Foamy mucus in stool. Mucus in the stool in adults: causes and treatment. Rectal ulcer
It is not accepted in society to talk about dysfunction of excretion. The problem with the health of this area of the body is so delicate that sometimes people prefer to make do with the simplest pharmaceutical products. Patients with intestinal diseases are in no hurry to seek qualified help. It is the psychological discomfort from communicating with a doctor that explains the late detection of quite serious diseases. These also include conditions characterized by the presence of impurities in feces. Regardless of whether an adult has mucus in the stool or a child is sick, you will need to undergo a diagnosis.
general information
Normally, the presence of mucus in the digestive system in moderate quantities is a physiological process. The secretion is necessary to protect the intestinal mucosa from toxins and mechanical injuries from dense fecal matter or dietary fiber, and to facilitate bowel movements.
Mucus is constantly secreted in the digestive system, since the adult body forms a bolus of food in real time and removes it through the anus to the outside. These are dead epithelial cells. Inflammation or intoxication changes the consistency of the secretion, its quantity, composition, and the result is:
- violation of the integrity of the mucous membrane, cracks;
- bleeding;
- hemorrhoids are formed;
- mucus plugs form;
- impurities of various types appear.
Depending on the pathology, the secretion of the intestinal glands may differ in color and shape:
- white mucus in the stool or its transparent version in large quantities indicates pathological changes in the distal parts of the intestine;
- yellow – the result of taking antibiotics, the formation of hemorrhoidal cones, polyps;
- gray – problems of the descending department;
- green – bacterial infection;
- pink – suppuration;
- black – tumor process;
- small flakes of undifferentiated color – pathology in the small intestine;
- admixture of blood - erosive and ulcerative processes of the mucous membrane, cracks, hemorrhages.
What is mucus in stool
The wisely designed human body constantly secretes mucus to protect tissues and organs. An oily, jelly-like substance of white or transparent color is formed by the secretion produced by the intestinal glands. Part of it consists of epithelial cells, leukocytes on the surface of the mucous membrane. This secret plays an important role:
- protects against the influence of toxic components of feces;
- protects the intestinal lining from the mechanical effects of coarse food fibers;
- prevents chronic constipation due to difficult passage of stool.
The adult body constantly produces and eliminates viscous contents - this is normal. Thanks to mucus, stool can easily move through the intestinal tract and exit through the anus. With inflammatory changes in the intestines, serious problems arise with the release of lubrication. As a result:
- in the absence of cracks, damage to the mucous membrane, bleeding, and development of hemorrhoids;
- Serious pathologies are possible with excessive secretion production;
- A change in the color of the discharge indicates the presence of problems that require treatment.
Causes of pathology
The trigger for hypersecretion of mucus in men and women can be for different reasons: lifestyle, eating habits, diseases. The most common causes of secretion are:
- drinking water with impurities dangerous to the mucous membrane of the food tube;
- rough, poorly digestible food;
- fasting or dieting;
- hypothermia;
- constant use of medications;
- swimming in cold water;
- alcohol;
- stress;
- smoking;
- unwashed vegetables, fruits;
- unbalanced diet.
Stool and mucus cause diseases:
- irritable bowel syndrome with vomiting, dyspepsia, constipation;
- imbalance of intestinal microflora;
- tumors of the gastrointestinal tract;
- Crohn's syndrome;
- sensitization of the body;
- infections;
- inflammatory processes.
Discharge in stool may be the result of:
- helminthiasis;
- viral pathologies;
- exacerbations of respiratory diseases;
- hemorrhoidal disease with complications;
- peptic ulcer of the stomach and duodenum;
- intestinal polyposis;
- inflammation of the pancreas, large intestine;
- colitis of spastic origin;
- diverticulosis;
- proctitis and paraproctitis;
- cystic fibrosis.
Infectious lesions of the intestine and the connection with mucus secretion
Intestinal infections are acute lesions of the gastrointestinal tract that occur when pathogenic microorganisms/viruses penetrate the mucous membranes and are characterized by inflammation of the intestinal membranes. Almost all intestinal infections are accompanied by increased secretion of mucous components, which are needed to protect the intestines from toxins and pathogens. Foodborne illnesses, poisoning, and intestinal infections have the same set of symptoms, which may include:
- increase in temperature to febrile levels (38°C and above);
- repeated vomiting with foam, pieces of undigested food and an unpleasant odor;
- spasmodic pain in the lower abdomen, less often in the epigastric area;
- lack of appetite and poor absorption of any food, including water.

Intestinal infections
Intestinal infections are dangerous due to the rapid development of dehydration, so the patient is recommended to drink plenty of fluids. It is necessary to give a person 1 teaspoon every 10-15 minutes. To normalize the water-electrolyte balance, it is better to use ready-made saline solutions, for example, “Hydrovit” or “Regidron”. To quickly remove toxic and blood poisoning substances, sorbents are used: “Activated carbon”, “Polysorb”, “Filtrum”.

"Regidron"
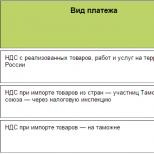
Table. Intestinal infections in which white mucus may appear in the stool.
| Name of the disease | What it is |
| Dysentery | Infectious lesions of the digestive tract with predominant damage to the final sections of the large intestine, provoked by Shigella (shigellosis). Causes acute systemic intoxication and can cause death of the patient. |
| Escherichiosis | Acute inflammation of the intestines and other segments of the digestive tract caused by infection with E. coli. |
| Salmonellosis | A type of intestinal infection that develops when salmonella bacteria enter the human body. The main route of infection is the consumption of stale eggs and poorly processed meat from sick animals. |
| Amoebiasis | Chronic recurrent colitis with extraintestinal manifestations, symptoms reminiscent of dysentery. The main route of transmission is fecal-oral. |

Where does intestinal infection live?
Clinical manifestations
Symptoms of pathological secretion of the glands of the mucous membrane of the digestive system are varied, since they are caused by many reasons. But the main clinical, visually distinguishable manifestation is still the color and consistency of the mucus.
White mucus in stool
Viscous white discharge, reminiscent of jelly, in the stool of an adult indicates inflammation of the rectum, dysbiosis, mycosis of the rectum, irritation of the mucous membrane by microorganisms or poorly digested foods. Rough food or infection can provoke cracks, an allergic reaction, and exacerbation of chronic gastrointestinal diseases.
Mucus instead of feces
If instead of formed feces during defecation, mucus plugs that imitate snot come out of the anus, this means the inability of the digestive system to correctly form a bolus of food and pass it along the entire length of the intestine. Excessive irritation of the mucous membrane causes hypersecretion in a volume that the anal sphincter is unable to hold. The flow of mucus is accompanied by abdominal pain and hyperthermia.
The most serious situation is bloody discharge from the anus, which indicates a violation of the integrity of the intestinal mucosa as a result of erosive and ulcerative processes or tumors. Blood in the stool may be a sign of hemorrhoids. The danger lies in the development of uncontrolled bleeding, anemia, and cancer metastasis.
