Has little effect on the biotransformation of drugs. What is biotransformation of drugs? Change in drug activity
Every day, any person is exposed to the negative effects of various chemicals called xenobiotics. They enter the body through the skin, lungs, and from the digestive tract along with food and air. Some of these substances do not have a negative effect on the body, but most are capable of causing biological responses. As a result, they are neutralized and removed from the body.
Definition
Biotransformation is a concept that includes the basic chemical changes that occur with drugs in the body.
As a result of this process, a decrease in lipophilicity in fats is observed), hydrophilicity increases (solubility in water increases).
Biotransformation of medicinal substances leads to changes in the pharmacological activity of the drug.
A small amount of the drug may be excreted unchanged by the kidneys. Basically, such drugs are “small molecules”, or can be in ionized form at pH values close to physiological indicators.
Unfortunately, many drugs do not have such physicochemical properties. Basically, physiologically active molecules of organic compounds are lipophilic, therefore, at physiological pH parameters they remain in a non-ionized form. They are bound to plasma protein, so they are slightly filtered in the glomeruli.
Biotransformation is a process aimed at increasing the solubility of drug molecules and accelerating its removal from the body along with urine. That is, the transformation of lipophilic drugs into hydrophilic compounds is observed.

Change in drug activity
Biotransformation of substances leads to significant changes in the physiological activity of drugs:
- the drug is converted from the active substance to an inactive form;
- “prodrugs” thereby acquire pharmacological activity.
The safety of drugs that contain active metabolites is influenced not only by the pharmacokinetics of the drug, but also by the indicators of the active metabolites.

Prodrugs
The purpose of creating such drugs is to increase pharmacological parameters, accelerate and increase the absorption of drugs. For example, ampicillin esters (talampicin, pivampicin, bicampicin) have been developed, which, unlike the parent drug, are absorbed orally to the maximum extent during administration.
Biotransformation reactions allow these drugs to be hydrolyzed in the liver. The catalyst in the process is the enzyme carboxylesterase, which has high antibacterial activity.
Biotransformation is a process that significantly increases the effectiveness of drugs. The antiviral drug "Valacyclovir" is bioavailable - more than half of it is converted into acyclovir in the liver. This process is explained by the presence of amino acid residues - valine - in the molecules.
The mechanism of action of adenosine-converting enzyme inhibitors, which contain carbonyl groups, is also of interest.
These include the following drugs: “Perindopril”, “Quinapril”, “Enalapril”, “Spirapril”, “Trandolapril”, “Ramipril”.
In this case, biotransformation is the conversion of the drug by hydrolysis into active enalaprilat. The process is carried out thanks to the enzyme carboxylesterase. If you take the drug itself, then its absorption in the body does not exceed 10 percent.

Improving drug safety
Biotransformation of xenobiotics makes it possible to increase the safety of drugs. For example, scientists managed to develop Sulindac, an NSAID. This drug does not initially block the synthesis of prostaglandins; only in the liver, during hydrolysis, active sulindac sulfide is formed, which has anti-inflammatory activity. At first, scientists believed that the drug had no effect, but as a result of research, it was possible to establish a similarity in the number of occurrences of erosive and ulcerative lesions of the digestive organs in the case of taking Sulindac and other NSAIDs.
Selectivity of action
Liver biotransformation is a whole complex of biochemical reactions that make it possible to convert drugs into metabolites that are excreted from the body.
Among the goals of creating prodrugs, one can note an increase in the selectivity of the action of drugs, which helps to increase the effectiveness and safety of drugs. "Dopamine" is used to increase renal blood flow in renal failure, but the drug has an effect on the blood vessels and myocardium. An increase in blood pressure, the development of arrhythmias and tachycardias were also detected when using this drug.
After adding a fragment of glutamic acid to dopamine, a new drug called Glutamyl-dopa was developed. When hydrolyzed in the kidneys, dopamine is formed under the influence of L-aromatic amino acid decarboxylase and glutamyl transpeptidase, without causing undesirable effects on central hemodynamics.

Main phases
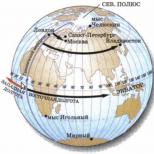
The figure shows the phases of biotransformation. After the drug enters the body, glucuronidation, sulfation, acetylation, methylation, conjugation with glutatin and amino acids occurs. Next, the drug is eliminated from the body.
