurs directly through the blood from mother to child.
Signs of pneumonia in newborns
Usually, with any degree of pneumonia there are pronounced symptoms. These include the occurrence of shortness of breath, cough, increased body temperature in the infant, and the skin color acquires a pale gray tint. A sick baby may vomit directly during feeding, intestinal spasms, bloating, loose stools, lethargy in behavior, fatigue from sucking the breast, obvious cardiovascular disorders, and severe diaper rash. Pneumonia in infants has a severe course with a high probability of mortality. During this period, children’s immune system has not yet fully formed, so the respiratory system is considered unprotected. Pneumonia is the cause of active inflammatory processes and severe damage to lung tissue. At the same time, infants are always at risk for the development of complications and various types of pathologies in the respiratory organs.
The occurrence of intrauterine pneumonia in newborns is detected almost immediately after their birth.
In addition, after discharge, the mother and newborn will be constantly visited by a doctor and a nurse for a month. If you notice any unusual behavior in your child, you should report it immediately. In the first days of life, the baby is advised to regularly measure body temperature, so even a slight increase in temperature should not go unnoticed. Signs of pneumonia of any form in very rare cases are hidden and usually appear immediately when infection occurs.
Pneumonia in an infant involves diagnosing the disease. The doctor makes a conclusion based on a direct examination of the sick child in the presence of obvious clinical manifestations. In this case, one of the mandatory procedures is an x-ray examination. Children with congenital heart disease, pulmonary pathologies and pneumopathy require a special approach.
Return to contents
The development of bilateral pneumonia in newborns is characterized by the most complex form of progression and a high probability of mortality. The occurrence of serious consequences is due to an underdeveloped immune system, pulmonary hypertrophy and prematurity.
In some cases, if there is no effect from drug therapy, the only method of treatment is open sanitation of the formations through surgery. The operation is quite difficult for children, but is a necessary measure. A complete cure can only be guaranteed if the disease is detected at the initial stage. In premature infants, the following complications are observed with bilateral pulmonary inflammation: impaired cardiovascular activity, decreased hemoglobin levels in the blood, changes in the acid-base balance, pneumocystis and chlamydia.
Return to contents
For the treatment of pneumonia in newborns, as much time as necessary for complete recovery is allocated. The acute course of the disease after the start of a complex of therapeutic measures lasts approximately 14 days, after which a decrease in respiratory failure is observed, the child’s appetite increases and the nervous system stabilizes.
Further treatment is prescribed taking into account the possibility of increasing immunity and stopping all associated causative factors. With pneumonia, complications may develop in the form of abscesses, pleurisy, respiratory system disorders, cardiac pathologies, insufficient weight gain in the child, and acid-base imbalance.
For therapeutic purposes, in almost every case, antibiotics with a broad spectrum of action are prescribed for this disease. In addition, the child must be closely supervised during treatment. Hypothermia or overheating of the baby should not be allowed; the baby should ensure hygiene and cleanliness of the skin, and change body position in time. In this case, feeding should be carried out through a tube in order to facilitate the process and save the child’s strength. Only when the baby’s condition is considered satisfactory, in the absence of the slightest signs of intoxication and respiratory pathologies, can breastfeeding be allowed.
In addition to antibiotics, the child is injected with vitamins B1, B2, B3, B6, B15 and C, and is prescribed a number of physiotherapeutic procedures, such as electrophoresis, microwave, hot wraps with and without mustard. In particularly severe cases, blood and plasma transfusions may be performed. Pneumonia is treated exclusively in a hospital setting under the constant supervision of doctors. In this situation, it is possible to correct prescriptions and procedures at any time.
It is worth considering that pneumonia, especially bilateral, greatly weakens the child’s body and requires increased attention and monitoring of the child’s condition. That is why recovered children can get sick again. To prevent this, children can be prescribed a course of vitamin therapy lasting 4 months. At the same time, the child must be observed by a specialist for another whole year.
Pneumonia in newborns
Pneumonia in newborns - infectious inflammation of lung tissue - is one of the most common infectious diseases. It is dangerous for any baby, especially when it comes to bilateral pneumonia in newborns. Unfortunately, the statistics today are as follows: pneumonia in newborns is diagnosed in 1% of full-term and 10-15% of premature babies.
Types and causes of pneumonia in newborns
In medicine, the following types of pneumonia are distinguished depending on the cause of the disease:
- congenital transplacental (the pathogen enters the baby through the placenta from the mother);
- intrauterine antenatal, caused by pathogens that penetrated from the amniotic fluid into the lungs of the fetus;
- intrapartum, occurs when the baby passes through the mother’s birth canal infected with microorganisms;
- postnatal pneumonia, in which infection occurs after birth in a maternity hospital, in the neonatal pathology department (nosocomeal), or at home.
The most common causes of pneumonia in newborns are:
- infections of toxoplasmosis, listeriosis, rubella, herpes (with congenital transplacental pneumonia in newborns);
- streptococci of groups B and O, gestal mycoplasmas, tuberculosis and Haemophilus influenzae (for antenatal and intrapartum pneumonia);
- group B streptococci, cytomegaloviruses, chlamydia, Candida fungi and herpes virus type II (for intrapartum pneumonia);
- Klebsiella, Pseudomonas aeruginosa, Escherichia coli, Proteus, staphylococci (with nosocomeal aspiration pneumonia in newborns);
- mixed bacterial-bacterial, viral-bacterial.
Acquired domestic pneumonia most often occurs against the background of ARVI (acute respiratory viral infection) caused by adenoviruses.
Secondary pneumonia, which is a manifestation or complication of sepsis, aspiration syndrome, is often caused in newborns by streptococci, staphylococci or gram-negative flora.
Symptoms of pneumonia in newborns
In the case of intrauterine infection, doctors will detect signs of pneumonia in a newborn even before discharge, because often the first signs of pneumonia begin to appear immediately after the birth of the child.
If a mother and child are discharged home, a doctor must come to their home for patronage during the first month. He will monitor the baby’s condition, and he needs to talk about all the alarming symptoms, for example, the baby’s lethargy, frequent regurgitation and loose stools, refusal to breastfeed, and rapid fatigue when sucking.
If your child’s temperature rises, you should not wait for the doctor’s next visit. Call an ambulance immediately. Cough in infants may be mild, but it is important to immediately pay attention to coughing. The appearance of nasal discharge and shortness of breath in a child should also alert you. Shortness of breath leads to symptoms of blueness on the feet, face and hands. A sick child develops diaper rash more quickly.
There is no need to be afraid of missing pneumonia in your child, because signs of the disease rarely appear without a rise in temperature. And it needs to be measured periodically for preventive purposes.
A doctor who regularly examines and listens to a child can easily detect pneumonia.
What treatment is prescribed for pneumonia in newborns?
Broad-spectrum antibiotics are always used to treat pneumonia. The child needs careful care to avoid hypothermia and overheating. It is important to monitor the hygiene of his skin, often change the position of his body, and feed exclusively from a horn or using a tube. Doctors will allow breastfeeding of a sick baby only if its condition is satisfactory, namely, if intoxication and respiratory failure have disappeared.
In addition to the listed treatments, physiotherapy (microwave and electrophoresis), vitamins C, B1, B2, B3, B6, B15, the use of immunoglobulins, mustard and hot wraps twice a day, and blood plasma transfusions are also prescribed.
Consequences of pneumonia in newborns
Children who have had pneumonia (especially double pneumonia in newborns) are prone to recurrent illnesses. After discharge, they should be given repeated courses of vitamin therapy and bioregulators (aloe and eleutherococcus extract) for 3-4 months. And for 1 year the child will be under medical supervision.
Related articles:
| Aquadetrim for newborns Vitamin D is urgently needed for newborn children. It helps to absorb calcium and fluoride in the body, which in turn affects the proper development of the baby’s skeletal system. Unfortunately, the sun, a natural supplier of vitamin D, does not shine all year round. The drug Aquadetrim, an aqueous solution of this vitamin, comes to the aid of mother and baby. | Disorders in the digestive system of a newborn baby cause a lot of concern to his parents. One of the most popular drugs for the treatment of tummy problems that has proven its effectiveness is the drug smecta. You will learn how to give it to a newborn correctly from our article. |
| Hydrocephalus in newborns Hydrocephalus of newborns is a diagnosis that parents hear from doctors very often. This is a fairly serious disease that has dangerous consequences, but a timely diagnosis and correctly prescribed treatment can help a child overcome this disease. Read about the details of hydrocephalus in infants in our article. | Cerebral ischemia in newborns Cerebral ischemia in newborns is a common disease, but dangerous because it does not always manifest itself immediately. The reasons for it can be different, but the consequences are very serious. Therefore, it is very important to recognize cerebral ischemia as early as possible. In this article we will tell you more about this disease. |
womanadvice.ru
Pneumonia in newborns: prognosis, symptoms, causes, treatment
Pneumonia in newborns occurs when infected with pathogenic bacteria in utero or during childbirth. Just a few decades ago, this condition caused high mortality among children, but the pharmaceutical industry has created effective drugs. Modern drugs against pneumonia are capable of destroying most pathogens of congenital pneumonia within a short period of time.
Congenital pneumonia is diagnosed in 10-15% of children. Very often the disease is observed in premature infants and with fetal malnutrition.
- IMPORTANT TO KNOW! Grandmother’s method of treating pneumonia SHOCKED doctors. Fast and efficient!
The prognosis for a child’s life depends on the correctness of treatment tactics and timely detection of pathology. The problem is relevant enough to leave its causes unattended, so we invite readers to read the article to the end.
Pathology of the lungs in premature infants

