During the next patronage visit. The Grand Canyon and night bingo in Vegas. Pediatrics with childhood infections
During our next visit to the casino, Lena decisively announced that tomorrow morning, and early in the morning, she was taking us to see the Grand Canyon. The degree of my ignorance, or rather darkness, was so great that I, frankly, did not know what kind of place this was and how famous it was. However, I was calmed down by the late hour and the beer I drank, which meant that it was unlikely that anyone would get up early in the morning.
However, alas, I underestimated Lena's energy. We left at dawn.
The trip from Las Vegas to the Grand Canyon took about six hours. All this time my husband slept in the back seat. Men are weak, their civilization is moving towards collapse and will be replaced by a new one - a perfect civilization of women. This has been clear to me for a long time. Harry decided not to go. Firstly, he saw the Grand Canyon twenty times, and secondly, being a responsible and hardworking person, he decided to spend the day when there were no guests in the house on business.
To be honest, I really wanted to sleep. Early morning is the most pleasant time for deep, restful sleep. But my task was to chat and not let Lena fall asleep. It was assumed that on the way back my husband would get behind the wheel, which is why they didn’t disturb him now.
The road lay deep into the continent. The air was dry, straw-yellow in color. Rows of plush scorched hills stretched out again, turning into mountains, surrounded on all sides by the dark trails of American roads.
There are so many pay phones, or rather call boxes for urgent free calls. Just too much. You can call the rescue service every 10 minutes! - I said, looking out the window.
- Yes, but it’s better not to get out of the car. You see, there are cougars roaming around here. “It may not be safe,” Lena said.
From the program “In the Animal World” I knew that pumas are red, bloodthirsty cats that calmly eat people. The road was no longer languid.
*** 
We approached the canyon from the old railroad. More precisely, the railway itself is fully functional, although it looks like an antique, and it really does take tourists to the attraction. The small wooden station from Western movies is also quite functional and, together with the railroad, which, by the way, also bears the name of the Grand Canyon, gives the necessary flavor to the place.
The boys who grew up on the "Mackenna Gold", and now have become big, good-natured guys, should begin to drag themselves away from the railway.
The view that soon opened up to us was truly great. In such places you understand: no matter what a person creates, no matter what miracles he comes up with, no matter how high his imagination soars, he cannot keep up with the Creator. The most impressive places when you see a cat  Some of them take your breath away in awe and there are not enough words to convey the impression, they were not created by human hands. I am not a religious person, I wore a red tie as a child, and some events in my short life so far led me to the seditious thought that there is no God. But, honestly, at the Grand Canyon I doubted my assumption. No, of course, according to the free booklets, everything was everyday: for several million years the Colorado River raged and rushed in crazy streams through an endless valley. Gradually, it subsided and turned into a barely noticeable ornate stream. At least it is very difficult to see in the depths of the canyon. She created this beauty.
Some of them take your breath away in awe and there are not enough words to convey the impression, they were not created by human hands. I am not a religious person, I wore a red tie as a child, and some events in my short life so far led me to the seditious thought that there is no God. But, honestly, at the Grand Canyon I doubted my assumption. No, of course, according to the free booklets, everything was everyday: for several million years the Colorado River raged and rushed in crazy streams through an endless valley. Gradually, it subsided and turned into a barely noticeable ornate stream. At least it is very difficult to see in the depths of the canyon. She created this beauty.
There is a horse and carriage tour along the bottom, but it costs something like $100 per person.
Those green dots in the photographs are trees twice the height of a man. It is impossible to photograph the canyon in length, just as it is impossible to photograph the entire horizon line.

In addition to the canyon itself, we were surprised by the hordes of squirrels, completely insolent from the amount of food and impunity. Proteins are not only fatty, but also very large. Each of them could well become a hearty dinner for a small family. At first, I used up half the film filming people squeezing constantly chewing squirrels, until I tried to touch the little animal myself. The squirrel did not run away and did not stop moving its jaws evenly. The squirrel was soft to the touch, like a toy.
In addition to the Grand Canyon itself and sites equipped for viewing the beauty of the landscape, there is a fairly expensive hotel, food establishments and a large number of gift shops near the canyon. As Lena said, there is an Indian reservation nearby. The Indians live by making cute handmade souvenirs, selling them and drinking fire water. They drink heavily. I have repeatedly heard the opinion in America that Indians are a rather closed community. ABOUT  they prefer to live in their world according to their own caste laws, and the authorities prefer not to interfere with them.
they prefer to live in their world according to their own caste laws, and the authorities prefer not to interfere with them.
I must admit that looking around Indian shops, and especially one, the largest one, with plush and maybe real heads of hunting trophies, unexpectedly proved to me that I like this style. I bought beads made from small multi-colored seeds (supposedly Indian women spat them out when eating exotic Indian fruits) and looked at a rag hip bag. A wonderful bag with a pattern characteristic of local folk art, the only thing I needed to be happy. This dream cost 30 dollars. I didn't have any money with me. My husband, seeing the price tag, flatly refused to give a gift, which I openly inform everyone about, as well as the fact that I will never forgive him for this fact.
We returned at sunset. Evening entertainment pleased with its consistency: exploring Las Vegas at night, a buffet, a casino. I wonder if this might get boring? Theoretically, yes, everything can get boring. In practice, I did not have time to verify this statement.
When we left the casino, full and satisfied with the loss, which can appropriately be called payment for a good time, Lena suddenly stopped.
“They play bingo in this casino,” she said. - I think that we should definitely buy tickets to the game.
As usual, I had no idea about the subject. The husband made a tired face, Harry admitted honestly. that he is not eager to waste the remaining money into the insatiable maw of the gambling house. In short, Lena and I were left, but this did not bother us, because she wanted to play, and I wanted further knowledge.
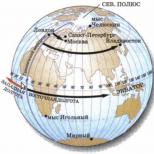
 So, as a result, I found out that a bingo game lasts almost three hours. The sacrament takes place in a separate room, in this case on a different floor. There are no vulgar machine guns screaming here and “one-armed bandits” are not going crazy with colored fountains of light - here there is a quiet stiffness, broken by the wooden gavel of the presenter. You can see what the hall looks like in the picture. This is not a photograph, since photography is also prohibited there, this is a picture from a booklet. In this case, it doesn’t matter, because we were in this very hall.
So, as a result, I found out that a bingo game lasts almost three hours. The sacrament takes place in a separate room, in this case on a different floor. There are no vulgar machine guns screaming here and “one-armed bandits” are not going crazy with colored fountains of light - here there is a quiet stiffness, broken by the wooden gavel of the presenter. You can see what the hall looks like in the picture. This is not a photograph, since photography is also prohibited there, this is a picture from a booklet. In this case, it doesn’t matter, because we were in this very hall.
In fact, their bingo is our bingo. Besides the fact that I think that lotto itself is quite a pleasant pastime, the atmosphere is, of course, captivating. There are even more grannies and venerable elders here than on the lower floors. This is a serious adult game. And it became clearer. that this is a very effective way to learn the English alphabet and numbers by ear.
Of course, I didn’t win anything, but I had fun to the fullest. Lena got herself a beer and some cocktails for me and won 50 dollars. Yes, the main beauty of bingo is that there is always a winner. You can see him in person because he yells "Bingo!" at the top of his lungs and stretches out his hand like an excellent student from the first desk.
Time flew by and we stayed for the second game.
Then we visited the restaurant, where we drank more beer, cocktails and had a wonderful dinner. However, maybe it was breakfast. I am very sorry that I cannot convey our conversation at the post-bing meal. I’m sorry, because the conversation itself was interesting, but I can’t, because there is too much personal information in it. What do you think two young beautiful Lenas can talk about in a Las Vegas restaurant after a couple of games of bingo and a couple of cocktails?
Assessment: the patient will note improvement in condition, elimination of suffocation, and demonstrate knowledge about the prevention of suffocation attacks. The goals will be achieved.
Problem No. 59
Calling a paramedic to a 4-year-old child. Complaints of repeated vomiting and loose stools for 2 days. According to the mother, the vomiting began after the child drank the milk. Vomiting is observed up to 3 times a day. After each act of defecation there is increasing weakness. Objectively: consciousness is clear, the child is adynamic, the skin is pale and dry, facial features are pointed. Subfebrile body temperature = 37.1º C, C, PS = 52 beats per minute. weak filling, A/D 78/40.
Medical diagnosis: CINE (intestinal infection of unknown form).
Tasks
Sample answers
1. The needs are violated: to be healthy, to eat, to drink, to excrete, to maintain body temperature.
Patient problems:
real:
Repeated vomiting
Dehydration,
Weakness,
Body temperature is low-grade;
potential:
The risk of deterioration of the condition associated with the development of complications, heart failure, dehydration.