All major biotransformations take place in the liver, but they can also occur in the kidneys, lungs, and digestive tract.
How is biotransformation carried out? Metabolism involves two phases: non-synthetic and synthetic.
Non-synthetic reactions
First-phase reactions are associated with the transition of drugs into more soluble (hydrophilic) compounds compared to the original substance. Changes in the initial physical and chemical parameters of drugs are explained by the process of addition or release of active functional groups: amino groups, sulfhydryl fragments, hydroxyl groups.
In the first stage, oxidation reactions occur. The most common process is hydroxylation, which involves the addition of an OH radical to the starting substance.
It is in this phase of biotransformation that the “hacking” of the original structure of the drug molecule occurs. Enzymes act as accelerators of oxidative processes (catalysts). Their substrate specificity is quite low, which explains their use as accelerators of oxidative interactions.

Synthetic reactions
Reactions of the second phase of biotransformation refer to the processes of combination (conjugation) of drugs or their metabolites with certain endogenous substances. The products of such interactions are polar conjugates that have high solubility in water and are quickly excreted from the body by bile or kidneys.
In order to enter into a phase 2 reaction, the molecule must have an active chemical group (radical), to which the conjugating molecule will attach. If such groups are initially present in the drug, then the interaction does not involve the first phase.
In some cases, drug molecules acquire active radicals directly during the chemical interaction at the first stage.
Passage through the liver
Most of the biotransformation of drugs occurs in the liver. Those that are carried out in the liver are divided into two subgroups: with high and low hepatic clearance.
The drugs of the first subgroup are characterized by a high degree of extraction (extraction) from the blood, which is explained by the high activity of the enzymatic systems that metabolize them. Because they are quickly and easily metabolized in the liver, clearance is related to the rate of blood flow in the liver.
For the second group, a connection was found with enzyme activity and the degree of binding of drugs to blood proteins. The capacity of enzyme systems is not a constant value; it can be increased by changing the dose of the drug.

Conclusion
When taking medications with high hepatic clearance, they are absorbed into the small intestine. They enter the liver through the portal vein. Here they are actively metabolized before they enter the circulatory system. This process is called presystemic elimination (“first-pass effect”). As a result, such drugs are low when taken internally, and absorption in this case is almost one hundred percent. This effect is achieved by such drugs as acetylsalicylic acid, Aminazine, Imipramine, Morphine, Reserpine, Salicylamide.
Genetic factors can have a significant impact on the pharmacokinetics of drugs. Depending on the rate of metabolism of drugs in the body, “extensive” and “slow” metabolizers are distinguished.
Specialists must take into account the patient’s genetic characteristics when selecting a group of medications.
Thanks to modern research methods used in modern scientific laboratories, pharmacists are constantly improving the quality of medications, increasing their absorption rate and effectiveness. As a result of these actions, it is possible to speed up recovery and reduce the negative impact of drugs on humans.
15. Biotransformation of drugs in the body, its main pathways, their characteristics. Factors influencing biotransformation.
Biotransformation of drugs– chemical transformations of drugs in the body.
Biological meaning of drug biotransformation: creation of a substrate convenient for subsequent utilization (as an energy or plastic material) or in accelerating the elimination of drugs from the body.
The main direction of metabolic transformations of drugs: non-polar drugs → polar (hydrophilic) metabolites excreted in the urine.
There are two phases of metabolic reactions of drugs:
1) Metabolic transformation (non-synthetic reactions, phase 1)- transformation of substances due to microsomal and extramicrosomal oxidation, reduction and hydrolysis
2) conjugation (synthetic reactions, phase 2)- a biosynthetic process accompanied by the addition of a number of chemical groups or molecules of endogenous compounds to a medicinal substance or its metabolites through a) the formation of glucuronides b) glycerol esters c) sulfoesters d) acetylation e) methylation
The influence of biotransformation on the pharmacological activity of drugs:
1) most often, biotransformation metabolites do not have pharmacological activity or their activity is reduced compared to the original substance
2) in some cases, metabolites can remain active and even exceed the activity of the original substance (codeine is metabolized to the more pharmacologically active morphine)
3) sometimes toxic substances are formed during biotransformation (metabolites of isoniazid, lidocaine)
4) sometimes during biotransformation metabolites with opposite pharmacological properties are formed (metabolites of non-selective b2-adrenergic receptor agonists have the properties of blockers of these receptors)
5) a number of substances are prodrugs that initially do not produce pharmacological effects, but during biotransformation are converted into biologically active substances (inactive L-dopa, penetrating the BBB, is converted in the brain into active dopamine, while there are no systemic effects of dopamine).