The causes of disease in premature infants can be divided into the following categories:
- Transplacental - when the pathogen penetrates the mother’s placenta if she has bacterial or viral infections;
- Antenatal - bacteria infect the fetal respiratory tract by penetration from the amniotic fluid;
- Intranatal - microorganisms enter the lungs when the child passes through the birth canal or from the environment when a pregnant woman undergoes a Caesarean section;
- Postnatal - infection in the maternity ward or at home.
Pneumonia in newborns is caused by a special spectrum of microorganisms, which requires the prescription of a special group of antibiotics in the treatment of the disease. For viral infections, the prognosis for the course of the disease in newborns depends on the state of the baby’s immune system and has specific features, which we will consider below.
- IMPORTANT TO KNOW! Doctor Galina Savina tells her PERSONAL story of victory over pneumonia! To defeat PNEUMONIA you need to drink...
Risk of illness after caesarean section
After Caesarean section, congenital pneumonia occurs when infected with the following microorganisms:
- Herpes viruses, rubella, toxoplasmosis, listeriosis;
- Bacterial pathogens: mycoplasmas, streptococci, chlamydia;
- Fungi of the genus Candida.
With a long course, congenital pneumonia is caused by a combination of flora, which is difficult to treat, which in ancient times led to high mortality in newborns.
Inflammation of the lung tissue that occurs after a Caesarean section in the mother is caused by streptococcus. The pathogen becomes the cause of purulent foci and sepsis (bacterial blood infection) when it multiplies rapidly, even against the background of antibiotics.
Home types of pneumonia in premature infants occur against the background of respiratory infections, adenoviral lesions, and streptococcal infections.
Pathogenetic signs in newborns

When a child is born healthy, this does not mean that he or she has a strong immune system. Some bacteria are antagonists to other pathogens of respiratory tract diseases. Thus, Proteus is able to destroy gram-negative bacteria.
Doctors' advice for pneumonia
In premature babies, there is underdevelopment of the protective factors of the alveolar tissue: surfactant defects are visible, there are no alveolar macrophages (cells that destroy microbes in the alveoli), the bronchial wall is weak. Against the background of such changes, it is difficult to assume that an encounter with infectious agents will not cause inflammatory reactions. The only salvation is the struggle of some representatives of the microbial world with others.
With bacterial contamination of the respiratory tract with Proteus, pneumonia caused by gram-negative bacilli cannot be traced for several months. Proteus is a pathogenic bacterium and can independently cause pneumonia in infants.
Interaction in the microbial world is a complex mechanism that has not been reliably studied by humans. It is obvious that the widespread use of antibiotics is not rational. The peculiarities of prescribing these drugs require control of the dosage and course of therapy. Due to a violation of the treatment regimen for infections with antibacterial agents, many bacteria have developed resistance, which complicates the process of their treatment.
What forms a negative forecast
A negative prognosis for pneumonia in newborns is formed by the following symptoms:
- Hypoxia of the brain with slowing of motor function and mental activity;
- Violation of the depth of respiratory movements and disorders of its rhythm;
- Irregularity of heart contractions;
- Increased respiratory acts (Cheyne-Stokes);
- Accumulation of toxins in the blood and the appearance of secondary changes in other organs.
If at least one of the above symptoms appears, the child is placed in the intensive care unit, as artificial ventilation may be required.
Pneumonia in premature babies has its own characteristics, unlike infants and infants under 1 year of age:
- Prevalence of respiratory symptoms and toxic reactions. When large amounts of carbon dioxide accumulate, swelling of the periorbital tissues appears. Over time, hypercapnia leads to depression of the central nervous system, the appearance of Cheyne-Stokes breathing;
- Increased temperature reaction and pulmonary complications - pneumothorax, atelectasis, pleurisy;
- Extrapulmonary complications - intestinal paresis, ear inflammation, blood clots, adrenal insufficiency;
- In premature infants, aspiration pneumonia often occurs, as they are prone to regurgitation;
- A typical picture of the formation of pathological changes in lung tissue: disseminated blood coagulation syndrome, sepsis;
- Unstable clinical condition of patients with fluctuations in laboratory and clinical tests.
Are you suffering from pneumonia?
The above-described signs of pneumonia in newborns depend on the cause of the pathology. If the inflammation is caused by pneumococcus, there is a high probability of complications or death. With this form, inflammatory foci quickly penetrate from one lung to another.
Congenital pneumonia in newborns is a dangerous condition. If the doctor does not prescribe antibacterial drugs, the child will quickly develop the following symptoms:
- Respiratory failure;
- Accumulation of carbon dioxide in the blood;
- Damage to brain tissue;
- Imbalance of water-salt metabolism;
- Heart overload;
- Increased heart rate.
The list of changes that pneumonia causes in premature newborns is endless. The final stage of the pathology is death (without adequate treatment).
How does congenital pneumonia occur in full-term infants?

Pneumonia at birth in full-term infants is benign. Its duration is 1-2 weeks, and then the patient’s condition gradually improves. Signs of respiratory failure rarely require relief with artificial ventilation.
In a full-term baby, the acute period of inflammatory changes in the lungs lasts 5-7 days. After the use of antibiotics, resorption of infiltrative foci in the alveolar acini is observed, which provides a favorable prognosis.
Segmental pneumonia at birth in premature babies is, at best, cured after 4 weeks. Due to this course of the disease, it is obvious that the fetus should be preserved in utero until the time of physiological labor, but this is not always possible.
Morphological symptoms
Symptoms of pneumonia in premature newborns can be divided into the following morphological types:
- Transplacental – consequences of widespread bacterial infection. Clinical symptoms of the disease occur due to generalized infection. Children with the pathology are born with asphyxia, cyanosis, and respiratory failure;
- The intrapartum type of pneumonia manifests itself in 2 variants. The disease can occur as a result of intracranial birth trauma, leading to respiratory failure. The second option is accompanied by the presence of a “light gap”. The child is born healthy, but after a few days he develops bouts of cyanosis, frequent regurgitation, and nervous agitation. Diarrhea and foam at the mouth may occur;
- Early neonatal – observed in the first days after birth. This type can be determined by the following signs: respiratory failure, lethargy, bluishness of the skin;
- Late neonatal - begins with manifestations of inflammation of the upper respiratory tract: fever, anxiety, rhinitis, regurgitation. Over time, other symptoms of inflammation of the pulmonary parenchyma appear: fever, cough, vomiting.
Is phlegm coming out poorly?
For a quick recovery, it is important that the mucus is expectorated and removed from the body, as pulmonologist E.V. Tolbuzina tells how to do this.
In premature babies, any of the above forms rapidly progresses and can cause death, so it is necessary to identify and treat the pathology in the early stages.
Danger level of pneumonia