2. Priority problems: diarrhea, dehydration.
Short-term goals: prevent the child from aspiration of vomit and further dehydration, stop diarrhea. Protect contacts from infection.
Long-term goals: The baby will be healthy at the time of discharge.
| Plan | Motivation |
| Nurse: will provide | |
| 1. Correct position: child (lying on his back, head turned to the side), use a functional bed. | 1. To avoid aspiration of vomit. |
| 2. Control the volume of excrement and vomit. | 2. To prevent exicosis. |
| 3. Hygienic child care. Frequent change of linen. | 3. To prevent diaper rash, skin irritation, and purulent complications. |
| 4. Constant monitoring of the child’s condition (A/D, PS, t). | 4. For early diagnosis and timely provision of emergency care in case of complications. |
| 5. Following the doctor’s medication prescriptions. | 5. To ensure the effectiveness of treatment. |
| 6. At the outbreak, he will provide isolation of contacts, monitoring of contacts for 7 days, and a biological examination. Preventive treatment of contacts. | 6. To avoid the spread of infections. |
| 7. Sanitary clearance. work on the prevention of intestinal and especially dangerous infections. | 7. To avoid the spread of infections. |
| 8. Giving an emergency notification to the SES. | 8. To avoid the spread of infections. |
Assessment: the patient will note an improvement in condition, absence of diarrhea and vomiting. The goals will be achieved.
Problem No. 60
During a regular visit to the clinic by a 1-year-old child weighing 10,700 grams, the nurse noticed a sharp pallor of the skin and mucous membranes. The mother reported that the child gets tired quickly, is irritable, inactive, and noted a loss of appetite. When questioning the mother, it was possible to establish that the child’s diet was monotonous: dairy foods, dairy products. The mother prefers not to give fruits and vegetables for fear of digestive problems. A child under 1 year old had ARVI 3 times. Blood history: Hb-100 g/l, Er-3.0x10 12, c.p. - 0.8
Medical diagnosis: Iron deficiency anemia.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. Violation of the need: - to eat, to be healthy, to rest, to play.
Patient problems:
real:
Anorexia errors in diet,
Fast fatiguability,
Irritability,
Weakness,
Paleness of the skin and mucous membranes.
potential:
Risk of developing moderate to severe anemia
The priority problem is anorexia.
1) short-term - the child’s appetite will improve by the end of the first week
2) long-term - the child’s parents will note an improvement in the child’s condition at the time of discharge, and will not complain about the child’s lack of appetite or increased irritability of the child.
| Plan | Motivation |
| Nurse: | |
| 1. Provides mental and physical peace. | |
| 2. Organizes the correct daily routine and nutrition (iron-containing foods). | 2. To ensure the necessary content of protein, vitamins and microelements in the body. |
| 3. The baby will be fed warm, small portions 5 times a day every 4 hours. | 3. For better absorption of nutrients in the body. |
| 4. Provide walks in the fresh air (in winter at least 3 times a day, in summer all day long), ventilation of the home (in winter - 5-10 minutes, in summer the whole day). | 4. For the prevention of secondary infectious diseases. For better aeration of the lungs, enriching the air with oxygen. |
| 5. Have a conversation with parents about the need for adequate nutrition. | 5. To compensate for the loss of protein, Fe, vitamins and increase the body’s defenses. |
| 6. Will observe the appearance and: condition of the patient. | 6. For early diagnosis and timely provision of emergency care. |
| 7. Carry out a set of hygiene measures. | 7. To maintain cleanliness of the skin and mucous membranes to prevent bedsores. |
| 8. For the effectiveness of treatment. |
Assessment: the patient will feel satisfactory, become active and sociable. Parents will demonstrate knowledge about proper nutrition for their child. The goals will be achieved.
Problem No. 61
A 9-month-old boy was visited by a local doctor at home, on call. Parents complain of an increase in T to 39.2º C, convulsive twitching. I have been sick for 2 days, I have a runny nose and a dry cough. A child from the first pregnancy, which occurred with gestosis in the second half. Childbirth is urgent, physiological. Weight at birth - 2900 g, length - 49 cm. Breastfeeding up to 1 month. Rickets was diagnosed at 2 months, acute respiratory infections at the age of 5 months. Parents are healthy, there are no occupational hazards, higher education. Housing and living conditions are satisfactory.
Objectively: the condition is of moderate severity. Consciousness is clear. The skin is clean and pale. Extremities are cold. The pharynx mucosa is hyperemic. Nasal breathing is difficult, serous discharge from the nasal passages. Micropolyadenia. Muscle tone is diffusely reduced. A large fontanel 2.0x1.5 cm, the edges are dense, there is no craniotabes. 2 teeth. The chest is compressed from the sides, deployed in the lower aperture, “rosary”. “Bracelets” are palpated. Percussion and auscultation of the lungs without pathology. The boundaries of the heart are not expanded. The tones are loud, clear, rhythmic. The abdomen is soft and painless. The liver and spleen are not enlarged. Stool and urination are not impaired. No meningeal symptoms were detected.
In the presence of a doctor, an attack of convulsions occurred. The child had twitching of the limbs and bending of the body. The duration of the attack was 7 seconds, it stopped on its own. The body temperature at this moment was 39.5º C. After the attack, consciousness was restored.
Medical diagnosis: Rickets. ARVI.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. The needs are violated: to be healthy, to breathe, to eat, to drink, to be clean, to play, to rest, to maintain body temperature.
Patient problems:
real:
Runny nose,
Dry cough,
Fever;
Cramps,
weakness;
potential:
Threat of death due to hyperthermia.
2. The patient’s priority problem is fever, convulsions.
Short-term - the patient will note a decrease in body temperature, absence of cramps, absence of runny nose and cough after 2 days;
Long-term - the patient will note the absence of all symptoms of the disease at the time of discharge.
| Plan | Motivation |
| The nurse will provide: | |
| 1. Mental and physical peace. | 1. To ensure the correct rhythm of the processes of higher nervous activity. |
| 2. Drink plenty of warm drinks. | 2. In order to reduce intoxication and dehydration. |
| 3. Strict bed rest. | 3. To prevent complications; |
| 4. Care for skin and mucous membranes. | 4. For the prevention of purulent complications. |
| 5. Monitoring the patient’s condition (t, PS, AD, respiratory rate). | 5. For early diagnosis and timely assistance in case of complications. |
| 6. Following doctor’s orders. | |
| 7. Taking vitamins. | 7. To enhance immunity. |
| 8. Use of physical methods to cool the child. | . To reduce a child's temperature. |
| 9. Have a conversation with parents about the prevention of hyperthermia. | 9. For the prevention of hyperthermia and seizures. |
Assessment: the patient will note a significant improvement in his condition, the temperature will drop, and the seizures will stop. Parents will demonstrate knowledge of hyperthermia prevention. The goal will be achieved.
Problem No. 62
Tolya Ch., 5 months. The mother went to the doctor with complaints about the child’s restlessness, poor sleep, and itchy skin. These complaints appeared 4 days ago. A child from the 1st pregnancy, which occurred with toxicosis in the first half. Urgent birth, birth weight 3450 g, height 52 cm. He screamed immediately. In the maternity hospital, toxic erythema was noted. He was discharged on the 6th day in satisfactory condition. The late neonatal period proceeded without changes. He was breastfed for up to 3 months. From this age he was transferred to mixed feeding due to maternal hypogalactia. From the age of 4 months he was switched to artificial feeding and receives the “Baby” formula. Five days ago, 5% semolina porridge with cow's milk was introduced into the diet. From 2 months he receives freshly prepared apple juice, currently in an amount of 50 ml. He suffered from ARVI at 3 months of age, and therefore was not vaccinated. Parents consider themselves healthy. Mother works in the chemical laboratory of the Tasma plant. My maternal grandfather suffers from bronchial asthma. My paternal grandmother has erosive gastritis. Father smokes.
Objectively: the child is in moderate condition, excited, scratches his skin during examination. There are greasy crusts on the scalp and eyebrows. The skin of the cheeks is dry, flaky, and brightly hyperemic. On the skin of the trunk and limbs there are a small number of smooth, shiny papules and scratch marks. In the groin areas the skin is eroded, moderate hyperemia. Micropolyadenia. In the lungs there is a percussion sound of pulmonary, puerile breathing. The boundaries of the heart are not expanded, the tones are clear, the abdomen is painless. The spleen is not enlarged. The stool is unstable up to 4-5 times a day, semi-liquid, without pathological impurities.
Blood test: Er-4.0x10 12/l, Hb-120 g/l, leuk-10.2x10 9/l, p-4%, s-26%, e-9%, l-56:, m- 5%, ESR-16 mm/h. Urinalysis - specific weight - 1012, leukemia - 3-4 in the field of view, squamous epithelium - 1-3 in the field of view.