Clinical significance of drug biotransformation. The influence of gender, age, body weight, environmental factors, smoking, alcohol on the biotransformation of drugs.
Clinical significance of drug biotransformation: Since the dose and frequency of administration required to achieve effective concentrations in the blood and tissues may vary in patients due to individual differences in the distribution, metabolic rate and elimination of drugs, it is important to take them into account in clinical practice.
The influence of various factors on the biotransformation of drugs:
A) Functional state of the liver: with its diseases, drug clearance usually decreases, and the half-life increases.
B) Influence of environmental factors: smoking promotes the induction of cytochrome P450, resulting in accelerated drug metabolism during microsomal oxidation
IN) For vegetarians biotransformation of drugs is slowed down
D) elderly and young patients are characterized by increased sensitivity to the pharmacological or toxic effects of drugs (in elderly people and in children under 6 months, the activity of microsomal oxidation is reduced)
D) in men, the metabolism of some drugs occurs faster than in women, because androgens stimulate the synthesis of microsomal liver enzymes (ethanol)
E) High protein content and intense physical activity: acceleration of drug metabolism.
AND) Alcohol and obesity slow down drug metabolism
Metabolic drug interactions. Diseases affecting their biotransformation.
Metabolic interaction of drugs:
1) induction of drug metabolism enzymes - an absolute increase in their quantity and activity due to the influence of certain drugs on them. Induction leads to an acceleration of drug metabolism and (usually, but not always) to a decrease in their pharmacological activity (rifampicin, barbiturates - inducers of cytochrome P450)
2) inhibition of drug metabolism enzymes - inhibition of the activity of metabolic enzymes under the influence of certain xenobiotics:
A) competitive metabolic interaction - drugs with high affinity for certain enzymes reduce the metabolism of drugs with lower affinity for these enzymes (verapamil)
B) binding to a gene that induces the synthesis of certain isoenzymes of cytochrome P450 (cymedine)
B) direct inactivation of cytochrome P450 isoenzymes (flavonoids)
Diseases affecting drug metabolism:
A) kidney diseases (impaired renal blood flow, acute and chronic kidney diseases, outcomes of long-term renal diseases)
B) liver diseases (primary and alcoholic cirrhosis, hepatitis, hepatomas)
C) diseases of the gastrointestinal tract and endocrine organs
C) individual intolerance to certain drugs (lack of acetylation enzymes - aspirin intolerance)
V.G. Kukes, D.A. Sychev, G.V. Ramenskaya, I.V. Ignatiev
Humans are exposed to a variety of foreign chemicals called “xenobiotics” every day. Xenobiotics enter the human body through the lungs, skin and from the digestive tract as part of impurities in air, food, drinks, and drugs. Some xenobiotics have no effect on the human body. However, most xenobiotics can cause biological responses. The body reacts to drugs in the same way as to any other xenobiotic. In this case, drugs become objects of various mechanisms of influence from the body. This, as a rule, leads to the neutralization and elimination (removal) of drugs. Some drugs, easily soluble in water, are eliminated unchanged by the kidneys; other substances are preliminarily exposed to enzymes that change their chemical structure. Thus, biotransformation is a general concept that includes all chemical changes that occur with drugs in the body. The result of the biological transformation of drugs: on the one hand, the solubility of substances in fats decreases (lipophilicity) and their solubility in water increases (hydrophilicity), and on the other hand, the pharmacological activity of the drug changes.
Reducing lipophilicity and increasing hydrophilicity of drugs
A small number of drugs can be excreted unchanged by the kidneys. Most often, these drugs are “small molecules” or they are able to be in an ionized state at physiological pH values. Most drugs do not have such physicochemical properties. Pharmacologically active organic molecules are often lipophilic and remain non-ionized at physiological pH values. These drugs are usually bound to plasma proteins, are poorly filtered in the renal glomeruli and at the same time are easily reabsorbed in the renal tubules. Biotransformation (or the biotransformation system) is aimed at increasing the solubility of the drug molecule (increasing hydrophilicity), which facilitates its excretion from the body in the urine. In other words, lipophilic drugs are converted into hydrophilic and, therefore, more easily excreted compounds.