Bilateral pneumonia in premature infants has a dangerously high probability of death. Serious consequences also occur against the background of primary immunodeficiency, severe malnutrition and prematurity.
The risk of respiratory failure increases with the presence of infiltrative fluid, foreign bodies, and liquid sputum in the lungs (against the background of cystic fibrosis). To empty purulent foci when antibiotics are ineffective, open sanitation of the formations by surgical method is necessary. Surgical intervention in premature babies is very difficult, but it is a necessary measure to save the life of the child.
With bilateral pneumonia in premature infants, the following complications are often observed:
- Pneumocystis;
- Chlamydia;
- Cardiac dysfunction;
- Changes in acid-base balance;
- Decreased hemoglobin and serum iron levels;
- Increased blood acidity.
The consequences of the disease in premature babies are too serious. Only with early detection of signs of infiltrative changes in the pulmonary parenchyma and the absence of provoking factors can a complete cure of the pathology be guaranteed.
Treatment time for infants
Congenital pneumonia is treated as long as pathogenetic symptoms of the disease exist. The acute period of the disease lasts about 2 weeks, after which the symptoms of respiratory failure decrease. When the condition of premature babies improves, their appetite increases and the central nervous system is restored. The resolution stage lasts 1-2 weeks.
The prognosis for pneumonia in premature infants depends on the state of the child’s immune system, the presence/absence of provoking factors, and the treatment tactics used.
The course of the pathology is complicated by the development of secondary pathological changes in the lung tissue:
- Abscesses;
- Pleurisy;
- Respiratory and cardiovascular failure;
- Hypotrophy of prematurity (lack of body weight);
- Violation of the acid-base balance of the blood.
Pneumonia of newborns is a dangerous pathology that requires constant analysis of the baby’s condition and immediate medical correction. It can only be treated in a hospital setting.
- PNEUMONIA! Write down a folk recipe, it helps a lot...
- Pneumonia, but I don’t really want to run to the doctors, then you need to know this...
- Tired of going to doctors? Write down a folk recipe, it helps a lot with pneumonia...
pneumonia.ru
Pneumonia in a newborn child: causes, symptoms, consequences

Pneumonia in a newborn baby can occur due to infection with pathogenic microorganisms in utero or during childbirth. Previously, this disease caused high mortality among infants, but today there are effective medications that have significantly reduced the mortality rate.
A fairly common problem is congenital pneumonia in newborns, the causes of which are caused by infection with herpes viruses, toxoplasmosis, streptococci, chlamydia, etc. This disease is diagnosed in 10-15% of children.
Causes of pneumonia in newborns
With the transplacental route of infection, the pathogen penetrates the maternal placenta. In the antenatal variant of pneumonia, the source of bacteria is amniotic fluid.
The intrapartum route involves the entry of microorganisms into the baby’s lungs during passage through the birth canal or from the environment (in the case of a Caesarean section). The postnatal variant of pneumonia is caused by infection either in the maternity ward or at home.
Signs of pneumonia in a newborn
The clinical picture of the disease, which developed in the prenatal period, is noticeable immediately after birth. Symptoms are most pronounced if the pregnancy lasted less than 37 weeks, as well as in the case of asphyxia. If a child is born with pneumonia, the following phenomena occur:
- very weak first cry;
- bluish tint of the skin and mucous membranes (this is very noticeable on the limbs, lips and tongue);
- intermittent noisy breathing with moist wheezing;
- in children born at term, the temperature is about 40 degrees, and in premature babies - about 35 degrees;
- possible swelling of the lower extremities;
- weight loss, delayed falling off of the remnant of the umbilical cord, there are cases of inflammation of the umbilical wound;
- Frequent regurgitation, possible vomiting.
If pneumonia occurs in a newborn during childbirth, symptoms appear after about two days. These include an increase in temperature up to 40 degrees, loss of appetite, cyanosis of the lips and paranasal area, drowsiness. In full-term infants, breathing is noisy and frequent, while in premature infants it is weak and infrequent.

Prognosis of congenital pneumonia in newborns
It is necessary to take into account a complex of factors, including the state of the child’s immunity and the treatment tactics used. Pneumonia in a newborn is treated as long as the pathogenetic symptoms persist. The acute period lasts about two weeks, after which the symptoms of respiratory failure decrease. The improvement in condition is accompanied by an increase in appetite. The duration of the resolution stage is usually 1-2 weeks.
The duration of treatment for pneumonia in a newborn child is delayed in the presence of secondary changes in the lung tissue. These include pleurisy, abscesses, and respiratory failure. When congenital pneumonia occurs in newborns, the consequences are less significant the more qualified the doctors are.
A competent specialist takes into account the differences in the course of the disease in full-term and premature babies and chooses the appropriate treatment tactics. So, if pneumonia is diagnosed in a newborn, the consequences will not necessarily be severe, so parents should not panic ahead of time. If the disease develops at home, then the main thing is to consult a doctor as quickly as possible.
Pneumonia in newborns has a negative prognosis in the presence of factors such as brain hypoxia, increased respiratory activity, uneven heartbeat, and accumulation of toxins in the blood. Such symptoms are an indication for placing the child in the intensive care unit, since there may be a need for artificial ventilation.
In a full-term infant, the duration of the acute period is usually 5-7 days. After the use of antibacterial drugs, infiltrative foci resolve, which provides a favorable prognosis.
Bilateral pneumonia in newborns
With such pneumonia there is a high risk of death. The situation is especially dangerous if the disease develops against the background of prematurity, severe malnutrition, or primary immunodeficiency.
There is a high risk of respiratory failure if foreign bodies, infiltrative fluid, and liquid sputum are present in the lungs. If antibiotics have no effect, purulent foci are drained surgically. A premature baby has a very difficult time undergoing surgery, but this is the only way to save his life.
Common complications of bilateral pneumonia in prematurely born babies include chlamydia, pneumocystis, cardiac dysfunction, increased blood acidity, and a drop in hemoglobin levels.
Treatment of pneumonia in newborns
A necessary condition for recovery is hospitalization of a sick baby in a specialized hospital while maintaining optimal temperature and humidity conditions. Under no circumstances should you rush to be discharged, even if it seems that the child is clearly feeling better. In the hospital, pneumonia in newborns is treated as much as necessary in order to protect them from severe consequences and complications.
Sometimes a problem arises such as parents’ mistrust of the attending physician. It is quite natural that against the backdrop of a severe illness in a child, the mother and other family members experience severe stress. They are trying to find out from third-party sources how and how much pneumonia in newborns is treated, for some reason trusting anonymous advisers on forums more than medical staff.
It is important to consider that all cases of this insidious disease are individual. Without knowing all aspects of the situation, it is impossible to immediately give an unambiguous answer as to how long it takes to treat pneumonia in newborns. One child copes with the disease faster, another takes longer. You should not immediately blame the medical staff for incompetence if the disease is not treated as quickly as concerned parents would like.
Treatment includes measures such as regular monitoring of breathing and body temperature, nutritious meals (breastfeeding is best), detoxification therapy, and oxygen therapy.
Detoxification therapy is carried out by intravenously administering saline solutions and diuretics to the baby. This is done in order to speed up the filtration of blood by the kidneys.
Oxygen therapy consists of giving a sick baby humidified oxygen through a mask. This is necessary to normalize breathing and oxygen levels in the blood. To stimulate the immune system, vitamin therapy (large doses of vitamin B and C) is prescribed.
Traditional methods of treatment for pneumonia in newborns should not be used. Sometimes honey is recommended as the most effective and safe remedy, but any experiments are unacceptable when it comes to the health of such young children.