Medical diagnosis: Exudative diathesis.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. Needs are violated: to be healthy, to be clean, to sleep, to rest. Patient's problem: play, communicate, allocate.
real:
Skin itching;
Sleep disturbance;
Unstable stool;
Poor sleep;
The skin of the cheeks is dry, flaky, brightly hyperemic, papular rash on the body and limbs, eosinophilia in the blood, micropolyadenia.
potential:
Threat of developing chronic diseases (eczema, bronchial asthma)
2. The patient’s priority problems are skin itching, sleep disturbances.
Short-term: the child will notice a decrease in itching, improved sleep by the end of the first week;
Long-term: the child will note the absence of itching, rash, sleep will become restful by the time of discharge.
| Plan | Motivation |
| Nurse: | |
| 1. Provide the child with complete mental and physical peace. | 1. To ensure the correct rhythm of the processes of higher nervous activity. |
| 2. Apply hygienic baths with: chamomile infusion, furatsilin solution or ointment dressings. | 2. To reduce and treat itching. |
| 3. Provides care for the skin and mucous membranes; | 3. For the prevention of purulent complications. |
| 4. Ensure compliance with the daily routine, long stay in the fresh air. | 4. To improve the child’s condition, to prevent complications, and better aeration. |
| 5. Provide ventilation of the premises. | 5. To improve lung aeration. |
| 6. Fulfill doctor’s orders. | 6. For the effectiveness of treatment. |
| 7. Have a conversation with parents about the prevention of allergies and the need for a hypoallergenic diet. | 7. For the prevention of allergic conditions. |
Assessment: the child will notice an improvement in his condition, the itching will go away, there will be no rash, the parents will demonstrate knowledge about preventing allergies in the child. The goals will be achieved.
Problem No. 63
A 13-year-old boy was admitted to the hospital with complaints of pain in the epigastric region. Before admission to the hospital, there was vomiting “coffee grounds”, after which the pain subsided, but weakness, palpitations, dizziness, and tinnitus appeared.
On examination: pallor of the skin, reduced A/D, PS 110 per minute, upon palpation muscle tension in the epigastric region.
Medical diagnosis: Gastric ulcer.
Stomach bleeding.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. The needs are violated: to be healthy, to eat, to excrete, to move, to be clean, to communicate, to study.
Patient problems:
real:
Vomiting coffee grounds
Decrease in A/D,
Decrease in circulating blood volume,
Pain in the epigastric region,
Weakness,
Heartbeat
Dizziness,
Noise in ears,
Paleness of the skin;
potential:
The risk of developing an acute decrease in circulating blood volume and hemorrhagic shock.
2. The patient's priority problem: vomiting coffee grounds.
Short-term: the patient will note a decrease in weakness by the end of the day, there will be no vomiting on the 2nd day;
Long-term: the patient will note the disappearance of weakness and palpitations after 7 days, pain in the epigastric region will disappear by 9-10 days.
| Plan | Motivation |
| Nurse: | |
| 1. Provide an urgent call to a doctor. | 1. To provide emergency medical care |
| 2. Puts the patient in a horizontal position. | 2. To prevent further complications. |
| 3. Place a rubber balloon with ice on the epigastric region, first place a towel on the body | 3. To reduce bleeding. |
| 4. Will monitor PS, A/D, and skin. | 4. For early diagnosis of possible complications |
| 5. Will strictly follow the doctor’s orders | 5. To ensure effective treatment. |
| 6. Conduct a conversation about the prevention of peptic ulcers and intestinal bleeding. | 6. To prevent possible complications. |
Assessment: the patient will note a significant improvement in his condition, there will be no vomiting of coffee grounds. The patient will demonstrate knowledge about the prevention of peptic ulcer disease and complications. The goal will be achieved.
Problem No. 64
Seryozha, 3 years old, became acutely ill, with a temperature rise to 38.8º C. One-time vomiting, headache, and pain when swallowing were noted. By the end of the day a rash appeared. On examination: condition of moderate severity, temperature 39.3º C. There is an abundant pinpoint rash on the skin on a hyperemic background. White dermographism, tongue coated with white coating. The pharynx is clearly hyperemic, the tonsils are hypertrophied and swollen. Cardiac tachycardia. The tones are loud, the abdomen is painless. Stool and urine output are normal.
Medical diagnosis: scarlet fever.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. The needs are violated: to eat, drink, be healthy, be clean, maintain body temperature, sleep, rest, play.
Patient problem:
real:
Headache,
Fever,
A sore throat;
potential:
The risk of developing lymphadenitis, otitis,
Risk of developing nephritis, rheumatic carditis.
2. Priority problems: fever, headache, sore throat.
Short-term - the child will notice a decrease in itching, sore throat, improved sleep, by the 3rd day of the disease;
Long-term - the patient will note the disappearance of all symptoms of the disease.
By the 10th day, itching and sore throat will disappear, sleep will normalize.
| Plan | Motivation |
| Nurse: | |
| 1. Isolates the child in a separate room. | 1. To prevent scarlet fever from infecting other family members. |
| 2. Provide bed rest for at least 7 days | 2. To avoid complications from the heart and kidneys. |
| 3. Teach the child to gargle with furatsilin solution and soda solution after eating. | 3. To eliminate a sore throat and prevent a secondary infection. |
| 4. Provide the child with plenty of fluids. | 4. To eliminate intoxication. |
| 5. Repeat urine and blood tests. | 5. For early diagnosis of complications. |
| 6. After recovery, he will give the mother: a referral to a rheumatologist, an ENT doctor, and an ECG. | 6. For early diagnosis of complications. |
| 7. Will monitor the appearance and: condition of the patient, PS, respiratory rate. | 7. For early diagnosis and timely provision of: emergency care in case of complications. |
| 8. Will follow doctor’s orders. | 8. For effective treatment. |
| 9. Have a conversation with the child’s parents about the prevention of infectious diseases. | 9. For the prevention of infectious diseases. |
Assessment: disappearance of all symptoms of the disease. Parents will demonstrate knowledge about the prevention of infectious diseases.
The goals will be achieved.
During the next patronage visit to a 1-year-old child, the paramedic drew attention to the sharp pallor of the skin and mucous membranes. The mother reported that the child gets tired quickly, is irritable, inactive, and noted a loss of appetite. When questioning the mother, it was possible to establish that the child’s diet was monotonous, milk porridge twice a day. He prefers not to give fruits and vegetables for fear of indigestion. On this diet, the child gains weight, which makes the mother happy. They live in a hostel and rarely go out.Upon examination: the baby's condition is satisfactory. Pronounced pallor of the skin and secretion of mucous membranes, peripheral lymph nodes are not enlarged. From the side of the heart: a systolic murmur is heard. The abdomen is soft, the liver protrudes 2 cm from the hypochondrium. From the anamnesis it was revealed that the child was born full-term, on mixed feeding from 1 month, and often suffered from ARVI.
Tasks
2. Name additional symptoms to clarify the diagnosis, tell us about the method for identifying them.
3. Tell us about the principles of treating the disease.
4. How to prepare vegetable puree.
Sample answers
1. The child may have iron deficiency anemia. The main symptoms of the disease are: pale skin, fatigue, irritability, loss of appetite, lethargy. A systolic murmur is heard in the child's heart, and the liver is enlarged. Reasons: one-sided milk feeding, frequent illnesses, poor care and poor living conditions.2. To clarify the diagnosis, it is necessary to conduct a general blood test, where you can detect a decrease in the amount of Er less than 3.5x10 12 l, hemoglobin below 100 g/l, color index below 0.8. Er smears are pale in color, decrease in size, and exhibit moderate leukocytosis and reticulocytosis.
Patients may have additional symptoms of the disease: seizures in the corners of the mouth, waxy ears, dry skin, dull brittle hair, muscle hypotonia.
3. Treatment of the child should be comprehensive; children with moderate and severe forms of anemia are hospitalized; those with mild anemia are treated at home. It is necessary to organize the correct diet. Give foods containing iron and other microelements: meat products, liver, cottage cheese, yolk, fruits, vegetables. You need to be in the fresh air more.
A child of the first year is prescribed aloe syrup with iron, ferrocal 0.3 gx3 times a day after meals, feramide, ferospan, vitamin C, B vitamins. It is necessary to establish the correct daily routine for the child. The child should walk in the fresh air, he needs massage and gymnastics, daily bathing.
When hardening, children are less likely to suffer from colds and anemia.
4. To prepare vegetable puree, take a combination of 2-3 vegetables, wash, cut and then boil them for 20 minutes, then cool and rub through a sieve, add a decoction of vegetables and a salt solution, butter, mix everything.
Task No. 4.