Yellow slime
The yellow color of the discharge indicates the presence of pus in the stool, the development of inflammation, the addition of secondary flora against the background of polyps, hemorrhoidal disease, dysbacteriosis, and intestinal infections.
Transparent slime
This is the safest option for hypersecretion of the glands of the mucous membrane of the digestive system. The reasons may be smoking, taking medications, coffee, hunger. The most dangerous is the development of spastic or membranous colitis. An examination by a specialist is required.
Pink slime
Pink secretion is a dangerous situation that most often occurs due to liver cirrhosis, peptic ulcer, Crohn's syndrome, allergic colitis, intestinal varicose veins of various locations, and diverticulosis.
Black slime
The most common cause of black secretion is taking vitamins or medications containing iron. But in the worst case scenario, this is a sign of a malignant neoplasm, therefore an urgent comprehensive examination is necessary in this case. A change in the color of mucus in the stool is associated with severe bleeding.
Brown slime
Most often, a brown secretion indicates insufficient pancreatic function or dysbacteriosis. However, sometimes this coloration of mucus can be caused by direct entry of mucus from the nose into the intestines during acute respiratory infections or acute respiratory viral infections, accompanied by a runny nose. In addition, a brown tint may indicate a secondary infection. Pus in the stool can also turn brown.
Symptoms of the disease
Usually people detect mucus in their stool not by chance, but in cases where something bothers them. That is, a large amount of mucus is one of the symptoms that signal the development of the disease.
In addition, patients usually feel:
Blood in stool
- severe abdominal pain, cramps;
- bloating and excessive gas formation;
- abdominal tightness, constipation or diarrhea;
- in severe cases, vomiting or other signs of intoxication;
- pain during defecation;
- blood or pus in the stool, possibly undigested food debris;
- change in the shape and consistency of feces, its nonspecific smell;
- mucus or bloody substance may remain on the patient's toilet paper or underwear;
- for respiratory diseases, characteristic symptoms of cough, nasal congestion, rhinitis and more;
- headaches and fatigue.
If you find these symptoms, as well as ichor or white discharge with feces, you should immediately consult a doctor and get tested to determine the cause of this phenomenon.
What it is and how to treat it can only be told by a competent specialist, and there is no need to self-medicate.
Diagnostics
A change in the color of the secretion of the glands of the mucous membrane of the digestive tube requires consultation with a qualified specialist: a therapist, gastroenterologist, proctologist, infectious disease specialist.

It is necessary to donate blood for a detailed analysis and conduct a bacteriological examination of stool. Sometimes a consultation with a surgeon or oncologist may be necessary. In any case, the clinical and laboratory examination of the patient includes:
- OAC, OAM – screening of the patient’s general condition;
- biochemical tests: blood for sugar, cholesterol, tumor markers, antibodies to hepatitis viruses, and so on;
- coprogram;
- endoscopic instrumental research methods: FGDS, anoscopy and others as recommended by a doctor;
- Ultrasound of the abdominal cavity and pelvis;
If this minimum is not prescribed:
- sigmoidoscopy, colonoscopy, irrigoscopy;
- blood electrolyte balance.
Transparent
If a dense film begins to appear in the stool, this may be the first sign of developing membranous colitis. As a rule, such a pathology is provoked by a rather long period of taking antibiotics, non-steroidal anti-inflammatory drugs and drugs aimed at combating flatulence.

However, colitis can also make itself felt against the background of colds, constipation and frequent smoking.
Features of treatment
Therapy for pathologically altered secretion of the mucous membrane of the digestive system is subject to correction by general and special methods. Common ones include the nutritional system, lifestyle changes, the use of systemic medications, and background traditional medicine. The most common pathologies are treated with separate complex regimens.
Balanced diet
The diet should be based on fractional meals with meals every three hours. A serving should not exceed 200 g in volume. Food products are selected on an individual basis, taking into account intolerance to individual components and susceptibility to allergies. The drinking ration is calculated per kilogram of weight, at least 1.5 l/day. Steaming, baking, boiling. Fatty and salty foods should be avoided.
Medicines
Systemic therapy to relieve hypersecretion of digestive mucus aims to stabilize and maintain the function of the digestive system. For this purpose, pre-, pro-, dysbiotics, lacto- and bifidobacteria are used. This helps restore the natural intestinal microflora. In addition, they use:
- laxatives if the cause of hypersecretion is constipation;
- diarrhea is treated with lactulose derivatives;
- pain is relieved with antispasmodics;
- immunity is supported by immunostimulants and immunomodulators;
- intoxication is removed with sorbents or activated carbon, drugs based on it.
Relationship with diet
Increased mucus production can occur if a person does not follow a diet and allows long breaks between meals. Most often, this situation occurs in women who follow low-calorie diets or practice fasting. To prevent this from happening, it is necessary to adhere to the norms of fractional nutrition and monitor the daily diet, controlling the amount of starchy food in the menu. If the formation of mucous secretion is too active, it is necessary to reduce the consumption of the following foods and drinks:
- jelly;
- oatmeal porridge;
- pumpkin;
- beets, carrots and potatoes.

Proper nutrition is the key to health
Folk recipes
There are no special herbs or plants to normalize mucus production in the digestive system. However, herbal remedies that are used to treat any pathological changes in the digestive system are effective. They are loyal to stomach acidity and bile production. Here are some of them:
- ginger drink: the root of the plant (1 cm) is crushed and brewed with a glass of boiling water, cool, add a spoonful of honey, lemon juice, drink 50 ml three times a day before meals;
- herbal tea from chamomile, calendula, yarrow in equal parts (teaspoon) per glass of boiling water - drink throughout the day;
- kefir with honey: a tablespoon of buckwheat flour per glass of kefir, half a teaspoon of ginger, a spoonful of honey - the mixture is infused for 8 hours in the refrigerator, stirred, and drunk instead of breakfast.
All prescriptions are agreed upon with the doctor in advance.
Find and neutralize: treatment

To understand how to deal with this delicate, sometimes discomforting phenomenon, you need to analyze what accompanies the appearance of intestinal mucus.
Pay attention to the color: clear or white mucus indicates that its secretion is caused by physiological factors and does not indicate pathology.
If mucus appears in the stool infrequently, in small quantities, and your health is generally stable, you can try to correct the situation at home by taking the following steps:
- Adjusting your diet. Avoid spicy, salty foods. Limit consumption of strong coffee, heavy and canned foods. Avoid alcohol.
- Maintain drinking regime. Drinking enough fluids will prevent dehydration and help remove toxins from your intestines.
- Treatment with folk remedies will help improve the situation.
Treatment regimens for common pathologies
Treatment of hypersecretion of digestive mucus depends on the type of pathology on an individual basis. It is not recommended to change the schemes.
Inflammatory diseases
Altered mucus is most common in irritable bowel syndrome. They use antispasmodics (Trimedat, No-Shpu, Duspatalin), antidiarrheals (Loperamide, Imodium, Smecta), laxatives (Duphalac, Buscopan), antidepressants (Fluoxetine, Imipramine, Citalopram), probiotics (Enterozermina, Linex), prebiotics (Fervital, Lactulose , Lactofiltrum).