Prevention of pneumonia in newborns
The mother of the child can take some steps that will reduce the likelihood of developing this dangerous disease. Among the preventive measures:
- planned pregnancy management, including tests to diagnose congenital diseases;
- treatment of foci of chronic infection;
- avoiding contact with infected patients;
- a thoughtful diet based on fruits, vegetables and herbs;
- fractional meals;
- walk in the fresh air for at least 2 hours per day;
- night sleep - at least 8 hours;
- giving up alcohol and smoking.
Prevention of pulmonary pneumonia in newborns is ensured by compliance with sanitary and epidemiological standards in maternity hospitals. In addition, after discharge from the hospital, parents must properly care for the baby. To do this, you need to follow the doctor’s recommendations and protect the child from contact with sources of infection.
Comments powered by HyperComments
Statistics on the incidence of congenital pneumonia indicate that the disease most often develops in women with a burdened history of infection during pregnancy. In premature babies and in children with aspiration, pneumonia occurs one and a half times more often than in children born at term.
Causes of congenital pneumonia in a newborn
Congenital pneumonia in a child is called such because infection and inflammation occur during pregnancy or childbirth, and external factors play a minor role in this disease. The cause of such pneumonia is an infectious pathogen that is present in a woman’s body and can be activated during pregnancy, or the pathogen is activated during childbirth. Therefore, according to the time of development, all congenital pneumonias can be divided into antenatal (those that develop in utero until the time of birth) and intranatal (develop during childbirth). In each case, the cause may be a different microorganism or virus, which is important for correct diagnosis and treatment.
The causes of antenatal pneumonia are often viruses, since it is during this period that the child is vulnerable to their effects. For the development of an infectious process in the lungs, it is necessary that the virus begins to act in the last trimester, and if earlier, this can cause birth defects. The most common causes of congenital pneumonia in utero include the TORCH group. These include toxoplasmosis, rubella, cytomegalovirus and herpes virus, as well as some others. Each such pathogen has its own structural and developmental characteristics, and, accordingly, treatment.
Toxoplasmosis is a disease caused by Toxoplasma gondii, which is a protozoan microorganism. The pathogen is transmitted through cats, which are its carriers, or through poorly cooked meat. Infection can occur during pregnancy in the last stages, and then it will cause pneumonia in the child. If infection occurs before pregnancy, then the woman may not be aware of the presence of such an antigen in her body, since the clinical picture is nonspecific.
Rubella is an acute viral disease that is transmitted by airborne droplets and poses a potential threat to the fetus in the early stages due to the development of congenital defects. The virus can provoke the development of pneumonia in a child if the mother becomes infected just before giving birth.
Cytomegalovirus infection is a disease that can be transmitted by airborne droplets, sexual contact and contact. More than 60% of people are affected by this virus, but not everyone develops the disease. When a pregnant woman is infected, the virus can penetrate the placenta and induce the development of an inflammatory process in many organs - lungs, liver, brain.
Herpes is a virus that has a tropism for the nervous system, but it can also cause pneumonia with the same frequency. There are two main types: labial herpes, which is transmitted by airborne droplets and contact, and genital herpes, which is sexually transmitted. The first virus is important in the development of antenatal pneumonia, and the second - intrapartum, since infection occurs through contact with the affected genital organs.
Infections from the TORCH group are dangerous in terms of pneumonia when infected precisely in the last stages or just before childbirth. As for other reasons, they can also be an etiological factor.
Congenital pneumonia can also be caused by bacteria - chlamydia, mycoplasma, listeria, ureaplasma, candida, trichomonas. Their role in the development of congenital pneumonia in a child is important already at the stage of infection before or during childbirth. Ureaplasma and Trichomonas are sexually transmitted infections that can rarely cause pneumonia in an absolutely healthy child. Such infections, including candida, infect the already sensitive body of a premature baby or a child with immunodeficiency. Chlamydia and mycoplasma are intracellular microorganisms that play a primary role in the development of congenital pneumonia of bacterial etiology. They can cause respiratory tract infection in a child already at birth or in the first hours thereafter, if appropriate conditions are present.
Summarizing the above reasons for the development of congenital pneumonia, we can say that viruses can be the most common cause of this, but at the same time bacteria also play a role in the development of inflammation. The pathogenesis of pneumonia in a newborn is not so dependent on the etiological factor. Any pathogen for the development of an infectious process first enters through the feto-placental barrier. Whether it is a virus or a bacterium, it has an affinity for the lung tissue and enters the lungs through the bloodstream. The peculiarities of the lung tissue of a newborn are such that the alveoli are not opened and can become a substrate for the development of infection. Inflammation occurs there, which is already revealed by symptoms at birth due to insufficient lung function, because it is after birth that the lungs must work at full strength. Therefore, the inflammatory process is further activated with the first breath and symptoms appear.
Risk factors
There are children who have a higher risk of developing congenital pneumonia than others. Risk factors include:
- pathologies of pregnancy and maternal illness lead to disruption of the formation of the normal protective barrier - the placenta;
- infectious diseases of the mother, especially from the TORCH group, increase the risk of infection through the placenta and the development of an infectious lesion;
- Prematurity increases the risk of infection due to weak immune defenses;
- birth conditions and external interventions increase the risk of infection.
Symptoms of congenital pneumonia in a newborn
Congenital pneumonia is characterized by the fact that symptoms begin to appear immediately after birth or in the early postpartum period. If the clinical picture develops within 72 hours from the moment of birth, then this also refers to the concept of congenital pneumonia, but here the intranatal route of infection already plays a role. If pneumonia is caused by intrauterine infection with a certain virus, then often, along with symptoms from the respiratory system, there are manifestations from other systems. This must be taken into account when diagnosing congenital pneumonia, since the approaches to treating pneumonia of viral and bacterial etiology are slightly different.
The first signs of the disease appear immediately after birth. The general condition of the child may be severe due to severe respiratory disorders. The child is born with a cyanotic or pale gray complexion; there may be a petechial rash due to intoxication. The child has a weak cry and depressed innate reflexes due to hypoxia of the central nervous system due to an infectious lesion. Therefore, the child's Apgar score may be low, preventing immediate skin-to-skin contact. Sometimes babies with congenital pneumonia require resuscitation measures immediately after birth, and sometimes the degree of respiratory impairment is not so pronounced. Manifestations of pneumonia are respiratory disorders, which are clinically defined by shortness of breath. Shortness of breath, depending on the severity, is characterized by retraction of the intercostal spaces and areas above and below the collarbones, retraction of the sternum during breathing. Against the background of respiratory failure, tachypne and rapid heartbeat are determined. All this indicates a clear pathology of the respiratory system and requires immediate further verification.
If pneumonia is caused by a virus from the TORCH group, then there may be other symptoms of a generalized infection. For example, cytomegalovirus has an affinity for the child’s brain and liver, therefore, when affecting the fetus, this infection causes severe brain damage in the form of ischemic lesions and cysts, as well as liver enlargement and severe jaundice with bilirubin encephalopathy. Therefore, pneumonia against the background of these symptoms may be a specific manifestation of this virus.
Congenital pneumonia, caused by the rubella virus, can manifest itself as a characteristic rash on the child’s body with symptoms from the respiratory system.
Bacterial pneumonia has peculiarities of its course, since the inflammatory process is purulent in nature. More often they develop during the first two days, when the baby’s condition sharply worsens. Against the background of severe shortness of breath, symptoms of intoxication appear - the child’s body temperature rises, or if it is a premature baby, hypothermia most likely develops. The newborn refuses the breast, loses weight and becomes restless. All this, together with respiratory symptoms, should suggest pneumonia.
Complications and consequences
Complications of congenital pneumonia depend on the type of pathogen and can be immediate or delayed. If the pathogen quickly causes destruction of lung tissue, complications such as the spread of infection are possible. Such a common infection when the lungs are affected can quickly cause the pathogen to enter the bloodstream and develop bacteremia. Sepsis can be fatal for such a young child. Other systemic complications may include hemorrhagic syndrome, disseminated intravascular coagulation syndrome, hemodynamic disorders, persistence of fetal communications and, against this background, acute cardiovascular failure.
Pulmonary complications may include the development of pleurisy, atelectasis, and pneumothorax.
The consequences of pneumonia can be more serious if the lesions are systemic. If pneumonia is viral, then there may be damage to other organs and systemic manifestations - congenital defects, chronic forms of infections and intellectual impairment.
Diagnosis of congenital pneumonia in a newborn
Diagnosis of congenital pneumonia is always complicated by the fact that there can be many variants of insufficiency of the respiratory system and it is necessary to differentiate these conditions. If the diagnosis of congenital pneumonia is confirmed, it is important to diagnose the type of pathogen, since treatment tactics are different. Therefore, diagnosis must begin with the mother’s anamnestic data on the course of pregnancy and childbirth. It is very important to find out whether the mother has infections and whether a study was conducted on the TORCH group, because these are the most serious pathogens.
A feature of congenital pneumonia, mainly in a premature baby, is an unclear objective picture. Auscultation data, as a rule, do not give a clear picture of pneumonia, since a bilateral process can equally indicate pneumonia and respiratory distress syndrome. Therefore, additional laboratory and instrumental research methods can be considered the main diagnostic methods.
Tests in a newborn have their own characteristics due to physiological reasons - the number of blood cells increases to ensure normal cellular respiration, and on the fifth day a physiological leukocyte crossover occurs. Therefore, changes in laboratory data that may indicate pneumonia are not as specific as in older children. But the benefit of pneumonia may be indicated by an increase in the number of leukocytes over time and the absence of leukocyte crossover on the fifth day of the child’s life. This indicates a bacterial infection, and one can rule out a viral etiology of pneumonia or think about an association of viruses and bacteria.