A 13-year-old boy was admitted to the hospital with complaints of pain in the epigastric region. Before admission to the hospital, there was vomiting of “coffee grounds”, after which the pain subsided, but weakness, palpitations, dizziness, and tinnitus appeared.On examination: pallor of the skin, decreased A/D, PS 110 per minute, palpation of the abdomen - muscle tension in the epigastric region.
Tasks
1. Formulate and justify the presumptive diagnosis.2. Tell us about the scope of first aid and the rules of transportation to the destination.
3. Draw up a plan for diagnostic tests in the hospital, tell us about the principles of treatment.
4. Tell us about further medical examination.
5. Demonstrate the technique of intravenous administration of 10% calcium chloride solution.
Sample answers
1. Diagnosis: gastric ulcer, complicated by bleeding. The conclusion was given on the basis of complaints and an objective examination: vomiting “coffee grounds”, dizziness, weakness, pale skin, tachycardia, decreased A/D, pain, muscle tension in the epigastric region.2. First aid – lay the patient down, apply cold to the stomach area, swallow pieces of ice, urgent hospitalization, consultation with a surgeon.
3. Plan of diagnostic examination in the hospital:
a) general blood and urine analysis;
b) fibrogastroscopy of the stomach - to determine the nature of the ulcerative defect of the gastric mucosa.
Treatment: diet - table No. 1a, No. 1b, No. 1. Medicines that are needed are drugs that suppress Helicobacter pylori infection: denol, de-nol + oxacillin, de-nol + trichopolum. Antisecretory agents: pepsin, cholinomimetics, atropine, platiphylline, selective M1-cholinomimetics-gastrocetin, antacids and adsorbents, almagel. Maolox, Vikalin. Gastrocytoprotectors: cytotec, smecta, agents that normalize gastric motility: cerucal, No-shpa, papaverine. Sedatives: elenium, diazepam, valerian. Remedies: sea buckthorn oil, rosehip oil.
4. After discharge from the hospital, patients are registered with a gastroenterologist and surgeon. The course of anti-relapse treatment includes diet therapy, drug treatment and physiotherapeutic procedures. The diet is mechanically and chemically gentle: foods with coarse fiber, such as mushrooms, are excluded from the diet. To ensure chemical sparing, foods that increase juice secretion (meat broth, fried foods) are excluded from the diet.
5. Technique for intravenous administration of calcium chloride solution according to the manipulation algorithm.
Collection
Clinical tasks
Specializing in General Medicine
PEDIATRICS WITH CHILDHOOD INFECTIONS
Problem-situational tasks
Task No. 1.
The boy is 8 months old. Complaints about the child's lethargy, loss of appetite, unstable stool. A child from the 5th pregnancy, which proceeded favorably, 2 term births (weight - 3700 g, length - 50 cm). The neonatal period is without any peculiarities. Breastfeeding up to 2 months, from 3 months. semolina porridge was introduced without the advice of a doctor; unadapted mixtures were used. The child did not take vitamin D and rarely received juices. There were not walks every day. The weight gain was uneven. I suffered from acute respiratory infections 2 times. Material and living conditions are satisfactory.
Objectively: the general condition is satisfactory, but the child is lethargic, pale, and sweating. Sits with support on his hands, his back is round. Muscle tone is diffusely reduced. The head is square in shape, with prominent frontal and occipital protuberances. Large fontanel 2.5x3.0 cm, pliable edges. The back of the head is flattened and bald. No teeth. The chest is compressed from the sides, the lower edges are unfolded, there are small “rosary beads” on the ribs, and pronounced “bracelets” on the arms. There is kyphosis in the lumbar spine, which disappears when the child is positioned on his stomach. Palpation, percussion and auscultation did not reveal any changes in the respiratory and cardiac organs. The liver protrudes 2 cm from under the edge of the costal arch. The spleen is not enlarged. The stool is unstable, urination is not impaired.
Blood test: HB 102 g/l, Er-3.98x10 12 /l, L-4x10 9 /l, ESR 5 mm / hour. Urinalysis is unremarkable. Biochemical data: serum phosphorus 0:034 g/l, calcium 0.09 g/l.
Tasks
3. Write a prescription for vitamin D
4. Demonstrate techniques for measuring the height of children of different ages.
Sample answers
1. The child has rickets of the second degree, the peak stage. Iron deficiency anemia, mild. The conclusion is based on medical history: breastfeeding only up to 2 months, early introduction of complementary foods, lack of vegetables and fruit juices in the diet, did not receive vitamin D for preventive purposes.
Objective examination: sweating, pale skin, decreased muscle tone, severe deformation of the bones of the skull, chest, spine, and limbs.
Laboratory tests: a slight decrease in hemoglobin in the blood, a decrease in phosphorus and calcium in the blood serum.
2. An additional symptom of this form of the disease is craniotabes softening of individual areas of the occipital bone, which is determined by palpation. At the level of attachment of the diaphragm, a retraction occurs, a “Harrison’s groove,” and the timing and order of teeth eruption are disrupted.
3. In this case, the child does not need urgent hospitalization in a hospital, and under satisfactory material and living conditions, treatment can be carried out at home.
4. In a hospital setting, to confirm the diagnosis, it is necessary to take an x-ray of the distal bones of the forearm and determine the level of the enzyme alkaline phosphatase in the blood serum, which plays an important role in the processes of bone calcification. First of all, it is necessary to prescribe proper nutrition with the daily inclusion in the diet of vegetable puree, cow's milk, kefir, grated apple, yolk, cottage cheese, low-fat meat broth, meatballs, and liver. For 30-45 days, the child should receive specific treatment for rickets with vitamin D in the form of calciferol 1600 IU per day. Considering the presence of anemia in the child, iron supplements (aloe syrup with iron), ascorbic acid, vitamin B 1 should be prescribed. Massage, daily therapeutic exercises, pine baths, and walks in the fresh air are necessary.
5. Technique for measuring height in children of different ages according to the algorithm for performing manipulations.
Task No. 2.
A mother with a 2.5-year-old girl consulted a local doctor about frequent and painful urination in the child, abdominal pain and an increase in temperature to 37.5º C. She was examined by a surgeon, surgical pathology was excluded. These symptoms were observed twice during the year, and after examination a diagnosis of cystitis was made. Treatment was carried out on an outpatient basis. History of frequent colds (7 times acute respiratory infections in the last year). The parents are healthy, but the grandmother on my mother’s side has kidney disease.
Objectively: weight 11.5 kg, length 85 cm. Condition is satisfactory. Asthenic physique. The skin and visible mucous membranes are clean. Lymph nodes: tonsillar, painless, up to 0.8 cm in size, not fused with the surrounding tissue. The subcutaneous fat layer is developed satisfactorily. Above the lungs there is a percussion sound of pulmonary, puerile breathing is heard. The boundaries of the heart correspond to age. The tones are clear and rhythmic. The abdomen is soft, painful above the womb. The liver and spleen are not enlarged. Pasternatsky's symptom is positive on both sides. Urination is painful, 15 times a day.
In general urine analysis, the reaction is alkaline, relative density of urine is 1012, turbid, leukocytes 20-25, squamous epithelium 3-5 in the field of view. Blood test: ESR-25 mm per hour, L-12x10 9 /l, Hb-108 g/l. Zimnitsky test: daytime diuresis 300 ml, nighttime diuresis 500 ml, fluctuations in specific gravity 1005-1012.
Ultrasound of the kidneys: the size corresponds to age, the position and mobility are normal, there is compaction of the pyelocaliceal system on both sides, doubling of the kidney on the right.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Name additional symptoms to clarify the diagnosis, tell us about the method for identifying them.
3. Tell us about the scope of first aid and the rules of transportation to the destination.
4. Make a plan for diagnostic tests in a hospital, tell us about the patient’s preparation for them and the principles of treatment.
5. Demonstrate techniques for collecting urinalysis from infants.
Sample answers
1. The patient has a disease of the urinary system - chronic pyelonephritis against the background of congenital kidney pathology.
The conclusion is based on the history and complaints typical for this disease:
Frequent and painful urination;
Abdominal pain, increased body temperature;
Symptoms continued for a year.
She has a life history of frequent colds, and her maternal grandmother has kidney disease.
Objective examination data: the child has an asthenic build, his weight is below the norm, the abdomen is painful on palpation above the womb, positive Pasternatsky’s sign on both sides; increased frequency of urination up to 15 times;
Laboratory data in urine tests: (general, Zimnitsky test), low specific gravity, leukocyturia; nocturia. In the blood, the ESR is increased to 25 mm/hour, there is slight leukocytosis, and hemoglobin is decreased.
An ultrasound examination reveals thickening of the pyelocaliceal system on both sides and doubling of the kidney on the right.
2. To clarify the diagnosis, it is necessary to check for the presence of edema (swelling of the eyelids, legs), and monitor A/D.