Changes in the pharmacological activity of drugs
Directions of changes in the pharmacological activity of drugs as a result of biotransformation.
A pharmacologically active substance is converted into a pharmacologically inactive substance (this is typical for most drugs).
At the first stage, a pharmacologically active substance is converted into another pharmacologically active substance (Table 5-1).
An inactive pharmacological drug is converted in the body into a pharmacologically active substance; such drugs are called “prodrugs” (Table 5-2).
Table 5-1. Medicines whose metabolites retain pharmacological activity
End of Table 5-1
 Table 5-2. Prodrugs
Table 5-2. Prodrugs
 End of Table 5-2
End of Table 5-2
 * Phenacetin has been discontinued due to severe side effects, in particular nephrotoxicity (“phenacetin nephritis”).
* Phenacetin has been discontinued due to severe side effects, in particular nephrotoxicity (“phenacetin nephritis”).
It should be noted that the effectiveness and safety of the use of drugs (listed in Table 5-1) that have active metabolites depend not only on the pharmacokinetics of the drug itself, but also on the pharmacokinetics of their active metabolites.
5.1. PRODRUGS
One of the goals of creating prodrugs is to improve pharmacokinetic properties; this accelerates and increases the absorption of substances. Thus, ampicillin esters (pivampicin p, talampicin p and bicampicin p) were developed, which, unlike ampicillin, are almost completely absorbed when taken orally (98-99%). In the liver, these drugs are hydrolyzed by carboxylesterases to ampicillin, which has antibacterial activity.
The bioavailability of the antiviral drug valacyclovir is 54%; it is converted into acyclovir in the liver. It should be noted that the bioavailability of acyclovir itself does not exceed 20%. The high bioavailability of valacyclovir is due to the presence of the amino acid valine residue in its molecule. That is why valacyclovir is absorbed in the intestine by active transport using the oligopeptide transporter PEPT 1.
Another example: adenosine-converting enzyme inhibitors containing a carboxyl group (enalapril, perindopril, trandolapril, quinapril, spirapril, ramipril, etc.). Thus, enalapril is absorbed by 60% when taken orally, hydrolyzed in the liver under the influence of carboxylesterases to active enalaprilat. It should be noted: enalaprilat, when administered orally, is absorbed only by 10%.
Another goal of prodrug development is to improve the safety of drugs. For example, scientists created sulindac p - an NSAID. This drug does not initially block prostaglandin synthesis. Only in the liver does sulindac p hydrolyze to form active sulindac p sulfide (it is this substance that has anti-inflammatory activity). It was assumed that sulindac p would not have an ulcerogenic effect. However, the ulcerogenicity of NSAIDs is due not to local, but to “systemic” action, therefore, as studies have shown, the incidence of erosive and ulcerative lesions of the digestive organs when taking sulindac p and other NSAIDs is approximately the same.
Another goal of creating prodrugs is to increase the selectivity of the action of drugs; this increases the effectiveness and safety of drugs. Dopamine is used to increase renal blood flow in acute renal failure, but the drug affects the myocardium and blood vessels. An increase in blood pressure, the development of tachycardia and arrhythmias are noted. The addition of a glutamic acid residue to dopamine made it possible to create a new drug - glutamyl-dopa p. Glutamyl-dopa p is hydrolyzed to dopamine only in the kidneys under the influence of glutamyl transpeptidase and L-aromatic amino acid decarboxylase and thus has virtually no undesirable effects on central hemodynamics.
 Rice. 5-1. Phases of drug biotransformation (Katzung V., 1998)
Rice. 5-1. Phases of drug biotransformation (Katzung V., 1998)
5.2. PHASES OF DRUG BIOTRANSFORMATION
The biotransformation processes of most drugs occur in the liver. However, the biotransformation of drugs can also occur in other organs, for example, in the digestive tract, lungs, and kidneys.
In general, all drug biotransformation reactions can be classified into one of two categories, designated as biotransformation phase I and biotransformation phase II.