Sometimes, while treating pneumonia in a child, it is not possible to achieve results, then the mother is examined to determine the specific pathogen. After all, the mother in this case is the main source of infection for the child, while the child has not yet formed antibodies and they cannot be determined. To do this, a serological test of the mother’s blood is carried out to determine antibodies to certain infections. The level of antibodies of the immunoglobulin class G and M is determined. In this case, special reagents are used that make it possible to determine the level of these antibodies to a special infection. If there is an increase in the level of immunoglobulin G, then this virus cannot be involved in the development of pneumonia in a child, since it only indicates an old infection. But if immunoglobulins M are detected, then this indicates an acute infection, that is, there is a high probability that the fetus is also infected. Among the special tests, if sexually transmitted infections are suspected, a vaginal smear is also examined. This is necessary for bacterial pneumonia, when it is possible to accurately determine the pathogen and its sensitivity to antibacterial agents.
Instrumental diagnostics make it possible to accurately establish the diagnosis of lung damage and clarify the localization of the process. X-ray signs of congenital pneumonia in a newborn are deflation of the lungs and increased vascular pattern in the initial stages of the disease, and then inflammatory-infiltrative changes of a confluent nature appear. But if the child is premature, then an x-ray does not allow an accurate diagnosis between pneumonia and hyaline membrane disease, since the changes are identical in both pathologies. Therefore, there is a need for additional treatment measures.
Differential diagnosis
Differential diagnosis of congenital pneumonia should be carried out with hyaline membrane disease, primarily in premature infants, as well as with aspiration syndrome, congenital lung malformations, diaphragmatic hernia, heart pathology and central nervous system injuries, which are accompanied by respiratory failure. Hyaline membrane disease is a pathology of premature babies that develops against the background of insufficient surfactant in the lungs. The pathology is characterized by similar changes in X-rays in the form of “cotton” lungs, so such children need the administration of exogenous surfactant.
Congenital defects of the respiratory system can also manifest as respiratory disorders, so they need to be excluded. As for congenital heart defects, the clinical manifestations appear at a later time, and ultrasound of the heart allows accurate differentiation. Some “critical” heart defects may manifest themselves in the first hours, in which case there will be an appropriate history to identify the defect in utero.
Treatment of congenital pneumonia in a newborn
Treatment of congenital pneumonia should begin immediately after diagnosis. The approach to treatment is complex, taking into account many links in the pathogenesis and conditions for caring for the child. Therefore, you need to start treatment with a regimen.
The most appropriate mode for a newborn with pneumonia is the incubation mode, since the correct temperature mode can be used. The average temperature in the incubator for babies is 32-34 degrees, and the air humidity is 80-90% in the first days. It is very important to provide oxygen support, which can also be done directly into the incubator.
Feeding a child with congenital pneumonia should continue with breast milk, total caloric intake should be limited but with an increase in the frequency of feedings. Oxygen support is required for the child, since metabolic disorders have a very bad effect on the cardiovascular system. If the child is in an incubator, free oxygen may be supplied or through a mask. If the child is weak or premature and correction of the act of breathing itself is necessary, then special oxygen supply devices with constant positive pressure in the respiratory tract or mechanical ventilation are connected if necessary.
Only after such measures can we talk about other drug therapy.
If the causative agent of pneumonia is precisely identified, then treatment should be as specific as possible. Of course, if the causative agent is of viral etiology, then antibacterial therapy is used together with antiviral therapy. If congenital pneumonia is caused by cytomegalovirus with systemic damage to organs and systems, then therapy is carried out with special agents from the group of interferons.
- Viferon is an antiviral drug that contains recombinant human interferon and is active against most viruses from the herpes group. It acts against cytomegalovirus, hepatitis virus, and some bacterial infections through immunomodulatory effects. The drug is available in the form of ointment, gel, and suppositories. For the treatment of newborns it is recommended in the form of rectal suppositories. The dosage of the drug is 500,000 IU twice a day, and then according to a special regimen with monitoring of the child’s blood tests for specific antibodies in the future. Side effects are possible: thrombocytopenia, itching at the injection site, redness, and allergies. Precautionary measures - not recommended for use in children with severe congenital immunodeficiencies.
- If toxoplasma is confirmed as a manifestation of pneumonia and generalized infection, specific treatment is carried out.
Spiramycin is an antibiotic from the macrolide group, which is the drug of choice for the treatment of toxoplasmosis. It has the highest activity against Toxoplasma, inhibiting the synthesis of its wall proteins, but does not have a teratogenic effect. The dosage of the drug is 6-9 million IU per day. Side effects of spiramycin are paresthesia, skin sensitivity disorders, numbness of the arms and legs, tremors, impaired bile outflow, as well as protracted jaundice in a child.
- Antibiotics for pneumonia in newborns are considered the main and mandatory means of treatment. In this case, treatment is carried out with two drugs, the methods of application of which are only parenteral (intramuscular and intravenous). Treatment is carried out in stages: for the first course, a b-lactam antibiotic (semi-synthetic penicillin or 2nd generation cephalosporin) is prescribed in combination with aminoglycosides. If this combination of drugs is ineffective, second-course drugs are prescribed - cephalosporins 3-4 with amikacin or vancomycin.
Netromycin– an antibiotic of the aminoglycoside group, the active substance of which is netilmicin. The drug is effective against staphylococcus, Klebsiella, Escherichia coli and some other bacteria that play a significant role in lung damage in utero. In the treatment of pneumonia in newborns, a dosage of 15 mg/kg/day in 2 doses is used. Side effects - sleep disturbance, drowsiness or lethargy, damage to the renal parenchyma, stool disorders. Precautions - do not use if you have kidney damage.
Cefpir– antibacterial agent of the 4th generation of the cephalosporin group. The drug has a bactericidal effect on many extracellular opportunistic microorganisms. In the treatment of pneumonia, this drug is used intravenously or intramuscularly. The dosage of the drug is from 50 to 100 milligrams per kilogram of weight per day. The drug does not have a pronounced effect on the organs of a newborn, so it can be used for treatment. Side effects are possible in the form of diarrhea in the baby or disruption of the formation of intestinal biocenosis, so treatment is carried out together with probiotic preparations.
- Probiotics are necessarily used in such children to correct disturbances in the bacterial composition of the intestines.
Acidolac- a drug that contains lactobacilli, which form lactic acid and do not allow pathogenic bacteria to multiply. Thanks to this, the drug creates favorable conditions for the development of beneficial intestinal microflora. Lactobacillus reuteri, which is part of the medicine, is completely resistant to antibiotics, and therefore can be used in the complex treatment of just such pathologies. The dosage sufficient to restore microflora and normalize the function of intestinal motility in children is half a sachet per day in two doses. The powder can be dissolved in milk and given to the baby before feeding. Side effects are diarrhea, stool discoloration, and rumbling in the intestines.
Vitamins and physiotherapeutic treatment for pneumonia in a newborn are not used in the acute period. A mother can take vitamin supplements while breastfeeding her baby, even after he has recovered from courses, which will improve the prognosis for the baby.
Traditional treatment of congenital pneumonia
Treatment with folk remedies can only be used by the mother, and prescribing any herbs or infusions to the child is contraindicated. If the mother is diagnosed with any infection, then folk remedies can be used in combination with medications.
- Medicinal herbs are highly effective in treating infections that are chronic in the mother and can cause illness in the child. To prepare medicinal tea, you need to take 25 grams of mint, 50 grams of licorice and the same amount of wild rosemary leaves, boil this over low heat for five to ten minutes and then strain. You need to drink this tea three times a day, half a cup.
- A decoction of marshmallow, cinquefoil, and rosehip herbs is especially effective against cytomegalovirus infection. You need to make tea from a liter of water and these herbs and drink in small sips throughout the day. The course of treatment is four weeks.
- Tea made from chamomile leaves, oak bark and anise bark has antiviral and antibacterial activity. To prepare it, all ingredients need to be poured with water and boiled. Take half a glass in the morning and evening.
Homeopathic medicines It can also be successfully used for the mother, which improves the child’s response to drug therapy and speeds up his recovery.
- Antimonium Tartaricum is a homeopathic remedy of natural plant origin. Used in the treatment of pneumonia in children with severe moist rales in the sixth dilution. Dosage of the drug: two drops every six hours in tea or water for mother. Side effects are possible in the form of allergic reactions. Precautionary measures - do not use the drug if you suspect congenital defects in the baby.
- Hepar sulfur is an inorganic homeopathic medicine. Used in premature babies with breathing problems and surfactant deficiency. Method of using the drug in capsules. Dosage of the drug: two capsules three times a day. Side effects are possible in the form of hyperemia of the skin of the hands and feet, as well as a feeling of heat. Precautionary measures - do not use in combination with sorbents.
- Veratrum viride is a homeopathic remedy that has a composition of organic agents and helps to activate the body's natural defenses, including in the fight against viral agents. The drug is used for pneumonia with severe heart failure in a child. Dosage four drops twice a day, half an hour before meals at the same time. The course of treatment is three months.
- Aconite is a homeopathic remedy of natural plant origin, which is recommended for use in the acute period in the third dilution, followed by a transition to the same dosage of Bryonia. Dosage – three drops per fifty grams of water for mother three times a day. The first drug is taken for two weeks, and then switched to the next one. Side effects include tremor of the child's fingers or chin.
It is necessary to take into account that folk and homeopathic remedies are not a priority in treatment and can only be used on the recommendations of a doctor.
Pneumonia in a newborn is usually called an acute disease of an infectious nature (the causative agents of the disease are microorganisms), which is characterized by damage to the respiratory (participating in gas exchange) parts of the lungs.
In this case, the child may exhibit symptoms of systemic (affecting not only the site of introduction of the pathogenic microorganism) inflammation. Often, signs of pneumonia in infants are reduced to respiratory distress, while suspicion of pneumonia in a newborn arises only during an X-ray examination (the image usually shows an area of shading in the lower parts of the lungs - this is the focus).