3. If a child has kidney disease, he or she must be hospitalized in a hospital.
4. In the hospital it is necessary to carry out: urine tests according to Nechiporenko, Addis-Kakovsky to study urine sediment and count the formed elements; functional test according to Zimnitsky, reflecting the reduced ability of the kidneys to concentrate urine. X-ray urological examination methods are informative - excretory urography, voiding cystourography, which reveal the size, contours and location of the kidneys, uneven damage to their parenchyma, reflux and other obstacles to the outflow of urine. It is necessary to conduct a bacteriological examination of urine, sensitivity to antibiotics; Constantly monitor your blood pressure and the amount of fluid you drink and excrete.
Treatment program in hospital:
Bed rest throughout the febrile period;
Diet during the acute period, table No. 7, then table No. 5 (dairy-vegetable) with a limitation of spicy and salty foods. Additional amount of liquid from watermelon, juices, cranberry and lingonberry fruit drinks, alkaline mineral waters;
Antibacterial therapy for 10-15 days: semisynthetic penicillins, aminoglycosides, cephalosporins, nitrofuran drugs (furadonin, furazolidone; nevigramon, 5-NOK);
Vitamins C, group B
When remission is achieved after hospital treatment, herbal medicine (medicinal herbal infusions) is prescribed according to the scheme.
5. Technique for collecting a general urine test in infants according to the manipulation algorithm.
Task No. 3.
During the next patronage visit to a 1-year-old child, the paramedic drew attention to the sharp pallor of the skin and mucous membranes. The mother reported that the child gets tired quickly, is irritable, inactive, and noted a loss of appetite. When questioning the mother, it was possible to establish that the child’s diet was monotonous, milk porridge twice a day. He prefers not to give fruits and vegetables for fear of indigestion. On this diet, the child gains weight, which makes the mother happy. They live in a hostel and rarely go out.
Upon examination: the baby's condition is satisfactory. Pronounced pallor of the skin and secretion of mucous membranes, peripheral lymph nodes are not enlarged. From the side of the heart: a systolic murmur is heard. The abdomen is soft, the liver protrudes 2 cm from the hypochondrium. From the anamnesis it was revealed that the child was born full-term, on mixed feeding from 1 month, and often suffered from ARVI.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Name additional symptoms to clarify the diagnosis, tell us about the method for identifying them.
4. How to prepare vegetable puree.
Sample answers
1. The child may have iron deficiency anemia. The main symptoms of the disease are: pale skin, fatigue, irritability, loss of appetite, lethargy. A systolic murmur is heard in the child's heart, and the liver is enlarged. Reasons: one-sided milk feeding, frequent illnesses, poor care and poor living conditions.
2. To clarify the diagnosis, it is necessary to conduct a general blood test, where you can detect a decrease in the amount of Er less than 3.5x10 12 l, hemoglobin below 100 g/l, color index below 0.8. Er smears are pale in color, decrease in size, and exhibit moderate leukocytosis and reticulocytosis.
Patients may have additional symptoms of the disease: seizures in the corners of the mouth, waxy ears, dry skin, dull brittle hair, muscle hypotonia.
3. Treatment of the child should be comprehensive; children with moderate and severe forms of anemia are hospitalized; those with mild anemia are treated at home. It is necessary to organize the correct diet. Give foods containing iron and other microelements: meat products, liver, cottage cheese, yolk, fruits, vegetables. You need to be in the fresh air more.
A child of the first year is prescribed aloe syrup with iron, ferrocal 0.3 gx3 times a day after meals, feramide, ferospan, vitamin C, B vitamins. It is necessary to establish the correct daily routine for the child. The child should walk in the fresh air, he needs massage and gymnastics, daily bathing.
When hardening, children are less likely to suffer from colds and anemia.
4. To prepare vegetable puree, take a combination of 2-3 vegetables, wash, cut and then boil them for 20 minutes, then cool and rub through a sieve, add a decoction of vegetables and a salt solution, butter, mix everything.
Task No. 4.
A 13-year-old boy was admitted to the hospital with complaints of pain in the epigastric region. Before admission to the hospital, there was vomiting of “coffee grounds”, after which the pain subsided, but weakness, palpitations, dizziness, and tinnitus appeared.
On examination: pallor of the skin, decreased A/D, PS 110 per minute, palpation of the abdomen - muscle tension in the epigastric region.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Tell us about the scope of first aid and the rules of transportation to the destination.
3. Draw up a plan for diagnostic tests in the hospital, tell us about the principles of treatment.
4. Tell us about further medical examination.
5. Demonstrate the technique of intravenous administration of 10% calcium chloride solution.
Sample answers
1. Diagnosis: gastric ulcer, complicated by bleeding. The conclusion was given on the basis of complaints and an objective examination: vomiting “coffee grounds”, dizziness, weakness, pale skin, tachycardia, decreased A/D, pain, muscle tension in the epigastric region.
2. First aid – lay the patient down, apply cold to the stomach area, swallow pieces of ice, urgent hospitalization, consultation with a surgeon.
3. Plan of diagnostic examination in the hospital:
a) general blood and urine analysis;
b) fibrogastroscopy of the stomach - to determine the nature of the ulcerative defect of the gastric mucosa.
Treatment: diet - table No. 1a, No. 1b, No. 1. Medicines that are needed are drugs that suppress Helicobacter pylori infection: denol, de-nol + oxacillin, de-nol + trichopolum. Antisecretory agents: pepsin, cholinomimetics, atropine, platiphylline, selective M1-cholinomimetics-gastrocetin, antacids and adsorbents, almagel. Maolox, Vikalin. Gastrocytoprotectors: cytotec, smecta, agents that normalize gastric motility: cerucal, No-shpa, papaverine. Sedatives: elenium, diazepam, valerian. Remedies: sea buckthorn oil, rosehip oil.
4. After discharge from the hospital, patients are registered with a gastroenterologist and surgeon. The course of anti-relapse treatment includes diet therapy, drug treatment and physiotherapeutic procedures. The diet is mechanically and chemically gentle: foods with coarse fiber, such as mushrooms, are excluded from the diet. To ensure chemical sparing, foods that increase juice secretion (meat broth, fried foods) are excluded from the diet.
5. Technique for intravenous administration of calcium chloride solution according to the manipulation algorithm.
Task No. 5.
A mother with a 5-year-old girl came to the children's clinic for an appointment. The child has weakness, abdominal pain, decreased appetite, and in the evenings the temperature rises to 37.9º C. The mother noticed that the girl urinates often and her urine is cloudy. The tongue is dry, covered with a white coating. In the lungs, breathing is vesicular, heart sounds are muffled. The abdomen is soft and painless. The liver and spleen are not enlarged.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Name additional symptoms to clarify the diagnosis and methods for studying this disease.
3. Tell us about the principles of treating the disease.
4. Demonstrate the technique of collecting urine samples according to Zimnitsky.
Sample answers
1. Acute pyelonephritis.
The diagnosis is based on medical history and complaints: the child has weakness, abdominal pain, fever in the evenings, frequent urination, cloudy urine.
2. Additional symptoms of the disease are symptoms of intoxication: fatigue, loss of appetite, pallor of the skin, pain in the lumbar region, the presence of edema.
3. Treatment of pyelonephritis is complex. The child is prescribed a regimen and diet appropriate to his condition, as well as antibacterial and stimulant medications. Strict bed rest during the acute period of the disease until the condition and well-being improve, body temperature normalizes, urine and blood tests.
A sick child must urinate frequently. To do this, you should strictly follow the eating and drinking regime.
Antibiotics are prescribed. Phytotherapy is carried out. Lysozyme, prodigiosan, methyluracil, pentoxyl, and sodium nucleinate are used as immunocorrective agents.
If blood pressure rises, antihypertensive drugs are prescribed.
Therapeutic nutrition is based on the principles of a dairy-vegetable diet with a moderate amount of protein and salt. Fried foods and meat broths are not allowed. As the manifestations of pyelonephritis subside, the child is transferred to table No. 5. In the presence of metabolic disorders, limit the use of fish and meat to 2 times a week, mainly in boiled, stewed form using a potato and cabbage diet. Drinking plenty of fluids is recommended.
4. Urine analysis according to Zimnitsky should be collected according to the manipulation algorithm.
Task No. 6.
A 4-year-old girl has been sick for 2 days. Complains of weakness, lethargy, minor sore throat. On examination: temperature 37.9º С, condition of moderate severity, child is lethargic. Hyperemia of the pharynx is noted. On enlarged tonsils there are shiny grayish-white plaques (not removed with tampons). Sickly sweetish odor from the mouth. In the lungs there is vesicular breathing, no wheezing. Cardiovascular system without pathological changes. Stool and urination are normal. Not vaccinated for medical reasons.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Is hospitalization necessary in this case?