In second place is hemorrhoids. A combination of anti-inflammatory suppositories and liniments (Natalsid, Relief, Proctosan), hemostatics (Ditsinon, Vikasol), laxatives (Mukofalk, Bisacodyl), analgesics (Anestezol, Analgin), venotonics (Detralex, Troxevasin), anticoagulants (Heparin, Prednisolone) are used. Read more: how else to treat hemorrhoids at home
For the treatment of diverticulum, antibiotics (Flemoxin, Cefoxitin), analgesics (Mesacol), antihistamines (Suprastin, Tavegil), laxatives (Normaze, Mucofalk), antispasmodics (No-Shpa, Meteospasmil) are used.
Worm infestations
Dysbacteriosis
Imbalance of intestinal microflora is corrected with antibiotics (Amoxicillin, Oksamp), antifungals (Fluconazole, Flucostat), bacteriophages (Sextaphage, Intesti), sorbents (Polysorb), probiotics (Bifilakt) and prebiotics (Lactofiltrum, Fervital), enzymes (Creon), immunomodulators (Immunal, Echinacea).
Drug therapy
The use of medications is prescribed taking into account the diseases that caused the discharge:
- Interferon and Arbidol are recommended for intestinal inflammation or diseases of viral origin.
- Ersefuril and Furazolidone have proven themselves in the treatment of intestinal infections.
- Viferon and Regidron are indispensable drugs in the treatment of intestines caused by a viral pathogen.
- Tinidazole and Piperazine are used for helminthic infestations.
- Antifungal suppositories and Amphotericin are prescribed for fungal intestinal diseases.
- Linex, No-shpa and Furazolidone are effective drugs that are used to treat colitis, dysbacteriosis and inflammation of the rectum.
- The use of chemical and radiation therapy is indicated in the treatment of cancer.
Taking medications is allowed only if prescribed by a doctor, specifying the dosage and duration of the course.
If mucus is a consequence of alcohol abuse, smoking or food, you will have to stop eating them. This means the need to reconsider our lifestyle and take a responsible attitude towards health.
Why does mucus appear?
The causes of mucus in the stool of an adult can be different. If mucus is released during bowel movements, this may be a natural reaction of the body to the aggressive influence of the external environment. But much more often, poop with mucus is a sign of malaise.
Mucus in feces as a physiological reaction of the body
There is little physiological mucus in excrement, so it is very difficult to notice visually. Stool with mucus is considered a normal reaction of the body if it is of medium density and shaped into a long sausage. Physiological mucus in poop, if a person is healthy, does not manifest itself in any way. Usually the patient has a lot of mucus in the stool in the following cases:
- when eating food containing starch, products made from cottage cheese, as well as bananas, watermelons, potatoes;
- after antibiotics (their use has a detrimental effect on digestion);
- with an unbalanced diet (frequent fasting or overeating);
- in case of non-compliance with personal hygiene rules.
Stool in the form of mucus in an adult also occurs in the presence of bad habits (smoking, alcohol abuse).
Nonspecific ulcerative colitis
Nonspecific ulcerative colitis (UC) is an autoimmune inflammation of the colon, which is quite difficult to treat. The inflammatory process provokes the formation of ulcers and erosions on the mucous membrane, which leads to the appearance of blood in the stool. Along with the blood, mucus and pus are found, and the stool has an extremely foul odor.
It is interesting: if in other pathologies blood in the stool is detected only in advanced stages, then ulcerative colitis can manifest itself from this manifestation. Also, blood and mucus can be released from the anus outside the act of defecation.
Other symptoms
In addition to changes in the nature of stool in nonspecific ulcerative colitis, the following symptoms occur:
- Diarrhea up to 20 times a day;
- Pain syndrome of varying intensity;
- Increase in body temperature to subfebrile levels;
- Loss of appetite, exhaustion;
- Flatulence.
A reliable cause of ulcerative colitis has not been established, but autoimmune inflammation and genetic predisposition play a major role. And stress and dietary errors worsen the patient’s condition.
Among the specific diagnostic methods to detect this pathology, stool analysis and endoscopic examination with biopsy are used.
Prevention
Prevention of large amounts of mucus in the stool is to minimize the risk of developing intestinal pathologies. The main rule is adherence to the principles of rational nutrition. What does it mean? Meals should be small and regular. You should follow a diet, take only biologically complete food.
It is very important to strengthen the body. High immunity is a reliable barrier to any intestinal infections. Playing sports, walking in the fresh air, positive emotions, and giving up bad habits will help.
In addition, regular prevention of helminthiasis should be carried out, and the established periods for medical examinations and preventive examinations should not be missed. If there is mucus in the stool, it is important to identify and treat the disease at an early stage in order to prevent the appearance of severe, painful symptoms.
Sometimes situations occur when mucus appears in the stool of an adult. This phenomenon causes fear for health. What could this phenomenon mean? The presence of mucus in the human intestines must be mandatory. It ensures the proper functioning of the organ. But there are cases when mucous clots in the stool will mean a disruption in the functioning of the digestive organs.
Diverticulosis
For what other reasons can mucus and blood appear in an adult? Adult patients may notice streaks of blood if diverticulosis develops. This is the name given to a disease that causes food debris or feces to become stuck in the walls of the esophagus. These protrusions are usually called diverticula. If the mass stagnates for a long time, then fermentation begins, as well as suppuration, and finally, perforation of the walls.
Complications of diverticulosis are chronic constipation, increased body temperature, as well as severe pain that is localized in the abdominal area.
Parents' actions
Having noticed unusual inclusions in the feces of their child, the first thing parents should do is to carefully look at his behavior: is he sleeping well, is he crying for no reason, is he behaving as usual or has something changed, has he lost his appetite... If everything is normal, and more mucus appeared, but there was no diarrhea, vomiting, or fever, you could exhale. Most likely, there was some kind of temporary glitch ⏱️.
In the same case, when there are accompanying symptoms and the stool contains characteristic impurities, you should not hesitate to visit a doctor. Without a diagnosis, there is no point in carrying out any treatment.
Consultation with a pediatrician, gastroenterologist (possibly a nutritionist, proctologist) and a high-quality examination are necessary.
Which doctor should I see and what tests should I take?
After the therapist or gastroenterologist has conducted an initial examination of the patient’s health, performed palpation of the abdomen, and entered the complaints heard into the patient’s medical record, he decides to prescribe the following types of tests and undergo the following diagnostic procedures:
- clinical blood test (checking the sugar level, the ratio of the main cells actively involved in metabolic processes);
- morning urine, which is taken on an empty stomach and shows the possible presence of an inflammatory process in the body;
- Ultrasound of organs located in the abdominal cavity (a specialist studies the condition of the tissues of the pancreas, liver, gall bladder, intestines, stomach, duodenum);
- stool samples are submitted for bacterial inoculation of their composition;
- smears are taken from the walls of the anus to analyze for the possible presence of helminth eggs, which also quite often form mucus in the stool;
- intestinal endoscopy (a special probe is inserted into the anus, which is advanced into the cavity of this digestive organ, where its cavity is examined to detect possible pathologies).