Since from the very first minutes of life the location of the child is determined by the obstetric or pediatric department, pneumonia in a newborn can be congenital or nosocomial.
Pneumonia in a newborn is usually divided, depending on the microorganism, after the introduction of which inflammation in the lungs occurred, into the following types:

There are factors that predispose a child to develop congenital pneumonia. The latter are prematurity of the fetus, complicated pregnancy, the consequences of severe suffocation during childbirth, as well as infectious diseases in the mother (then the infection can be transmitted directly from the mother; this is called the transplacental transmission mechanism: through the placenta - the organ through which the fetus is nourished, with blood mother).

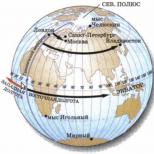
Illustration of the trans-placental route of transmission in general.
An additional risk is a caesarean section (removal of the baby through an incision in the abdominal wall and uterus, respectively). Also, the reasons why congenital pneumonia occurs may lie in violation of the sanitary and epidemiological regime by hospital staff (for example, insufficient care of the child’s respiratory system). In addition, the introduction of the pathogen into the newborn's body can occur during a blood transfusion. Unfortunately, such consequences of medical activities are not so rare.
In principle, there are different possible causes of pneumonia in a newborn. However, most often the pathogenic microorganism ends up in the child’s lungs transplacentally (consequences of blood exchange with the mother), as well as in the case of aspiration (inhalation by the newborn) of the infectious agent along with amniotic fluid (the fluid that was the habitat for the fetus before birth). That is, the most common is congenital pneumonia.
In the first day of a child’s life, if he has inflammation in the lungs, it may be difficult for the doctor to interpret the resulting signs of illness as symptoms of congenital pneumonia. To understand the true cause of breathing disorders in a child, you need to know about the indirect signs of inflammation in the lungs. The earliest signs are dysfunction of the gastrointestinal tract, which consists of an increase in food debris in the stomach mixed with bile.

Symptoms include poor breastfeeding and constant regurgitation while feeding the baby. At the same time, symptoms of general intoxication of the body may be observed: pallor (even “gray”) of the skin,

enlargement of the spleen (splenomegaly) or liver (hepatomegaly). And sometimes even pathological jaundice occurs - a yellow discoloration of the skin due to a disruption in the processes of bile formation and bile excretion (there is also physiological jaundice: it is usually distinguished from pathological jaundice by how much bilirubin was detected in the patient during a biochemical blood test).

But the symptoms of pneumonia typical of an adult patient, such as fever (increased temperature) and cough, are completely uncharacteristic of pneumonia in infants.
If a newborn does not have congenital pneumonia, but acquired (nosocomial), it may be hidden behind conditions requiring resuscitation measures (severe suffocation and other critical respiratory disorders of the child). All these are objective consequences of the natural (until treatment is prescribed) course of lung disease. Often, such a development of events accompanies premature babies, especially if a cesarean section was performed (an additional risk factor for infection).
Diagnostic measures when identifying a disease
To confirm the diagnosis of pneumonia in a newborn, it is necessary to obtain radiographic data,

and also perform sowing

from the birth canal of the mother and the respiratory tract of the child to understand whether the microflora (microorganisms) in them is the same. Also important signs are an increase in the level of white blood cells in the blood (an indicator of inflammation), an increase in the level of C-reactive protein within 72 hours after birth (also confirms inflammation). In addition, there may be the following symptoms: the presence of purulent sputum during the first intubation (insertion of a breathing tube into the baby’s respiratory tract), a significant enlargement of the newborn’s liver in the first days after birth, as well as inflammation in the placenta, which is detected during its special histology (study of the tissue structure ) research. All these signs, especially if several of them are found together, indicate with a high degree of certainty the presence of the disease.
In addition to the above signs, important data indicating the possibility of pneumonia in a newborn may be previous infectious diseases in the mother: respiratory infections during pregnancy, chronic inflammation of the female organs or kidneys. Complications that occur in the mother after pregnancy are also important. They indirectly indicate its not entirely favorable course.
In this case, while listening to the child’s lungs, wheezing will be detected in them, as well as weakening of breathing (muffling of breathing sounds).

Listening to the heart will give an increase in the number of its contractions in one minute (this is called tachycardia) and some muffling of the heart beats.
Basic treatment measures
Pneumonia can be treated successfully (including the consequences of the disease) if optimal conditions for caring for the patient have been previously created.
Non-drug treatment consists mainly of inhalation (based on inhalation) measures: the newborn is given a humidified air-oxygen mixture. At the same time, the tension (quantity) of oxygen in the blood is monitored. Treatment is often accompanied by transferring the child to artificial ventilation (insertion of a tube into the trachea with a parallel supply of oxygen from a special apparatus).

Drug treatment of the disease usually involves antibacterial therapy. They are usually treated with penicillin antibiotics in combination with aminoglycosides (ampicillin is a broad-spectrum antibiotic). If the causative agent of the disease is identified and it is Pseudomonas aeruginosa (Pseudomonas aeruginosa, usually a nosocomial rather than a congenital infection), then the disease is treated with cephalosporins (also antibacterial drugs) of the 3rd generation (ceftazidime) with aminoglycosides (netilmicin).
In general, it should be noted that the choice of antibacterial drug, first of all, depends on how many pathogens were found in the lungs of a particular child, what groups of microorganisms they belong to, as well as on what consequences the disease had already caused at the time of its diagnosis .
If the disease is particularly severe, treatment may include drugs whose action is aimed directly at the newborn’s immune system. In children, it is not yet perfect, so it is better to avoid such effects. However, if the baby's condition is truly critical, immune therapy may be necessary.
Summary
If you calculate the percentage of mortality due to pneumonia in newborns, you will get figures of about 5-10%. In this case, lethality depends, first of all, on the processes against which the disease occurred, as well as on the degree of maturity of the child (pneumonia in premature infants occurs more often and is accompanied by serious complications). The prognosis worsens if the disease occurs while the child is in the intensive care unit.
To understand whether a disease is congenital or nosocomial, you need to take into account how much time passed from the moment the child was born until the moment when the first symptoms of the disease were noticed.