3. List possible complications.
4. Tell us about the principles of treatment.
5. Demonstrate the technique of taking a throat swab using a Loeffler stick.
Sample answers
1. A 4-year-old girl has a localized form of diphtheria of the pharynx. The diagnosis was made according to the anamnesis, complaints, objective examination: weakness, slight sore throat, t-37.9º C, hyperemia of the pharynx, grayish-white plaques on the enlarged tonsils (cannot be removed with tampons). Epidemic history: lack of vaccination for medical reasons.
2. The child is isolated in an infectious diseases hospital; to clarify the diagnosis, swabs are taken from the throat for Loeffler’s diphtheria bacillus. Bed rest, treatment with antitoxic diphtheria serum.
3. Possible complications: infectious-toxic shock, myocarditis, polyradiculoneuritis, acute glomerulonephritis.
4. Bed rest, nutritious, fortified diet.
The main thing in the treatment of all forms of diphtheria is the neutralization of diphtheria toxin with antitoxic diphtheria serum. The dose of serum depends on the form and severity of the disease. Before administering a therapeutic dose, a test is carried out according to the Bezredka method using 0.1 ml of serum diluted 1:100, injected intradermally; in 30 min. 0.2 ml of undiluted serum is administered subcutaneously and after 1.5 hours the remaining amount of serum is administered intramuscularly. For localized forms of diphtheria, serum is usually administered once.
5. The technique of taking a smear from the throat and nose on the BL is carried out according to the algorithm for performing the manipulations.
Task No. 7.
A paramedic was asked for help with a one-year-old child. I have been sick for three days, complaining of cough, severe runny nose, poor sleep, decreased appetite, lethargy.
Objectively: the child’s condition is moderate, t - 38.9º C, restless, severe catarrhal symptoms, profuse serous discharge from the nose, conjunctivitis, hemorrhage in the sclera, diffuse hyperemia in the pharynx, granularity of the posterior pharyngeal wall, enlarged submandibular lymph nodes. The skin is clean. In the lungs, breathing is puerile, wheezing is not heard. Heart sounds are sonorous, tachycardia. The stool is normal.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. List the methods for diagnosing the disease.
3. Tell us about the principles of treatment.
4. Demonstrate the Nechiporenko urine collection technique.
Sample answers
1. Clinical diagnosis: “Adenoviral infection” is made on the basis of:
History: complaints of cough, severe runny nose, poor sleep, decreased appetite, lethargy;
Objective examination: condition of moderate severity, temperature 38.9º C, catarrhal phenomena are expressed: profuse serous discharge from the nose, conjunctivitis, hemorrhages in the sclera, diffuse hyperemia in the pharynx, granularity of the posterior pharyngeal wall, enlargement of the submandibular lymph nodes.
2. Laboratory diagnostics:
a) serological testing for viruses of paired blood sera is carried out at intervals of
7-14 days;
b) culture of mucus from the nasopharynx for viruses 2 times;
c) immunofluorescent rapid method for detecting respiratory viruses in the columnar epithelium of the nasal passages. The answer can be obtained 3-4 hours after taking mucus from the nose.
Clarification of the epidemiological situation helps in making the correct diagnosis.
3. Children with ARVI can be treated at home, but the child must be isolated and kept in bed during the febrile period. A high-calorie diet with limited fat, meat products, and a predominance of fermented milk and fruit and vegetable dishes is necessary. Drinking plenty of fluids and symptomatic treatment are necessary.
Prescribe desensitizing drugs (diphenhydramine, suprastin, tavegil), antipyretics (paracetamol, panadol), multivitamins, alkaline inhalations, gargling (decoctions of chamomile, sage, eucalyptus, calendula), mustard plasters. The nasal mucosa is lubricated with oxaline ointment (0.25%).
When treating conjunctivitis, antiviral drugs - interferon - are instilled 6-8 times a day, 0.25% oxolinic or florenal ointment is placed in the nose 1-2 times a day.
The conjunctival sac is often washed with solutions of furatsilin (1:5000), rivanol (1:5000).
For severe forms, placental immunoglobulin is used. For bacterial complications, antibiotics are prescribed.
If there is heavy discharge from the nose, the mucus is sucked out using a rubber bulb. The nose is cleaned with turunda, vasoconstrictor drops are used (galazolin, sanorin, naphthyzin).
Specific prevention: influenza vaccines, but they are ineffective.
4. Urine collection technique according to Nechiporenko according to the manipulation algorithm.
Task No. 8.
A 3-year-old child lives with his parents in a dormitory and attends kindergarten. I fell acutely ill: temperature - 38.5º C, abdominal pain, vomiting once, frequent loose stools mixed with mucus, streaks of blood, the child is straining, restless. On examination: the child is pale, lethargic, muffled heart sounds, tachycardia, the abdomen is soft, the sigmoid is contracted, painful, the anus is pliable.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Name additional symptoms to clarify the diagnosis,
3. Make a plan for diagnostic tests in the hospital.
4. List possible complications.
5. Tell us about treatment methods.
6. Prevention of dysentery.
7. Demonstrate gastric lavage techniques.
Sample answers
1. Dysentery. The diagnosis is based on the history and complaints typical for this disease: t - 38.5º C, abdominal pain, vomiting once, frequent loose stools mixed with mucus, streaks of blood, the child is straining, restless; as well as objective examination data: the boy is pale, lethargic, heart sounds are muffled, tachycardia, the abdomen is soft, the sigmoid is contracted, painful, the anus is pliable.
2. Additionally, there may be symptoms of intoxication (headaches, weakness, decreased or lack of appetite). Symptoms of distal colitis develop: spasm and soreness of the lower part of the colon, excruciating nagging pain, false urges (tenesmus).
3. A child with any intestinal infection should be hospitalized in a children's infectious diseases hospital.
Diagnostic program in the hospital:
Laboratory and instrumental research methods;
Bacterial culture on the intestinal group;
Coprogram;
Sigmoidoscopy;
Indirect hemagglutination reaction. Bacterial culture for dysentery group.
4. Complications are possible with dysentery, especially in young children: pneumonia, gingivitis, stomatitis, otitis, anemia, dysbacteriosis. In severe dysentery, rectal prolapse is sometimes observed.
5. Treatment should be carried out taking into account the patient’s age, the severity of the infectious process and the period of the disease. On the first day, reduce the amount of food by 25%, prescribe fermented milk mixtures, liquid cereals, slimy soups, cottage cheese.
Etiotropic therapy: antibiotics, chemotherapy drugs and specific dysentery bacteriophage. Furazolidone, polymyxin, chloramphenicol are prescribed. In severe cases, prescribe gentamicin. The course of treatment with etiotropic drugs is 5-7 days. Along with etiotropic treatment in the acute period, it is advisable to prescribe vitamin C, groups B, A, E, and nonspecific immune stimulants: methyluracil, pentoxyl, sodium nucleinate.
To relieve intoxication, inject saline and colloidal solutions intravenously; 10% albumin solution, concentrated plasma, rheopolyglucin, 10% glucose solution. Infusion therapy is prescribed at the rate of 130-150 ml/kg body weight per day. For hyperthermia, prescribe the following medications: 50% analgin solution intramuscularly, paracetamol, aspirin.
6. Prevention. An important role in the fight against dysentery is played by: sanitary education of the population, universal implementation of sanitary and hygienic requirements, strict sanitary supervision of food enterprises and water supply. Hospitalization of patients with dysentery who work in the food industry is mandatory.
Current disinfection is carried out at the patient's bedside, and final disinfection is carried out after hospitalization. At the same time, a bacteriological examination of contact persons in the outbreak is prescribed. The child communicating with the patient is monitored for 7 days. When cases of the disease appear in the children's team, a one-time bacteriological examination of children and staff is carried out.
7. Gastric lavage technique according to the manipulation algorithm.
Task No. 9.
While providing patronage to a newborn child, the mother turned to a paramedic for advice due to the fact that her eldest daughter, 5 years old, had become capricious, irritable, her sleep and appetite had worsened, and she was complaining of periodic abdominal pain, itching in the anus, and nausea. The girl began to experience bedwetting.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Name additional symptoms to clarify the diagnosis.
3. Tell us about the treatment of this disease.
4. List methods of prevention.
5. Demonstrate the technique of scraping pinworm eggs.
Sample answers
1. Enterobiosis. The diagnosis is made on the basis of anamnesis, complaints typical for this disease: the child is capricious, irritable, sleep and appetite have worsened, complains of periodic abdominal pain, itching in the anus, nausea, and bedwetting is noted.
2. Pinworms can be detected on the surface of feces, and their eggs can also be removed from the perianal area with sticky, transparent plastic film, followed by microscopy.