Depending on the presence of concomitant symptoms characteristic of this gastrointestinal disorder, the attending physician, at his discretion, may prescribe other types of tests, as well as diagnostic measures.
Diet
In order to ease the work of the intestines and eliminate mucous secretions, you should change your diet for a short period to a more gentle diet. For this purpose, a table 4 diet is prescribed, which is used for acute and chronic intestinal diseases.
During the diet, exclude from the diet most foods containing fat and carbohydrates, as well as foods that cause fermentation processes in the intestines:
- fatty meats, fish, sausages, canned meat and fish, etc.;
- fatty, fried, salty and spicy;
- whole milk and fatty fermented milk products;
- all types of fresh bread;
- foods high in sugar;
- raw vegetables and fruits high in fiber, which lead to bloating (white cabbage, apples);
- alcoholic and carbonated drinks, kvass and fruit juices that can increase gas formation.
In order to normalize digestion when mucus appears for a long time, it is necessary to eat only heat-treated food in small portions 4 times a day and drink 1.5 liters of water per day. The following categories of dishes can be included in the diet:
- boiled lean fish and meat (in the form of meat puree, meatballs, steamed cutlets);
- vegetable broths, as well as vegetables pureed;
- liquid porridge from rice, oatmeal, buckwheat;
- jelly from berries and fruits;
- low-fat cottage cheese and curd soufflé.
Mucus in the stool is not always a symptom indicating the presence of a pathological process in the body. A small amount of it is always observed in feces.
This is a consequence of the presence of dead epithelial cells in the body, resembling light or transparent jelly-like discharge, which are removed from the intestines during bowel movements.
The presence of mucus contributes to the normal functioning of the intestines; its lack causes disruption of its patency and is accompanied by constipation.
Due to prolonged stool retention, toxic substances, which are waste products of pathogenic microorganisms, are not removed from the gastrointestinal tract and enter the blood. In addition, the delicate intestinal mucosa is exposed to the destructive effects of toxic components.
The appearance of a large number of such secretions in the feces indicates serious problems associated with disruption of the gastrointestinal tract.
Reasons for exceeding the permissible amount of mucus
Factors that can provoke active mucus secretion are quite diverse.
Among the most common are: 
- prolonged fasting;
- sudden change in food products;
- drinking raw drinking water from random sources;
- colds and infectious diseases of the respiratory tract, accompanied by copious sputum production;
- dietary nutrition, which involves daily consumption of decoctions of oats and flax seeds;
- uncontrolled use of medications;
- irritable bowel syndrome, which causes digestive problems accompanied by constipation, diarrhea, bloating, and increased gas production;
- hypothermia, which causes inflammation of the pelvic organs and anal area.
Paying attention to your health helps eliminate or prevent negative manifestations.
Diseases that cause mucus secretion
The appearance of impurities in the stool of an adult is in most cases associated with various diseases of the digestive system. Depending on the nature of the pathology, different types of mucous discharge appear.
Among the most common diseases it should be noted:
- Intestinal infections of a bacterial or viral nature. These are dysentery, colitis, enteritis, typhoid fever. These pathologies are a fundamental factor predisposing to an extremely active process of mucus secretion in the feces. This occurs due to increased secretion of glands and the removal of dead pathogenic bacteria, viruses and leukocytes from the body during the act of defecation. In addition to mucous discharge, symptoms such as intense abdominal pain, diarrhea, high fever and weakness are observed.

 Lack of normal intestinal microflora - dysbiosis causes digestive disorders, resulting in the appearance of jelly-like clots and undigested food fragments in the stool. Factors such as alcohol abuse, smoking, stress, poor diet, as well as antibiotics and hormonal drugs taken without a doctor’s prescription act as a trigger for dysbiosis. The most noticeable symptoms, besides excessive mucus secretion, are frequent migraines, susceptibility to respiratory diseases and the likelihood of skin rashes.
Lack of normal intestinal microflora - dysbiosis causes digestive disorders, resulting in the appearance of jelly-like clots and undigested food fragments in the stool. Factors such as alcohol abuse, smoking, stress, poor diet, as well as antibiotics and hormonal drugs taken without a doctor’s prescription act as a trigger for dysbiosis. The most noticeable symptoms, besides excessive mucus secretion, are frequent migraines, susceptibility to respiratory diseases and the likelihood of skin rashes.- Worm infestation. If there are worms in the intestines, mucus may also contain blood impurities. The patient has no appetite, stomach pain often occurs, digestion is upset, and anemia develops.
- Pathologies of the respiratory organs. Clots of mucus in feces during bowel movements are observed during respiratory diseases. Their shade varies from white and yellowish to brown. Mucus, produced in excess quantities during illness, enters the stomach, so its streaks are a common occurrence during viral infections, influenza, and acute respiratory viral infections. It should be noted that in this case there are no signs of dyspepsia, and the appearance of mucus stops on its own as you recover.

 Polyps and hemorrhoids. Such formations on the intestinal walls provoke the occurrence of long-term constipation, accompanied by intense painful sensations in the anal passage during the passage of feces. The inflammation characteristic of this disease leads to the formation of mucus, which is released along with the feces.
Polyps and hemorrhoids. Such formations on the intestinal walls provoke the occurrence of long-term constipation, accompanied by intense painful sensations in the anal passage during the passage of feces. The inflammation characteristic of this disease leads to the formation of mucus, which is released along with the feces.- Oncology. Tumor processes localized in the stomach or intestines lead to the death of epithelial cells. This is accompanied by the release of thick mucus. An expressive sign of a serious illness is sudden weight loss and chronic fatigue.
It is difficult to independently determine the cause of such discharge. Moreover, it is not recommended to diagnose yourself and try to independently eliminate the symptoms, which sometimes indicate the likelihood of a life-threatening disease.
Other reasons
In some cases, the appearance of stool mixed with mucus in adult patients is caused by reasons that are not as serious as diseases that pose a threat to health.
Such phenomena occur:
- when consuming large amounts of cottage cheese, bananas, watermelons, oatmeal and rice porridge;
- due to starvation diets or during the absorption of large quantities of vegetables and fruits;
- due to a lack of protein in the diet.
The mucous membrane is exposed to the irritating effects of coarse fibers, which, due to improper nutrition, leads to its depletion and, as a result, disruption of digestive processes and an increase in secretions.
Causes of mucus in pregnant women
An important factor that can lead to excess mucus production is pregnancy.. The opinion of experts is that this is not a cause for concern if there are impurities of clear mucus in the stool after defecation.
Such manifestations do not pose a danger to the health of the expectant mother and fetus. They indicate the presence of food incompatibility or dysfunction of the digestive glands.