Mother's behavior during and before pregnancy plays a major role in the prevention of pneumonia in newborns. In addition, it is important to comply with the sanitary and epidemiological regime, use the material once, as well as distribute infants in a ratio of no more than two newborns per nurse in the intensive care unit.
Pneumonia is an inflammation of the lung tissue, which has an infectious or bacterial nature, and still remains one of the most dangerous diseases, the final outcome of which can be death. According to the World Health Organization (WHO), pneumonia is one of the 10 diseases that can lead to death, especially in childhood. According to statistics, the most vulnerable to this disease are children in the first year of life, most often premature.
Causes of the disease
Due to their physiological and anatomical characteristics, infants are often susceptible to respiratory diseases, which is due to their fragile immunity and imperfect respiratory system. The lumens of the larynx, bronchi, trachea and nasal passages are still very poorly developed, and the mucous membrane tends to swell quickly, which complicates the child’s already shallow breathing. In addition, infants are not able to get rid of phlegm on their own, and its excessive accumulation in the bronchi slows down the healing process and causes severe coughing.
Infants are susceptible to two types of pneumonia:
- Congenital – when infection occurs in the womb or during childbirth.
- Acquired – occurring in the first months of a baby’s life.
As a rule, the causative agents of the disease are:
- streptococci;
- pneumococci;
- staphylococci;
- herpes virus;
- chlamydia;
- mycoplasma;
- cytomegalovirus;
- fungus type Candida;
- Haemophilus influenzae and Escherichia coli.
Congenital form of the disease

The cause of the congenital form of pneumonia is a consequence of a disease suffered by a woman during pregnancy, in which viral agents enter the child’s body through the placenta or amniotic fluid. The severity of the congenital form of the disease can vary and depends on a number of factors:
- The length of time that elapses from the moment of infection to the birth of the baby, the longer it is, the more difficult the disease will progress;
- The causative agent of the disease;
- The degree of term of the newborn;
- Individual characteristics of the child’s body, immunity.
Infection in the womb
If the fetus is infected in the womb, through the blood (hematogenous method), the disease is diagnosed immediately after the baby is born and is characterized by the following symptoms:
- Weak muscle tone - the child’s movements are sluggish, limbs hang down, muscles are in a relaxed state;
- The color of the skin varies from gray to bluish;
- Immediately after birth, the baby does not cry or his cry is very weak, and his breathing is hoarse and intermittent, more like groans;
- Unstable body temperature. For premature babies, a decrease to 35˚ C is typical, and for newborns born at term, an increase to 40˚ C;
- The baby has no or weakly expressed congenital reflexes (breathing, swallowing, sucking). After birth, such children are on artificial ventilation and receive nutrients through a special tube;
- After birth, the baby exhibits obvious signs of asphyxia;
- Foamy discharge from the mouth is possible.
Infection during childbirth

Infection of the baby can occur during its passage through the infected birth canal; in this case, pathogenic microorganisms penetrate the baby’s lungs (bronchogenic method), and signs of inflammation that appear on days 2-3 are characterized by the following symptoms:
- Lack of appetite, breast refusal, severe weight loss;
- Indigestion, diarrhea, cramps and bloating;
- Frequent regurgitation and vomiting;
- A bluish tint to the nasolabial triangle and tongue;
- Pale or earthy-gray skin color;
- Whistling, noisy, arrhythmic breathing;
- Increase in body temperature to very high values;
- Sometimes a superficial cough;
- Poor breathing in premature babies;
Due to the lack of immunity, pneumonia is a rather serious disease for newborns and can lead to aggravating consequences. When such a diagnosis is made, urgent medical treatment of the baby is necessary in a hospital or maternity hospital.
Acquired pneumonia

Acquired or postnatal form of pneumonia can develop in infants in the first months of life, at home or in a hospital setting, for several reasons:
- Viral diseases;
- Hypothermia or overheating of the child;
- Asphyxia during childbirth and penetration of amniotic fluid into the respiratory tract;
- Intrauterine brain damage;
- Birth injury;
- Deviation in the development of the respiratory system;
- Premature birth;
- Childbirth by caesarean section;
- Ingestion of vomit into the respiratory tract of a newborn.
Symptoms of the disease

In most cases, acquired pneumonia develops as a consequence of improper treatment of colds and viral diseases. What symptoms should young parents pay attention to in order to identify and recognize incipient pneumonia, advises Dr. Komarovsky:
- The main signs of the disease are a dry, superficial cough and fever, which cannot be brought down with the help of antipyretics;
- ARVI, cold, severe dry cough, lasting more than a week;
- The skin becomes pale gray;
- A child's attempt to take a deep breath is accompanied by a strong cough;
- The frequency and depth of breathing is impaired, shortness of breath appears;
- Blue discoloration in the area of the nasolabial triangle.
During the primary disease, the symptoms of pneumonia are mild and very similar to the manifestations of acute respiratory infections and acute respiratory viral infections. Signs of the disease may not appear immediately, but several days after the onset of the inflammatory process. The onset of the disease is accompanied by a sharp rise in temperature, weakness, refusal to eat and general malaise. With further development of the disease, the above symptoms appear.
The level of severity of acquired pneumonia depends on the degree of formation of the newborn’s body; in premature infants, the clinical picture of the disease will be more severe than in babies born at term.
Pediatrician Evgeniy Komarovsky warns that in some cases, pneumonia in newborns is hidden and is not accompanied by symptoms such as cough and fever, which makes timely diagnosis quite difficult. Therefore, the task of parents and doctors is to identify and recognize other signs of the disease in a timely manner. Komarovsky notes that the latent form of the disease is characterized by symptoms such as lethargy, drowsiness, thirst and lack of appetite.
Types of lung tissue damage in pneumonia

With any type of pneumonia, the degree of damage to the lungs is not the same, and this determines how severe the symptoms of the disease will be. Based on the location and severity of damage to the lung tissue, several types of inflammation can be classified. The most common type of pneumonia is focal pneumonia, which affects a small area of the lung; it is characterized by symptoms such as a wet cough, fever and increased sweating. With total inflammation, one of the lungs is completely affected, and bilateral inflammation covers both organs at the same time,
Diagnosis and treatment
Dr. Komarovsky advises: at the first suspicion of pneumonia, the baby’s parents should urgently contact a medical institution and undergo the appropriate examination:
- Visual examination of the skin and mucous membranes of the baby;
- Listening to the lungs for the presence of wheezing and the duration of inhalation and exhalation;
- Tapping the chest to identify inflamed areas;
- Biochemical and general blood test;
- General urine analysis;
- Bacteriological cultures of sputum;
- X-ray or fluorography of the chest.
When a diagnosis of pneumonia is made, the infant requires immediate hospitalization. The sooner treatment is started, the more likely a successful outcome of the disease and the absence of complications.
In most cases, treatment of pneumonia begins with broad-spectrum antibacterial drugs, either orally or intramuscularly.
In addition to them, the doctor may prescribe immunomodulatory drugs and vitamin complexes.
An important role in successful anti-inflammatory therapy is played by herbal preparations or medications that relieve swelling from the mucous membranes, transform a dry cough into a wet one, and promote the rapid discharge of sputum.
To relieve symptoms of intoxication, measures are taken to administer intravenous saline solutions.
Dr. Komarovsky advises accompanying the treatment of a sick baby by following basic rules of hygiene and prevention. The room where it is located must be subject to daily wet cleaning, ventilation, and maintain optimal levels of temperature and humidity. The child should drink as much fluid as possible and eat food more often, but in small portions, so as not to overload the gastrointestinal tract. A good help in complex treatment, after the patient’s condition improves, will be a massage that helps cleanse the respiratory system of phlegm.
An important preventive measure to combat pneumonia is vaccination against pneumococcal infection.
Possible complications

Timely and competent treatment gives effective results, the disease can be defeated within 10 - 15 days. Belatedly started antibacterial therapy and not receiving pneumococcal vaccination on time are fraught with a number of complications:
- Cough that persists for a long time after the end of treatment;
- Inflammation of the lungs caused by pneumococci can further lead to otitis media and meningitis;
- If the serous membrane of the respiratory organs (pleura) is damaged during the course of the disease, there is a possible risk of developing pleurisy, causing the child severe chest pain;
- A protracted illness can most likely take a chronic form, and any further respiratory diseases of the child can provoke another inflammation of the lungs;
- Sepsis of lung tissue.
Prevention of pneumonia