3. Treatment. Pyrantel is effective in a single dose of 10 mg/kg, or piperazine adipate in an age-specific dosage for 5 days. If necessary, the course of treatment is repeated after 5 days. When treating enterobiasis, strict adherence to a hygienic regime is necessary. The prognosis is favorable. Control analysis - scraping for pinworm eggs is carried out after 1 month.
4. Prevention. Maintaining hygiene of body, clothing, home, simultaneous treatment of all family members. Parents are advised to monitor the child’s hygiene, wash vegetables, fruits, toys and household items, boil and iron and change bedding frequently. Carry out wet cleaning and ventilation of the room daily.
5. Technique for taking scrapings for enterobiasis according to the algorithm for performing the manipulation.
Task No. 10.
A 5-year-old child came to the kindergarten medical office. Today the mother discovered rashes all over the child’s body at normal temperatures. Almost all the children in the group got sick; no quarantine was announced.
Objectively: the girl’s condition is satisfactory, she is playing. On the skin of the face, torso and limbs there is a small papular rash of pink color against a normal skin background. The pharynx is hyperemic. The occipital lymph nodes are palpated to the size of a bean, elastic, painless. The heart and lungs are normal, the abdomen is soft, stool and urination are normal.
Tasks
1. Formulate and justify the presumptive diagnosis.
2. Name additional symptoms to clarify the diagnosis, tell us about the method for identifying them.
6 years old, became acutely ill, developed chills, repeated vomiting, and the temperature rose to 39o C. A local doctor was called, who, after examining the girl, gave a referral to the hospital.
Complaints upon admission: sore throat, headache, joint and muscle pain.
Objectively: the general condition is closer to severe. Correct physique, satisfactory nutrition. On a hyperemic background of the skin there is an abundant, pinpoint rash. Pulse 130 beats per minute, heart sounds are muffled. The tip of the tongue is papillary. The tongue is covered with a thick white coating. In the pharynx there is bright limited hyperemia, loose tonsils, purulent deposits on them. The submandibular lymph nodes are enlarged and painful on palpation.
Diagnosis: scarlet fever, severe course.
Tasks
1. Identify what needs are met in the child and the patient’s problems with justifying them.
3. Explain to the mother the need to use antibiotics for treatment.
4. Teach the mother how to collect urine from girls for general analysis.
5. Demonstrate throat and nasal swab collection on BL.
Sample answers
1. The child’s needs are violated: to be healthy, to maintain body temperature, to excrete, to be clean, to play, to communicate.
Patient problems
real:
A sore throat,
Headache,
Joint and muscle pain,
Fever,
Purulent plaque on the tonsils,
Isolation of the child.
potential:
Risk of developing myocarditis, nephritis.
Of these problems, the priority is fever, pain (throat,
joint, muscle, head).
2. Short-term goal: fever and pain will decrease within 2 days, and vomiting will stop.
Long-term goal: the baby will be healthy in 10 days without complications.
Plan
Motivation
Nurse:
1. Ensure that the child is isolated in a separate box for 10 days + 12 days at home. Will submit an emergency notification to the SES.
1. To prevent the spread of the disease (according to epidemic indications).
2. Provide bed rest until the fever and severe symptoms of intoxication disappear.
Tasks
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. Violation of the need: - to eat, to be healthy, to rest, to play.
Patient problems:
real:
Anorexia errors in diet,
Fast fatiguability,
Irritability,
Weakness,
Paleness of the skin and mucous membranes.
potential:
Risk of developing moderate to severe anemia
The priority problem is anorexia.
1) short-term - the child’s appetite will improve by the end of the first week
2) long-term - the child’s parents will note an improvement in the child’s condition at the time of discharge, and will not complain about the child’s lack of appetite or increased irritability of the child.
Plan
Motivation
Nurse:
1. Provides mental and physical peace.
2. Organizes the correct daily routine and nutrition (iron-containing foods).
2. To ensure the necessary content of protein, vitamins and microelements in the body.
3. The baby will be fed warm, small portions 5 times a day every 4 hours.
3. For better absorption of nutrients in the body.
4. Provide walks in the fresh air (in winter at least 3 times a day, in summer all day long), ventilation of the home (in winter - 5-10 minutes, in summer the whole day).
4. For the prevention of secondary infectious diseases. For better aeration of the lungs, enriching the air with oxygen.
5. Have a conversation with parents about the need for adequate nutrition.
5. To compensate for the loss of protein, Fe, vitamins and increase the body’s defenses.
6. Will observe the appearance and: condition of the patient.
6. For early diagnosis and timely provision of emergency care.
7. Carry out a set of hygiene measures.
7. To maintain cleanliness of the skin and mucous membranes to prevent bedsores.
8. For the effectiveness of treatment.
Assessment: the patient will feel satisfactory, become active and sociable. Parents will demonstrate knowledge about proper nutrition for their child. The goals will be achieved.
Problem No. 61
A 9-month-old boy was visited by a local doctor at home, on call. Parents complain of an increase in T to 39.2º C, convulsive twitching. I have been sick for 2 days, I have a runny nose and a dry cough. A child from the first pregnancy, which occurred with gestosis in the second half. Childbirth is urgent, physiological. Weight at birth - 2900 g, length - 49 cm. Breastfeeding up to 1 month. Rickets was diagnosed at 2 months, acute respiratory infections at the age of 5 months. Parents are healthy, prof. no harm, higher education. Housing and living conditions are satisfactory.
Objectively: the condition is of moderate severity. Consciousness is clear. The skin is clean and pale. Extremities are cold. The pharynx mucosa is hyperemic. Nasal breathing is difficult, serous discharge from the nasal passages. Micropolyadenia. Muscle tone is diffusely reduced. A large fontanel 2.0x1.5 cm, the edges are dense, there is no craniotabes. 2 teeth. The chest is compressed from the sides, deployed in the lower aperture, “rosary”. “Bracelets” are palpated. Percussion and auscultation of the lungs without pathology. The boundaries of the heart are not expanded. The tones are loud, clear, rhythmic. The abdomen is soft and painless. The liver and spleen are not enlarged. Stool and urination are not impaired. No meningeal symptoms were detected.
In the presence of a doctor, an attack of convulsions occurred. The child had twitching of the limbs and bending of the body. The duration of the attack was 7 seconds, it stopped on its own. The body temperature at this moment was 39.5º C. After the attack, consciousness was restored.
Medical diagnosis: Rickets. ARVI.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. The needs are violated: to be healthy, to breathe, to eat, to drink, to be clean, to play, to rest, to maintain body temperature.
Patient problems:
real:
Runny nose,
Dry cough,
Fever;
Cramps,
weakness;
potential:
Threat of death due to hyperthermia.
2. The patient’s priority problem is fever, convulsions.
Short-term - the patient will note a decrease in body temperature, absence of cramps, absence of runny nose and cough after 2 days;
Long-term - the patient will note the absence of all symptoms of the disease at the time of discharge.
Plan
Motivation
The nurse will provide:
1. Mental and physical peace.
1. To ensure the correct rhythm of the processes of higher nervous activity.
2. Drink plenty of warm drinks.
2. In order to reduce intoxication and dehydration.
3. Strict bed rest.
3. To prevent complications;
4. Care for skin and mucous membranes.
4. For the prevention of purulent complications.
5. Monitoring the patient’s condition
(t, PS, AD, NPV).
5. For early diagnosis and timely assistance in case of complications.
6. Following doctor’s orders.
6. For the effectiveness of treatment.
7. Taking vitamins.
7. To enhance immunity.
8. Use of physical methods to cool the child.
To reduce a child's temperature.
9. Have a conversation with parents about the prevention of hyperthermia.
9. For the prevention of hyperthermia and seizures.
Assessment: the patient will note a significant improvement in his condition, the temperature will drop, and the seizures will stop. Parents will demonstrate knowledge of hyperthermia prevention. The goal will be achieved.
Problem No. 62
5 months. The mother went to the doctor with complaints about the child’s restlessness, poor sleep, and itchy skin. These complaints appeared 4 days ago. A child from the 1st pregnancy, which occurred with toxicosis in the first half. Urgent birth, birth weight 3450 g, height 52 cm. He screamed immediately. In the maternity hospital, toxic erythema was noted. He was discharged on the 6th day in satisfactory condition. The late neonatal period proceeded without changes. He was breastfed for up to 3 months. From this age he was transferred to mixed feeding due to maternal hypogalactia. From the age of 4 months he was switched to artificial feeding and receives the “Baby” formula. Five days ago, 5% semolina porridge with cow's milk was introduced into the diet. From 2 months he receives freshly prepared apple juice, currently in an amount of 50 ml. He suffered from ARVI at 3 months of age, and therefore was not vaccinated. Parents consider themselves healthy. Mother works in the chemical laboratory of the Tasma plant. My maternal grandfather suffers from bronchial asthma. My paternal grandmother has erosive gastritis. Father smokes.