Phase I reactions (non-synthetic reactions)
During non-synthetic reactions, drugs transform into compounds that are more polar and better soluble in water (hydrophilic) than the original substance. Changes in the initial physicochemical properties of drugs are caused by the addition or release of active functional groups: for example, hydroxyl (-OH), sulfhydryl (-SH), amino groups (-NH 2). The main reactions of phase I are oxidation reactions. Hydroxylation is the most common oxidation reaction - the addition of a hydroxyl radical (-OH). Thus, we can assume that in phase I of biotransformation, “breaking” of the drug molecule occurs (Table 5-3). The catalysts for these reactions are enzymes called “mixed-function oxidases.” In general, the substrate specificity of these enzymes is very low, so they oxidize various drugs. Other, less frequent phase I reactions include the processes of reduction and hydrolysis.
Phase II reactions (synthetic reactions)
Phase II biotransformation reactions, or synthetic reactions, represent the combination (conjugation) of a drug and/or its metabolites with endogenous substances, resulting in the formation of polar, highly water-soluble conjugates that are easily excreted by the kidneys or bile. To enter into a phase II reaction, the molecule must have a chemically active radical (group) to which a conjugating molecule can attach. If active radicals are present in the drug molecule initially, then the conjugation reaction proceeds bypassing the phase I reactions. Sometimes a drug molecule acquires active radicals during phase I reactions (Table 5-4).
Table 5-3. Phase I reactions (Katzung 1998; with additions)
 Table 5-4. Phase II reactions (Katzung 1998; with additions)
Table 5-4. Phase II reactions (Katzung 1998; with additions)
 It should be noted that the drug during the biotransformation process can be converted only due to phase I reactions, or exclusively due to phase II reactions. Sometimes part of the drug is metabolized through phase I reactions, and part - through phase II reactions. In addition, there is the possibility of sequential passage of phase I and phase II reactions (Fig. 5-2).
It should be noted that the drug during the biotransformation process can be converted only due to phase I reactions, or exclusively due to phase II reactions. Sometimes part of the drug is metabolized through phase I reactions, and part - through phase II reactions. In addition, there is the possibility of sequential passage of phase I and phase II reactions (Fig. 5-2).
 Rice. 5-2. Functioning of the mixed-function oxidase system
Rice. 5-2. Functioning of the mixed-function oxidase system
Liver first pass effect
The biotransformation of most drugs occurs in the liver. Drugs whose metabolism occurs in the liver are divided into two subgroups: substances with high hepatic clearance and substances with low hepatic clearance.
Drugs with high hepatic clearance are characterized by a high degree of extraction (extraction) from the blood, which is due to the significant activity (capacity) of the enzyme systems that metabolize them (Table 5-5). Since such drugs are quickly and easily metabolized in the liver, their clearance depends on the size and speed of hepatic blood flow.
Drugs with low hepatic clearance. Hepatic clearance does not depend on the speed of hepatic blood flow, but on the activity of enzymes and the degree of binding of drugs to blood proteins.
Table 5-5. Drugs with high hepatic clearance
 With the same capacity of enzyme systems, drugs that are largely bound to proteins (diphenine, quinidine, tolbutamide) will have low clearance compared to drugs that are weakly bound to proteins (theophylline, paracetamol). The capacity of enzyme systems is not a constant value. For example, a decrease in the capacity of enzyme systems is recorded with an increase in the dose of drugs (due to saturation of enzymes); this can lead to an increase in the bioavailability of the drug.
With the same capacity of enzyme systems, drugs that are largely bound to proteins (diphenine, quinidine, tolbutamide) will have low clearance compared to drugs that are weakly bound to proteins (theophylline, paracetamol). The capacity of enzyme systems is not a constant value. For example, a decrease in the capacity of enzyme systems is recorded with an increase in the dose of drugs (due to saturation of enzymes); this can lead to an increase in the bioavailability of the drug.