Types of discharge
A small amount of mucus does not cause alarm, as this is a normal protective function of the body that helps protect the walls of the esophagus from various damages.
However, the nature of the discharge, a significant increase in its quantity and a difference in color are characteristic symptoms of special conditions and various diseases: 
- White mucus, yellow, green or brown impurities in the stool appear in adults due to food allergies or lactose intolerance. Such discharge appears with dysbacteriosis, accompanied by poor absorption of food. This indicates a lack of liquid medium that facilitates the movement of feces.
- A large amount of clear mucus is evidence of cystic fibrosis, which develops against the background of increased mucus production by the glands. This condition indicates an inflammatory process in the respiratory tract or intestines. Food allergies are also accompanied by the discharge of clear clots.
- Painful bowel movements and orange mucus without fever indicate the possibility of ulcerative colitis.
- With well-formed stool, scarlet or pink mucus with blood is detected - this is a sign of hemorrhoids.
- Signs of dyspepsia (foamy, loose stools, vomiting, fever) with clear mucus indicate an E. coli infection.
- Mucus streaked with blood indicates the possibility of ulcerative colitis or dysentery.
- Foul-smelling stool with yellow mucus is a dangerous symptom of a ruptured abscess or decomposition of a cancerous formation.
- Mucus and pus in the stool are an alarming indicator. It indicates the presence of serious inflammation, proctitis, granulomatous colitis, rectal cancer or villous tumor.
The list of conditions is quite diverse.
In addition to the cases described, you should also pay attention to the fact that:
- Frequent urge to have a bowel movement due to stress, accompanied by pain in the abdomen and the release of clear or yellow mucus - irritable bowel syndrome.
- The appearance of a large amount of mucus in the stool indicates the body’s reaction to the presence of toxins that contribute to the development of allergies.
- Autoimmune diseases also contribute to the production of excess mucus.
- Transparent mucus is observed after treatment with antibiotics or hormonal agents.
- White or pink mucus is often seen with constipation.
Feces with mucus should be recognized as a serious diagnostic indicator, which requires consultation with a doctor.
Diagnostics
It is possible to differentiate diseases accompanied by the presence of mucous discharge in the stool using the following diagnostic measures: 
- stool coprograms;
- bacterial culture to determine the causative agent of infection;
- macro and microscopy of feces;
- colonoscopy;
- radiography;
A general clinical and detailed biochemical blood test is required.
Treatment
The severity of symptoms requires immediate consultation with an experienced specialist.
Which doctor should I contact?
The first visit is to a family doctor or therapist.
He will refer you to specialized specialists:
- gastroenterologist;
- proctologist;
- infectious disease specialist;
- endocrinologist.
Drug therapy
The use of medications is prescribed taking into account the diseases that caused the discharge: 
- Interferon and Arbidol are recommended for intestinal inflammation or diseases of viral origin.
- Ersefuril and Furazolidone have proven themselves in the treatment of intestinal infections.
- Viferon and Regidron are indispensable drugs in the treatment of intestines caused by a viral pathogen.
- Tinidazole and Piperazine are used for helminthic infestations.
- Antifungal suppositories and Amphotericin are prescribed for fungal intestinal diseases.
- Linex, No-shpa and Furazolidone are effective drugs that are used to treat colitis, dysbacteriosis and inflammation of the rectum.
- The use of chemical and radiation therapy is indicated in the treatment of cancer.
If mucus is a consequence of alcohol abuse, smoking or food, you will have to stop eating them. This means the need to reconsider our lifestyle and take a responsible attitude towards health.
Nutrition adjustments
An effective measure to eliminate negative manifestations is to follow a gentle diet.
It assumes: 
- excluding spicy, fried and fatty foods from the menu;
- refusal of marinades, pickles, sausages;
- Alcoholic drinks, black coffee, and spices that stimulate the production of gastric juice are prohibited.
The prognosis for the treatment of diseases accompanied by the appearance of mucus in the stool is favorable in most cases.
Lack of timely treatment can lead to complications such as peptic ulcers, internal bleeding, and oncological processes.
It is possible to prevent their development provided that the recommendations of qualified specialists are followed. Self-medication leads to a protracted course of the disease and is fraught with dangerous consequences for health and life.
The stool of a healthy person usually does not contain noticeable particles of mucus. In this case, white mucus in the feces, impurities of a different color and consistency are formed in small quantities due to the activity of the intestinal glands. With the help of mucus in feces, the process of removing digestive waste from the human body is simplified.
When mucous discharge is normal
The passage of feces with mucus in an adult is a physiological process. The mucous substance envelops the intestinal walls, thereby protecting them from the irritating effects of various substances. That is, treatment is not always necessary, because in a number of different situations a certain amount of mucus in the stool is quite normal. If there is no mucous discharge in the stool, a person may experience constipation and certain difficulties during bowel movements.
The release of feces with mucus in an adult can play an important role. Normally, it is a jelly-like substance of light or transparent color, the basis of which is made up of epithelial and leukocyte cells.
If there is a lot of mucus in the stool and it is visible, there is no need to panic. Noticeable mucus coming out of the anus is considered normal in certain situations. There are a number of cases when mucus in an adult should be perceived not as a pathology, but as a natural state:
- During a cold and runny nose, a large amount of mucus, that is, sputum, penetrates the esophagus and then into the intestines.
- After taking a large amount of certain foods from our usual diet. The main nutritional reasons are the consumption of oatmeal, bananas, cottage cheese, and watermelons. The presence of a mucous substance in the stool speaks specifically about dietary habits.
- Mucus in stool during pregnancy simultaneously covers dietary habits and some dysfunctions of the body. However, if a woman has very noticeable mucus in her stool while carrying a child, it is better to consult a doctor about this. After childbirth, women have watery and mucous stools that are also not uncommon.
Pathological causes
 As a rule, the appearance of stool with white mucus or a copious amount of a jelly-like substance with a yellowish tint, green or white impurities, indicates the presence of intestinal problems. This mainly concerns the distal sections, that is, we are talking about the large intestine.
As a rule, the appearance of stool with white mucus or a copious amount of a jelly-like substance with a yellowish tint, green or white impurities, indicates the presence of intestinal problems. This mainly concerns the distal sections, that is, we are talking about the large intestine.
In adults with hemorrhoids, dysbacteriosis, and other disorders, the intestinal glands actively produce excess mucus in order to neutralize certain negative factors.
What does mucus in the intestines mean? In adults, this may mean that the body turns on a special protective function when the intestinal walls are irritated by harmful substances or dangerous microbes. The mucus on the surface of the walls protects them, envelops them and acts as a lubricant.
The detection of this in an adult indicates that inflammatory processes are occurring in his intestines. But before you get rid of a pathological substance in excess, you need to understand why it appears and in the form of what impurities.
Depending on where the inflammatory process may be present, excrement appears along with a different type of substance:
- Impurities in the form of threads, jelly-like film or large flakes. These white-gray mucous masses may appear on the surface of stool. The presence of a long film or a kind of thread indicates that the distal part of the intestine is affected. In parallel with this, in addition to tape-like mucous inclusions, hard stool is observed. It is difficult to pass or is accompanied by prolonged constipation.