The disease is easier to prevent than to cure, therefore, to reduce the risk of infection, pediatrician Evgeniy Komarovsky advises parents of infants to follow some preventive measures:
- Competent planning and management of pregnancy (timely testing and regular visits to the antenatal clinic);
- Timely detection and treatment of inflammatory processes during pregnancy;
- Compliance with the regime and a healthy lifestyle;
- Vaccination against pneumococcus;
- Feeding a newborn with breast milk;
- Proper and balanced nutrition for the mother;
- Avoiding contact with infected people.
In the last few years in Russia, the list of mandatory vaccinations has included vaccination against pneumococcal infection, represented by the Prevenar (USA) and Pneumo-23 (France) vaccines. The first vaccination is given to infants starting at 2 months of age, the second to children from 2 to 5 years of age.
Children's doctor Evgeniy Komarovsky believes that timely vaccination against pneumococcal infection can protect a child in the future from the occurrence of such serious diseases as pneumonia, tonsillitis, otitis media and meningitis.
Pneumonia, or pneumonia, is a lesion of the lung tissue primarily of infectious origin. How does pneumonia occur in newborns and what consequences can this disease have?
Causes and risk factors
Pneumonia in newborns occurs when infected with pathogenic microorganisms in utero, during the passage of the birth canal or in the first days of life. Depending on the type of infection, there are several ways of developing the disease:
- Transplacental (through the placenta from the mother's blood): herpes simplex virus, rubella, cytomegalovirus, listeria, treponema pallidum, mycobacterium tuberculosis.
- Perinatal (during childbirth or after cesarean section): chlamydia, mycoplasma, E. coli, streptococci, Haemophilus influenzae, anaerobes.
- Postnatal (after birth): respiratory viruses, Staphylococcus aureus and Staphylococcus epidermidis, bacteria of the intestinal group, fungi.
Finding out the exact cause of pneumonia in a newborn is quite difficult. Microbiological studies are carried out only in a maternity hospital or a specialized children's department. If a child is treated at home, it is not always possible to identify the culprit of the problem. In this case, the doctor focuses on the symptoms of the disease and selects therapy taking into account all possible pathogens.
Important aspects:
- Viral pneumonia develops extremely rarely in children in the first months of life.
- Severe forms of the disease in a child are most often associated with infection with mixed bacterial flora.
- In infants, the causative agent of severe pneumonia that occurs without fever is usually chlamydia.
- Up to 10% of all pneumonias that occur in the first days of life are caused by Haemophilus influenzae.
- Many children develop a mixed infection, which causes blurred symptoms of the disease and difficulty in diagnosis.
- 70% of all household pneumonia in newborns are caused by streptococci.
- Fungal infection occurs mainly in children who have been on mechanical ventilation for a long time.
- Prolonged pneumonia (more than 1.5 months) occurs in weakened children with immunodeficiencies and some developmental defects. The consequences of such pneumonia can affect throughout life.
Risk factors for developing the disease:
- intrauterine infection;
- maternal illnesses during pregnancy;
- long difficult labor;
- asphyxia during childbirth;
- mechanical ventilation after birth;
- prematurity;
- malformations of the lungs and heart;
- rickets;
- immunodeficiency states;
- hypothermia.
Representatives of atypical flora: chlamydia and mycoplasma play an important role in the development of pneumonia in infants. This disease is characterized by a protracted course without a rise in temperature. In second place in terms of frequency of occurrence are bacterial pneumonia caused by anaerobes and intestinal flora. Staphylococcal lung disease outside the hospital is extremely rare. Children older than 3 months are at increased risk of contracting respiratory viruses.

Symptoms
Symptoms of pneumonia will depend on the pathogen and the time of infection. With intrauterine infection, signs of the disease appear in the first minutes of life. Most children have asphyxia during childbirth. Even if the baby takes his first breath on his own, clear symptoms of respiratory failure appear within the first hours.
Signs of pneumonia in a newborn due to intrauterine infection:
- dyspnea;
- noisy difficulty breathing;
- pale skin;
- refusal to eat;
- frequent regurgitation;
- inhibition of basic reflexes;
- weight loss.
All symptoms in a baby develop within 24 hours after birth. On days 1-2, the body temperature rises and the baby’s condition worsens. There may be signs of damage to other organs (heart, digestive tract, brain). Treatment of such a baby is carried out in the intensive care unit.
Symptoms of pneumonia in a newborn with postnatal infection appear somewhat later. An increase in body temperature is observed on days 2-3 of life. In the first days, the child's condition may be satisfactory. Along with signs of respiratory tract damage, other symptoms appear:
- diarrhea;
- conjunctivitis;
- pustular skin lesions.
These signs do not occur in all children. The severity of the manifestations of the disease will depend on the prevalence and severity of the process.
At the first sign of pneumonia in your baby, be sure to call a doctor!
Pneumonia in infants aged 1-6 months has its own distinctive features:
- rise in body temperature;
- runny nose with mucous or purulent discharge;
- nasal congestion;
- cough;
- dyspnea;
- refusal to eat;
- poor sleep;
- excitement followed by lethargy.
Dangerous symptoms of pneumonia in infants and newborns:
- increased respiration rate of more than 60 per minute in newborns and more than 50 in children 1-6 months;
- moaning or grunting breathing;
- pronounced retraction of the intercostal spaces;
- cyanosis of the nasolabial triangle;
- severe pallor;
- lethargy, confusion.
If any of these signs appear, you must call an ambulance and prepare for hospitalization in the children's department.

Complications
Pneumonia is a dangerous condition that threatens the life of a child. With untimely diagnosis and inadequate treatment, the following complications may develop:
- purulent pleurisy (damage to tissue around the lungs);
- lung abscess;
- heart damage;
- DIC syndrome;
- sepsis.
If complications develop, the child is treated in intensive care in a specialized children's department.

Treatment methods
Pneumonia in newborns requires a special approach to diagnosis and treatment. Pneumonia in children in the first days and months of life is often severe, with a high risk of complications. In premature and weakened babies, the clinical picture of the disease may be blurred, which does not allow a quick diagnosis to be made. Mixed bacterial-fungal or bacterial-viral lung damage also significantly complicates diagnosis.
Non-drug therapy
Feeding a child with severe lung damage with signs of respiratory failure is carried out parenterally or through a tube. Breastfeeding is possible if the baby is in satisfactory condition. If the newborn does not take the breast, an adapted artificial formula is selected for feeding.
Throughout the treatment, it is important to prevent the child from hypothermia and to monitor the cleanliness of the skin. The baby should be turned over regularly, monitoring the occurrence of possible rashes, as well as preventing the appearance of diaper rash.
Drug therapy
Pneumonia in newborns is a reason for prescribing antibacterial therapy. The choice of drug will depend on the causative agent of the disease, the severity of the condition and the age of the child. For the treatment of newborns, drugs from the group of protected penicillins are used in combination with III-IV generation cephalosporins or aminoglycosides. If pneumonia occurs after discharge from the maternity hospital, cephalosporins and drugs from the group of glycopeptides are mainly used for treatment.
In infants aged 1-6 months, drugs from the macrolide group are used to treat pneumonia. The active use of these drugs is explained by the frequent development of atypical (chlamydial) pneumonia. For pneumonia caused by common bacterial flora, cephalosporins are used. The course of treatment is 7-10 days.
Use antibiotics only as prescribed by a doctor and in strictly prescribed dosages!
After a course of antibiotic therapy, the effectiveness of the drugs must be monitored. To do this, a sputum culture is taken to identify pathogenic microorganisms. If the child is treated at home, the assessment of the effectiveness of therapy is based on clinical data (the condition of the baby, the severity of symptoms of the disease). The baby’s well-being improves after 2-3 days of using antibiotics.
Other treatments for pneumonia:
- infusion therapy (infusion of solutions that normalize the functioning of the body).
- enzyme preparations;
- immunomodulators;
- vitamins (during recovery).
Pneumonia of newborns is a serious pathology that requires close attention of parents and doctors. Self-medication for pneumonia in a baby in the first days and months of life is not acceptable. The consequences of untimely and inadequate treatment can be very sad. When the first signs of trouble appear in your child, you should definitely consult a doctor.