When drugs with high hepatic clearance are taken orally, they are absorbed in the small intestine and enter the liver through the portal vein system, where they undergo active metabolism (50-80%) even before entering the systemic circulation. This process is known as presystemic elimination, or the first-pass effect. (“first-pass effect”). As a result, such drugs have low bioavailability when taken orally, while their absorption can be almost 100%. The first pass effect is characteristic of drugs such as chlorpromazine, acetylsalicylic acid, vera-
pamil, hydralazine, isoprenaline, imipramine, cortisone, labetolol, lidocaine, morphine. Metoprolol, methyltestosterone, metoclopramide, nortriptyline p, oxprenolol p, organic nitrates, propranolol, reserpine, salicylamide, moracizine (ethmozine) and some other drugs are also subject to presystemic elimination. It should be noted that minor biotransformation of drugs can also occur in other organs (lumen and intestinal wall, lungs, blood plasma, kidneys and other organs).
As studies in recent years have shown, the effect of the first passage through the liver depends not only on the processes of drug biotransformation, but also on the functioning of drug transporters, and, above all, glycoprotein-P and transporters of organic anions and cations (see “The role of drug transporters in pharmacokinetic processes").
5.3. PHASE I ENZYMES OF DRUG BIOTRANSFORMATION
Microsomal system
Many enzymes that metabolize drugs are located on the membranes of the endoplasmic reticulum (ER) of the liver and other tissues. When the ER membranes are isolated by homogenizing and fractionating the cell, the membranes are converted into vesicles called “microsomes.” Microsomes retain most of the morphological and functional characteristics of intact ER membranes, including the property of roughness or smoothness of the surface, respectively, of rough (ribosomal) and smooth (non-ribosomal) ER. While rough microsomes are mainly associated with protein synthesis, smooth microsomes are relatively rich in enzymes responsible for the oxidative metabolism of drugs. In particular, smooth microsomes contain enzymes known as mixed-function oxidases, or monooxygenases. The activity of these enzymes requires the presence of both the reducing agent nicotinamide adenine dinucleotide phosphate (NADPH) and molecular oxygen. In a typical reaction, one molecule of oxygen is consumed (reduced) per molecule of substrate, with one oxygen atom being incorporated into the reaction product and the other forming a water molecule.
Two microsomal enzymes play a key role in this redox process.
Flavoprotein NADPH-H cytochrome P-450 reductase. One mole of this enzyme contains one mole each of flavin mononucleotide and flavin adenine dinucleotide. Since cytochrome C can serve as an electron acceptor, this enzyme is often called NADP-cytochrome C reductase.
Hemoprotein, or cytochrome P-450 performs the function of the final oxidase. In fact, the microsomal membrane contains many forms of this hemoprotein, and this multiplicity increases with repeated administration of xenobiotics. The relative abundance of cytochrome P-450, compared to liver reductase, makes the process of heme reduction by cytochrome P-450 the rate-limiting step in the oxidation of drugs in the liver.
The process of microsomal oxidation of drugs requires the participation of cytochrome P-450, cytochrome P-450 reductase, NADP-H and molecular oxygen. A simplified diagram of the oxidative cycle is shown in the figure (Fig. 5-3). Oxidized (Fe3+) cytochrome P-450 combines with the drug substrate to form a binary complex. NADP-H is an electron donor for flavoprotein reductase, which, in turn, reduces the oxidized cytochrome P-450-drug complex. The second electron passes from NADP-H through the same flavoprotein reductase, which reduces molecular oxygen and forms the “activated oxygen”-cytochrome P-450-substrate complex. This complex transfers "activated oxygen" to the drug substrate to form an oxidized product.
Cytochrome P-450
Cytochrome P-450, often referred to as CYP in the literature, represents a group of enzymes that not only metabolize drugs and other xenobiotics, but also participate in the synthesis of glucocorticoid hormones, bile acids, prostanoids (thromboxane A2, prostacyclin I2), and cholesterol. Cytochrome P-450 was identified for the first time Klingenberg And Garfincell in rat liver microsomes in 1958. Phylogenetic studies have shown that cytochromes P-450 appeared in living organisms about 3.5 billion years ago. Cytochrome P-450 is a hemoprotein: it contains heme. The name cytochrome P-450 is associated with the special properties of this hemoprotein. In restored
In this form, cytochrome P-450 binds carbon monoxide to form a complex with maximum light absorption at a wavelength of 450 nm. This property is explained by the fact that in the heme of cytochrome P-450, iron is bound not only to the nitrogen atoms of the four ligands (while forming a porphyrin ring). There are also fifth and sixth ligands (above and below the heme ring) - the nitrogen atom of histidine and the sulfur atom of cysteine, which are part of the polypeptide chain of the protein part of cytochrome P-450. The largest amount of cytochrome P-450 is located in hepatocytes. However, cytochrome P-450 is also found in other organs: in the intestines, kidneys, lungs, adrenal glands, brain, skin, placenta and myocardium. The most important property of cytochrome P-450 is the ability to metabolize almost all known chemical compounds. The most important reaction is hydroxylation. As already indicated, cytochromes P-450 are also called monooxygenases, since they include one oxygen atom in the substrate, oxidizing it, and one in water, in contrast to dioxygenases, which include both oxygen atoms in the substrate.