Objectively: the child is in moderate condition, excited, scratches his skin during examination. There are greasy crusts on the scalp and eyebrows. The skin of the cheeks is dry, flaky, and brightly hyperemic. On the skin of the trunk and limbs there are a small number of smooth, shiny papules and scratch marks. In the groin areas the skin is eroded, moderate hyperemia. Micropolyadenia. In the lungs there is a percussion sound of pulmonary, puerile breathing. The boundaries of the heart are not expanded, the tones are clear, the abdomen is painless. The spleen is not enlarged. The stool is unstable up to 4-5 times a day, semi-liquid, without pathological impurities.
Blood test: Er-4.0x10 12/l, Hb-120 g/l, leuk-10.2x10 9/l, p-4%, s-26%, e-9%, l-56:, m- 5%, ESR-16 mm/h. Urinalysis - beat. weight - 1012, leukemia - 3-4 in the field of view, squamous epithelium - 1-3 in the field of view.
Medical diagnosis: Exudative diathesis.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. Needs are violated: to be healthy, to be clean, to sleep, to rest. Patient's problem: play, communicate, allocate.
real:
Skin itching;
Sleep disturbance;
Unstable stool;
Poor sleep;
The skin of the cheeks is dry, flaky, brightly hyperemic, papular rash on the body and limbs, eosinophilia in the blood, micropolyadenia.
potential:
Threat of developing chronic diseases (eczema, bronchial asthma)
2. The patient’s priority problems are skin itching, sleep disturbances.
Short-term: the child will notice a decrease in itching, improved sleep by the end of the first week;
Long-term: the child will note the absence of itching, rash, sleep will become restful by the time of discharge.
Plan
Motivation
Nurse:
1. Provide the child with complete mental and physical peace.
1. To ensure the correct rhythm of the processes of higher nervous activity.
2. Apply hygienic baths with: chamomile infusion, furatsilin solution or ointment dressings.
2. To reduce and treat itching.
3. Provides care for the skin and mucous membranes;
3. For the prevention of purulent complications.
4. Ensure compliance with the daily routine, long stay in the fresh air.
4. To improve the child’s condition, to prevent complications, and better aeration.
5. Provide ventilation of the premises.
5. To improve lung aeration.
6. Fulfill doctor’s orders.
6. For the effectiveness of treatment.
7. Have a conversation with parents about the prevention of allergies and the need for a hypoallergenic diet.
7. For the prevention of allergic conditions.
Assessment: the child will notice an improvement in his condition, the itching will go away, there will be no rash, the parents will demonstrate knowledge about preventing allergies in the child. The goals will be achieved.
Problem No. 63
A 13-year-old boy was admitted to the hospital with complaints of pain in the epigastric region. Before admission to the hospital, there was vomiting “coffee grounds”, after which the pain subsided, but weakness, palpitations, dizziness, and tinnitus appeared.
On examination: pallor of the skin, reduced A/D, PS 110 per minute, upon palpation muscle tension in the epigastric region.
Medical diagnosis: Gastric ulcer.
Stomach bleeding.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. The needs are violated: to be healthy, to eat, to excrete, to move, to be clean, to communicate, to study.
Patient problems:
real:
Vomiting coffee grounds
Decrease in A/D,
Decrease in circulating blood volume,
Pain in the epigastric region,
Weakness,
Heartbeat
Dizziness,
Noise in ears,
Paleness of the skin;
potential:
The risk of developing an acute decrease in circulating blood volume and hemorrhagic shock.
2. The patient's priority problem: vomiting coffee grounds.
Short-term: the patient will note a decrease in weakness by the end of the day, there will be no vomiting on the 2nd day;
Long-term: the patient will note the disappearance of weakness and palpitations after 7 days, pain in the epigastric region will disappear by 9-10 days.
Plan
Motivation
Nurse:
1. Provide an urgent call to a doctor.
1. To provide emergency medical care
2. Puts the patient in a horizontal position.
2. To prevent further complications.
3. Place a rubber balloon with ice on the epigastric region, first place a towel on the body
3. To reduce bleeding.
4. Will monitor PS, A/D, and skin.
4. For early diagnosis of possible complications
5. Will strictly follow the doctor’s orders
5. To ensure effective treatment.
6. Conduct a conversation about the prevention of peptic ulcers and intestinal bleeding.
6. To prevent possible complications.
Assessment: the patient will note a significant improvement in his condition, there will be no vomiting of coffee grounds. The patient will demonstrate knowledge about the prevention of peptic ulcer disease and complications. The goal will be achieved.
Problem No. 64
Seryozha, 3 years old, became acutely ill, with a temperature rise to 38.8º C. One-time vomiting, headache, and pain when swallowing were noted. By the end of the day a rash appeared. On examination: condition of moderate severity, temperature 39.3º C. There is an abundant pinpoint rash on the skin on a hyperemic background. White dermographism, tongue coated with white coating. The pharynx is clearly hyperemic, the tonsils are hypertrophied and swollen. Cardiac tachycardia. The tones are loud, the abdomen is painless. Stool and urine output are normal.
Medical diagnosis: scarlet fever.
Tasks
1. Identify the needs whose satisfaction is disrupted; formulate and justify the patient’s problems.
2. Identify goals and create a motivational nursing intervention plan.
Sample answers
1. The needs are violated: to eat, drink, be healthy, be clean, maintain body temperature, sleep, rest, play.
Patient problem:
real:
Headache,
Fever,
A sore throat;
potential:
The risk of developing lymphadenitis, otitis,
Risk of developing nephritis, rheumatic carditis.
2. Priority problems: fever, headache, sore throat.
Short-term - the child will notice a decrease in itching, sore throat, improved sleep, by the 3rd day of the disease;
Long-term - the patient will note the disappearance of all symptoms of the disease.
By the 10th day, itching and sore throat will disappear, sleep will normalize.
Plan
Motivation
Nurse:
1. Isolates the child in a separate room.
1. To prevent scarlet fever from infecting other family members.
2. Provide bed rest for at least 7 days
2. To avoid complications from the heart and kidneys.
3. Teach the child to gargle with furatsilin solution and soda solution after eating.
3. To eliminate a sore throat and prevent a secondary infection.
4. Provide the child with plenty of fluids.
4. To eliminate intoxication.
5. Repeat urine and blood tests.
5. For early diagnosis of complications.
6. After recovery, he will give the mother: a referral to a rheumatologist, an ENT doctor, and an ECG.
6. For early diagnosis of complications.
7. Will monitor the appearance and: condition of the patient, PS, respiratory rate.
7. For early diagnosis and timely provision of: emergency care in case of complications.
8. Will follow doctor’s orders.
8. For effective treatment.
9. Have a conversation with the child’s parents about the prevention of infectious diseases.
9. For the prevention of infectious diseases.
Assessment: disappearance of all symptoms of the disease. Parents will demonstrate knowledge about the prevention of infectious diseases.
The goals will be achieved.
Tasks for providing first aid in emergency conditions
Problem No. 65
A 12-year-old girl was brought to the first aid station after accidentally drinking a solution of caustic soda. Suffering from acute pain in the mouth, throat and chest. There is drooling due to the inability to take at least one sip. There are traces of burns on the lips, tongue, and mucous membranes of the cheeks. The condition is serious. The girl is crying in pain, pale, pulse 100 beats/min.
Tasks
3. Demonstrate the intradermal injection technique.
Sample answers
1. Poisoning with caustic soda solution.
a) before gastric lavage, premedicate with a 1% solution of promedol 0.1 ml/year intramuscularly;
b) rinse the stomach with cold water or a weak solution of 1-2% citric acid;
c) introduce an enveloping agent;
d) hospitalize in a hospital for further observation and treatment;
3. Intradermal injection technique according to the manipulation algorithm;
1.
A 9-year-old girl suffers from diabetes. Receives 20 units in the morning. insulin. After taking insulin, I was late for school and didn’t have breakfast. During the first lesson, convulsions suddenly appeared and she lost consciousness. The skin is moist, shallow breathing, dilated pupils, clonic-tonic convulsions.
Tasks
1. Identify the patient’s emergency condition.
2. Draw up an emergency care algorithm.
3. Demonstrate the subcutaneous injection technique to the child.
Sample answers
1. Hypoglycemic coma.
2. Emergency care algorithm:
a) administer 10-20 ml intravenously. 40% glucose solution;
b) when blood pressure decreases, administer intravenously plasma and its substitutes: polyglucin, rheopolyglucin, albumin and cardiac glycosides: corglycon - 0.06% solution 0.5 mg/kg slowly intravenously, hormones: prednisolone, hydrocortisone 5 ml/kg;
c) for convulsions, administer diazepam 0.3-0.5 ml/kg slowly intravenously or sodium hydroxybutyrate 20% solution 0.5-0.75 ml/kg;