- Small flakes mixed with feces. Thick feces of a dense structure are mixed with mucous inclusions, that is, the presence of clots occurs inside and outside. This means that the higher parts of the large intestine are affected, and in some cases this situation is a prerequisite for damage to the small intestine. Then the jelly-like substance will be yellow.
Diseases with mucous stool
 If there is copious amounts of mucus in the stool, or even if there is only a little of it, it is better to immediately contact a specialist. You should not take Linex or Enterofuril on your own before consulting with your doctor. First, a specialist must conduct an examination, study a stool analysis and make an appropriate conclusion. Almost everything that can help determine the development of diseases in the early stages is indicated.
If there is copious amounts of mucus in the stool, or even if there is only a little of it, it is better to immediately contact a specialist. You should not take Linex or Enterofuril on your own before consulting with your doctor. First, a specialist must conduct an examination, study a stool analysis and make an appropriate conclusion. Almost everything that can help determine the development of diseases in the early stages is indicated.
A thorough examination of stool allows you to find and prevent all kinds of diseases. Such simple studies as analysis of stool, urine and blood are the basis for understanding the current state of health of each person. If you have hemorrhoids, constipation, other diseases, discomfort, when you are haunted by constant rumbling in your stomach, consult a doctor for a routine preventive check. The appearance of mucus in the stool is a reason to consult a specialist.
Frequent bowel movements, a lot of mucus, itching in the anus, and stool with an unpleasant odor that is not typical for your body may indicate potential problems.
There are several diseases that can cause loose stools with mucus, for example:
- For hemorrhoids or internal polyps. With the help of mucus that our body produces, a protective shell is created. But the secretion of mucous substance in humans during hemorrhoids is different, since the jelly-like threads have their own characteristics. They do not mix with feces, and after defecation they can come out on their own without feces and remain on the used paper.
- Mucous colitis. It is also called membranous. It is a functional dangerous lesion of the human intestine. In this case, the mucous component is represented by threads or dense films. This makes them look a bit like tapeworms. You should not confuse them, but it is better to seek help from doctors.
- Absorption problems. The reasons for the appearance of mucus are that the body cannot absorb certain foods. This is due to the patient's food intolerance or food allergy. That is, a person is not able to consume even a small amount of certain foods. These diseases include celiac disease, lactose intolerance and malabsorption syndrome.
- Dysbacteriosis. Sticky mucus and even green feces with mucus can be caused by dysbacteriosis. In this case, the normal beneficial intestinal microflora is disrupted, and nutrients are not absorbed. Poisoning, vomiting, flatulence and other unpleasant symptoms may also appear. A person is bothered by frequent bowel movements; mucus comes out in large quantities, since it is produced to remove various toxins and harmful wastes. However, with dysbiosis in the human body, pathogenic microflora is activated, which leads to inflammatory processes. In this case, it is imperative to get rid of the mucus. Dysbacteriosis can develop against the background of other diseases, after taking antibiotics or some other provoking factor. This requires consultation with a doctor to make an accurate diagnosis. Under no circumstances should folk remedies be used without the consent of a specialist.
- Irritable bowel syndrome (IBS). The disease does not look the best, since a person is often bothered by diarrhea; a jelly-like mass comes out of the anus along with feces. Soft stools progress to diarrhea with mucus in an adult.
- Intestinal infectious lesions. Green stool with mucus, dark stool with a black mucous admixture may appear against the background of infections affecting the intestines. Purulent discharge indicates serious neglect of the disease, so you should definitely seek help. A high temperature, mushy stool and mucus in the stool with an unpleasant odor indicate a potential infection. Mucous pus is very dangerous as a sign of illness. Treatment at home may not be effective and you will be sent to a hospital. It all depends on the doctor’s decision and the results of the analysis.
- Diverticulitis. This is an inflammation and hernial formation on the intestinal wall. In addition to the impurities in the feces themselves, diarrhea is a symptom of this disease. Plus, there is profuse gas formation and pain in the left lower abdomen.
- Cystic fibrosis. This is a congenital disease of a genetic nature, characterized by damage to the organs responsible for the secretion of mucus. It most often occurs in children, but can also occur in adult patients.
- Tumors. The mushy stool is supplemented with blood in the form of streaks, there is pain in the lower abdomen, and general weakness is observed. The first signs should be an immediate reason to consult a doctor.
Diagnosis of possible violations
 Also, discharge can provoke diseases such as gastritis, pancreatitis, rotavirus. Diseases are not always the culprits. For example, poisoning, side effects after suppositories, antibiotics can also increase the activity of the production of mucous masses and remove them along with feces.
Also, discharge can provoke diseases such as gastritis, pancreatitis, rotavirus. Diseases are not always the culprits. For example, poisoning, side effects after suppositories, antibiotics can also increase the activity of the production of mucous masses and remove them along with feces.
But if you notice green stools with mucus or pus in your stool, which usually produces brown mucus, immediately consult a doctor. Trying to cure or independently determine why mucus appears instead of feces is not recommended. There are several potential causes for the passage of mucous formations without feces - worms, constipation and intestinal obstruction. One way or another, each of the diseases or disorders that lead to such symptoms requires exclusively professional intervention.
Any discharge from the anus during defecation that is different from normal, such as foamy feces, blood clots, or an uncharacteristic color of stool, is a good reason to get tested and undergo a comprehensive examination. Feel free to take the coprogram at least once a year. For an adult, this is not just useful, but necessary. Good and correct bowel movements are a sign of excellent condition of the body.
Most people do not tend to carefully examine their own feces, and the design of modern plumbing often interferes with such research. If various kinds of impurities and inclusions are accidentally discovered in excrement, then it makes sense to be wary: some of them may be the first clinical manifestations of pathologies. Certain impurities are a good reason for visiting a doctor and further undergoing a medical examination, which necessarily includes testing.
Normal composition, color and consistency of stool
A healthy adult produces an average of 300 g of excrement per day, and defecation usually occurs once a day.
Note:Normally, stool has an almost uniform consistency.
The main components of excrement are:

In the absence of acute and chronic diseases, as well as intestinal disorders, the color of an adult's stool varies from light brown to dark brown.
A change in color is one of the signs of the development of pathology. A greenish tint is one of the symptoms of regional enteritis (Crohn's disease), gray color indicates problems with the pancreas, light gray or almost white indicates a violation of the functional activity of the liver (in particular, with Botkin's disease). A yellow tint indicates gallbladder disease.

What are the types of impurities?
The following impurities are most often detected in stool:
- leftover food;
- slime;
- blood;
- foreign inclusions;
- pus.
The presence of impurities may indicate the development of diseases (sometimes quite serious pathologies of the digestive system), but it is often due to the nature of the diet.