Cytochrome P-450 has many isoforms - isoenzymes. Currently, more than 1000 cytochrome P-450 isoenzymes have been identified. Cytochrome P-450 isoenzymes, according to classification Nebert(1987), it is customary to divide nucleotide/amino acid sequences into families according to the proximity (homology) of the nucleotide/amino acid sequence. In turn, families are divided into subfamilies. Cytochrome P-450 isoenzymes with amino acid composition identity of more than 40% are grouped into families (36 families have been identified, 12 of them are found in mammals). Cytochrome P-450 isoenzymes with amino acid composition identity of more than 55% are grouped into subfamilies (39 subfamilies are identified). Families of cytochromes P-450 are usually designated by Roman numerals, subfamilies by Roman numerals and a Latin letter.
Scheme of designation of individual isoenzymes.
The first character (at the beginning) is an Arabic numeral indicating the family.
The second symbol is a Latin letter indicating the subfamily.
At the end (third character) indicate the Arabic numeral corresponding to the isoenzyme.
For example, the cytochrome P-450 isoenzyme designated CYP3A4 belongs to family 3, subfamily IIIA. Cytochrome P-450 isoenzymes are representatives of various families of subfamilies -
differ in activity regulators (inhibitors and inducers) and substrate specificity 1 . For example, CYP2C9 exclusively metabolizes S-warfarin, while R-warfarin is metabolized by CYP1A2 and CYP3A4.
However, members of individual families, subfamilies and individual cytochrome P-450 isoenzymes may have cross-substrate specificity, as well as cross-inhibitors and inducers. For example, ritonavir (an antiviral drug) is metabolized by 7 isoenzymes belonging to different families and subfamilies (CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4). Cimetidine simultaneously inhibits 4 isoenzymes: CYP1A2, CYP2C9, CYP2D6 and CYP3A4. Cytochrome P-450 isoenzymes of families I, II and III take part in the metabolism of drugs. CYP1A1, CYP1A2, CYP2A6, CYP2B6, CYP2D6, CYP2C9, CYP209, CYP2E1, CYP3A4 are the most important and well-studied isoenzymes of cytochrome P-450 for the metabolism of drugs. The content of various cytochrome P-450 isoenzymes in the human liver, as well as their contribution to the oxidation of drugs, are different (Table 5-6). Medicinal substances - substrates, inhibitors and inducers of cytochrome P-450 isoenzymes are presented in Appendix 1.
Table 5-6. The content of cytochrome P-450 isoenzymes in human liver and their contribution to the oxidation of drugs (Lewis et al., 1999)
 1 Some cytochrome P-450 isoenzymes have not only substrate specificity, but also stereospecificity.
1 Some cytochrome P-450 isoenzymes have not only substrate specificity, but also stereospecificity.
Endogenous substrates for isoenzymes of the CYPI family are still unknown. These isoenzymes metabolize xenobiotics: some drugs and PAHs - the main components of tobacco smoke and products of fossil fuel combustion. A distinctive feature of the CYPI family isoenzymes is their ability to be induced by PAHs, including dioxin and 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD). Therefore, the CYPI family is called “cytochrome, inducible PAH” in the literature; “dioxin-inducible cytochrome” or “TCDD-inducible cytochrome”. In the human body, the CYPI family is represented by two subfamilies: IA and IB. The IA subfamily includes isoenzymes 1A1 and 1A2. The IB subfamily includes isoenzyme 1B1.