Residues of food in stool
 If you find whole corn kernels or seeds (for example, sunflower seeds) in your feces, this is not a reason to sound the alarm. Some foods are very difficult to digest, especially if they are poorly chewed. Also, digestive enzymes are completely unable to cope with the veins present in meat products, as well as fish bones and fragments of eggshells.
If you find whole corn kernels or seeds (for example, sunflower seeds) in your feces, this is not a reason to sound the alarm. Some foods are very difficult to digest, especially if they are poorly chewed. Also, digestive enzymes are completely unable to cope with the veins present in meat products, as well as fish bones and fragments of eggshells.
The reason for a visit to the doctor is the presence of undigested meat fibers, as well as cottage cheese or eggs, in the excrement. This sign indicates a lack of digestive enzymes.
Note:the presence of large particles of undigested food is called lientorrhea. When meat fibers are detected, they speak of creatorrhoea.
The reason for the lack of enzymes may be:
- insufficient secretion of pancreatic juice (after resection of part of the pancreas or against the background of pancreatitis);
- inhibition of enzyme secretion in the intestine;
- pronounced atrophy of the gastric mucosa.
Residues of food may appear in the stool during its accelerated evacuation against the background of increased peristalsis. In this case, some foods simply do not have time to be digested and absorbed. This phenomenon is particularly characteristic of irritable bowel syndrome.
If the stool has an oily sheen, this is a sign of steatorrhea, i.e. the presence of a large amount of lipid compounds (fats).
Possible causes of steatorrhea:
- a large amount of fat in the diet;
- diseases of the liver, gall bladder and ducts (cirrhosis, hepatitis, cholecystitis, etc.);
- pancreatic diseases (inflammation, strictures, ulcers and tumors);
- hemochromatosis (accumulation of iron in organs due to metabolic disorders);
- intestinal pathologies (inflammatory, autoimmune and tumor);
- endocrine diseases and pathologies of the endocrine glands;
- congenital (hereditary) diseases;
- systemic manifestations of skin diseases;
- Excessive consumption of laxatives.
Mucus in stool
 Note:the presence of some mucus in the stool (in the form of lumps or inclusions) is normal for young children who are breastfed. Mother's milk is characterized by high fat content, which the baby's digestive enzymes are not yet able to fully cope with.
Note:the presence of some mucus in the stool (in the form of lumps or inclusions) is normal for young children who are breastfed. Mother's milk is characterized by high fat content, which the baby's digestive enzymes are not yet able to fully cope with.
In any healthy person, the cells of the intestinal wall produce mucus, which is necessary to facilitate the passage of feces through the lower parts of the digestive tract. A small amount of colorless (almost transparent) mucus is often normal and is not a cause for concern.
If mucus is released in large volumes or is brown or yellowish in color, this may indicate the following pathologies:
- increased intestinal motility;
- inflammatory diseases of non-infectious origin;
- acute intestinal infections (dysentery, typhoid fever, etc.);
- benign or malignant formations;
Note:often a large amount of mucus is the first clinical sign of the development of regional enteritis (). The admixture of a significant amount of mucus is also quite often recorded in chronic constipation.
Based on the degree of distribution of the mucous component in feces, the height of the location of the pathological focus can be determined. If mucus relatively evenly permeates the excrement, then the inflammatory process is localized in the upper sections of the intestine, but if impurities are detected on the surface (usually in the form of lumps), then the lower sections are affected.
Bloody feces
The presence of blood in excrement is an absolute reason to consult a doctor, since it can be a clinical manifestation of the following diseases:
- autoimmune intestinal pathologies ();
- malignant neoplasms of the gastrointestinal tract;
- benign tumors of the intestinal walls ();
- ischemic colitis;
- diseases of infectious origin (dysentery, etc.);
- and ulcers of the rectum and rectal area;
- intestinal angiodysplasia;
- blood pathologies (clotting disorders);
- some helminthic infestations (in particular, ascariasis).
Blood volume varies depending on the nature of the disease and the severity of the pathology. Feces often contain only small and inconspicuous streaks, but in case of serious pathologies, up to 200 ml or more can be released during defecation. In this case, we are talking about intestinal bleeding, which requires immediate action.
 Note:in some pathologies, during the act of defecation, only blood mixed with intestinal mucus is released.
Note:in some pathologies, during the act of defecation, only blood mixed with intestinal mucus is released.
The color of blood in the stool makes it possible to determine with a high degree of probability the approximate location of the bleeding site. The scarlet color and location of the blood on top of the feces indicates that there is a pathology of the sigmoid, descending or rectum. Fresh blood is also released from anal fissures and hemorrhoids. Darker blood and blood clots mixed relatively evenly with the stool indicate that the source of the bleeding is in the upper part of the large intestine (colon) or small intestine. Black coloring of the stool may indicate that blood is being secreted in the stomach or esophagus (the specific color is due to the fact that the blood has been exposed to hydrochloric acid of the gastric juice).
Note:a reddish tint to the stool or burgundy streaks are not always due to the presence of blood - be sure to remember if you ate beets the day before?
Foreign inclusions
The presence of films in feces may be due to a rather serious pathology of the large intestine - pseudomembranous colitis, often caused by long-term or irrational antibiotic therapy.
Fragments of necrotic tissue are found during the disintegration of malignant tumors, as well as during intussusception against the background of intestinal obstruction.
When taking pharmacological drugs in granular forms, their particles are also often detected in the stool. Activated carbon gives excrement a black color.
The so-called feces are sometimes detected. pancreatic, biliary and intestinal stone formations - coprolites. Intestinal compactions (stones) are not true stones, but are highly compacted feces formed due to chronic constipation. This pathology is more typical for elderly patients. True coprolites consist of an organic core with gradually growing mineral salts. The presence of such stones in the stool suggests diseases of the pancreas or bile ducts.
Pus in stool
The presence of pus in feces is unconditional evidence of the development of a pathology of inflammatory origin. In most cases, pus is detected in parallel with blood and mucus.
Pus may have a yellowish or greenish tint and appears in the following diseases:
- proctitis;
- infectious colitis;
- ulcerative colitis;
- decay (in the later stages of cancer);
- breakthrough of an abscess into the intestinal lumen;
- autoimmune intestinal damage (Crohn's disease).
Important:remember that if pus is released during defecation, then self-medication is strictly unacceptable. There can be no talk of a positive effect in this case.
Treatment
The detection of most of the mentioned impurities is the basis for contacting a gastroenterologist at the clinic. The local physician can also refer the patient to a specialized specialist and prescribe a series of tests.
Specialists whose consultation may be needed:
- proctologist;
- infectious disease specialist;
- surgeon;
- hematologist;
- oncologist.
Important:If a large amount of blood is released against the background of a deterioration in the general condition, an ambulance should be called. Massive bleeding is a life-threatening condition and requires hospitalization of the patient in the intensive care unit or intensive care unit.
To establish or clarify the diagnosis, in most cases the patient is referred for examination to an endoscopist.
Plisov Vladimir, medical observer
Article prepared by:
In an adult, mucus in the stool is not always a sign of normality. As a rule, many people ignore such a symptom, bringing the current disorder to an advanced form. It is important to pay attention to accompanying signs. In some cases, mucus in an adult's stool may require immediate diagnosis and further treatment. Timely consultation with a doctor helps to avoid a number of complications. The patient should pay attention to the color of the discharge. This is necessary to establish a preliminary diagnosis and prescribe the required studies.
 If mucus impurities appear in the stool, you must consult a doctor and undergo the necessary examinations.
If mucus impurities appear in the stool, you must consult a doctor and undergo the necessary examinations. In this article you will learn:
Factors contributing to the appearance of the symptom
Doctors identify the following causes of mucus in the stool in adults:
- irritable bowel syndrome;
- the presence of neoplasms in the intestinal tract;
- individual intolerance to something by the body;
- infectious diseases of the intestinal tract;
- helminthiases;
- viral infections;
 Colitis and other intestinal diseases can cause mucus in the stool
Colitis and other intestinal diseases can cause mucus in the stool - hemorrhoids accompanied by cracks in the anus;
- stomach ulcers;
- pancreatitis;
- inflammatory process in the colon;
- colitis;
- proctitis
The presence of a disorder can be determined by the color of the mucus observed in the stool of an adult patient. Treatment can begin only after a comprehensive diagnosis.
Causes of white mucus
White mucus in stool usually indicates the presence of diseases of the digestive organ and intestinal tract. The most common root causes include:
- inflammatory process in the rectum;
- the body’s natural reaction to the presence of pathogenic microorganisms;
- increased number of fungi;
- dysbiosis.
With these disorders, as a rule, the mucous membrane of the intestinal tract is affected. In addition, the natural microflora of the body changes for the worse.
The reasons for the appearance of white mucus in stool are described in detail in the video:
Causes of mucus without feces in an adult
Mucus without feces indicates that the adult is unable to retain the contents of the intestines. In this case, the patient complains of sharp pain in the lower abdominal cavity. The patient's body temperature increases. The condition can be caused by:
- prolonged absence of bowel movements;
- helminthiasis;
- ulcerative lesions of the digestive organ;
- the presence of neoplasms in the gastrointestinal tract;
- foreign object in the gastrointestinal tract.
Long-term constipation can cause mucus to come out of the anus.
Bloody mucus
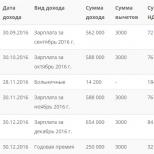
Red mucus in the stool is the most dangerous sign. It is important to pay attention to the characteristic features of the selection. The main ones are described in the table.
If there is bloody mucous in the stool of an adult, you should immediately consult a doctor. To hesitate with such a sign is dangerous to health and life. Sometimes the symptom indicates an advanced stage of liver cirrhosis.
Yellowish spots in stool
Yellow mucus usually indicates the presence of polyps. This symptom is also observed with inflammation of hemorrhoids. Often a deviation indicates:
- inflammatory process in the intestines of a bacterial type;
- impaired absorption of products;
- recently completed a course of antibacterial therapy;
- hypothermia of the genital area;
- infectious diseases of the intestinal tract;
- the presence of malignant neoplasms.
Yellow mucus may appear in the stool due to hypothermia of the genitals
Brown mucous patches in the stool of an adult
In most cases, brown mucus usually indicates that the pancreas is not functioning properly. Liquid consistency of feces may indicate dysbacteriosis.
Doctors say that the symptom in some cases may be normal. The sign occurs when:
- allergic reaction;
- rhinitis;
- flu;
- polyp.
A malfunction of the pancreas can cause brown mucus to appear in the stool.
Symptom as a sign of normality
Mucus in an adult’s stool does not always require treatment. The symptom is common among patients. The sign is normal for colds, which are accompanied by discharge from the nasal cavity.
Mucus in the stool during a cold indicates that fluid from the upper respiratory tract is draining along the surface of the back wall. Some of it enters the esophagus and intestines. After this, the mixture is excreted naturally. In this case, only the underlying root cause needs to be treated.
If you eat bananas in excess, a person may experience mucous patches in their stool.
Sometimes mucus in stool can be a result of eating certain foods. These include:
- cottage cheese;
- oatmeal;
- bananas;
- watermelon.
Typically, the symptom occurs when one of the listed foods is present in the diet in excessive quantities. When mucus is normal, there are no additional symptoms, and the patient’s condition is satisfactory.
The symptom is also often present in people who lead an unhealthy lifestyle. Smoking and alcohol abuse can provoke the appearance of mucus. The symptom may also appear during treatment with certain medications.
Diagnostic methods
The patient cannot do without a comprehensive diagnosis. This is the only thing that will help establish a final diagnosis and select effective treatment. First of all, the doctor finds out the patient’s diet and its quality. The doctor performs an external examination of the patient. If necessary, palpation is performed. It is important that the sick person reports all associated symptoms.
It is required to submit stool for examination. This is necessary to find pathogenic microflora. The doctor determines the causative agent of the disorder. Mucus inclusions are also studied in the laboratory.
A blood test can determine an increased level of white blood cells. In this case, the presence of an inflammatory process should be assumed.
An occult blood test is not always required. This is necessary when there are mucous red streaks in the stool. Sometimes the sign indicates internal bleeding. The patient may also be given a referral to:
- endoscopy;
- rectoscopy.
Treatment in stool mucus
Treatment for the disorder in adults depends on the underlying cause. Typically, therapy is complex and includes:
- diet;
- drinking large amounts of liquid;
- taking medications.
Normalization of diet is one of the measures to treat the disorder
If a disorder occurs due to individual intolerance, it is necessary to exclude the allergen. Usually this is enough. It is important to stick to a daily routine. For worms, anthelmintic therapy is indicated. Typically, medications are taken for 1 to 10 days. Antiviral treatment is indicated for viral infections.
In case of pancreatitis, the patient is prescribed medications to normalize the functioning of the pancreas. For malignant neoplasms, chemotherapy and surgery are recommended.
If the symptom is associated with food intake or bad habits, then no special treatment is required. It is enough to get rid of the provoking factor. Therapy for any disorder can only be selected by a highly qualified doctor.
The patient must follow the correct daily routine
Nutritional Features
Diet is the basis of successful treatment. Food should be consumed in small portions. It is advisable to eat food at the same time. First of all, you need to exclude:
- alcohol;
- fatty foods;
- fried food;
- soda;
- confectionery;
- spicy;
- spicy;
- pickled;
- canned.
Food should have a comfortable temperature - about 40 degrees. Portions should be small. Food should be consumed 5-6 times a day.
You need to drink enough liquid per day. This is especially important if the feces have a liquid consistency. It is advisable to first grind the food to a mushy consistency. Allowed to add to the diet:
- steam cutlets;
- boiled or steamed lean meats and fish;
- dried fruit compotes;
- herbal teas;
- decoctions and tinctures;
- porridge;
- low-fat broths;
- dairy products.
If violated, all fried foods must be excluded from the menu.
Diet, as well as treatment, is selected on an individual basis. Nutritional characteristics are directly related to the final diagnosis.