Cytochrome P-450 isoenzyme 1A1 (CYP1A1) is found mainly in the lungs, and to a lesser extent in lymphocytes and the placenta. CYP1A1 is not involved in drug metabolism, but in the lungs this isoenzyme actively metabolizes PAHs. At the same time, some PAHs, for example, benzopyrene and nitrosamines, turn into carcinogenic compounds that can provoke the development of malignant neoplasms, primarily lung cancer. This process is called “biological activation of carcinogens.” Like other cytochromes of the CYPI family, CYP1A1 is induced by PAHs. At the same time, the mechanism of CYP1A1 induction under the influence of PAHs was studied. Having penetrated the cell, PAHs bind to the Ah receptor (a protein from the class of transcription regulators); the resulting PAH-Ap receptor complex enters the nucleus with the help of another protein, ARNT, and then stimulates the expression of the CYP1A1 gene by binding to a specific dioxin-sensitive region (site) of the gene. Thus, in people who smoke, the induction processes of CYP1A1 are most intense; this leads to biological activation of carcinogens. This explains the high risk of lung cancer in smokers.
Cytochrome P-450 isoenzyme 1A2 (CYP1A2) is found primarily in the liver. Unlike cytochrome CYP1A1, CYP1A2 metabolizes not only PAHs, but also a number of drugs (theophylline, caffeine and other drugs). Phenacetin, caffeine, and antipyrine are used as marker substrates for CYP1A2 phenotyping. In this case, phenacetin is subjected to O-demethylation, caffeine - 3-demethylation, and antipyrine - 4-hydroxylation. Grade
caffeine clearance is an important diagnostic test to determine the functional state of the liver. Due to the fact that CYP1A2 is the main metabolizing enzyme of caffeine, in essence, this test determines the activity of this isoenzyme. The patient is asked to ingest caffeine labeled with the radioactive carbon isotope C 13 (C 13 -caffeine), then the air exhaled by the patient is collected in a special reservoir for an hour and analyzed. In this case, the air exhaled by the patient contains radioactive carbon dioxide (C 13 O 2 - formed by radioactive carbon) and ordinary carbon dioxide (C 12 O 2). The clearance of caffeine is determined by the ratio of C 13 O 2 to C 12 O 2 in exhaled air (measured using mass spectroscopy). There is a modification of this test: using high-performance liquid chromatography, the concentration of caffeine and its metabolites in blood plasma, urine and saliva taken on an empty stomach is determined. In this case, cytochromes CYP3A4 and CYP2D6 make a certain contribution to the metabolism of caffeine. Assessment of caffeine clearance is a reliable test that allows you to assess the functional state of the liver in case of severe damage (for example, with cirrhosis of the liver) and determine the degree of impairment. The disadvantages of the test include its lack of sensitivity in cases of moderate liver damage. The test result is affected by smoking (CYP1A2 induction), age, and concomitant use of drugs that alter the activity of cytochrome P-450 isoenzymes (inhibitors or inducers).
Cytochrome P-450 subfamily CYPIIA
Of the isoenzymes of the CYPIIA subfamily, the most important role in drug metabolism is played by the cytochrome P-450 2A6 isoenzyme (CYP2A6). A common property of isoenzymes of the CYPIIA subfamily is the ability to be inducible under the influence of phenobarbital, therefore the CYPIIA subfamily is called phenobarbital-inducible cytochromes.
Cytochrome P-450 isoenzyme 2A6 (CYP2A6) is found mainly in the liver. CYP2A6 metabolizes a small number of drugs. With the help of this isoenzyme, nicotine is converted into cotinine, as well as cotinine into 3-hydroxycotinine; 7-hydroxylation of coumarin; 7-hydroxylation of cyclophosphamide. CYP2A6 makes a significant contribution to the metabolism of ritonavir, paracetamol and valproic acid. CYP2A6 is involved in the biological activation of nitrosamine components of tobacco smoke, carcinogens that cause lung cancer. CYP2A6 promotes bioactivation
powerful mutagens: 6-amino-(x)-risene and 2-amino-3-methylmidazo-(4,5-f)-quanoline.
Cytochrome P450 subfamily CYPIIB
Of the isoenzymes of the CYPIIB subfamily, the most important role in drug metabolism is played by the CYP2B6 isoenzyme. A common property of isoenzymes of the CYPIIB subfamily is the ability to be induced by phenobarbital.
The cytochrome P-450 2B6 isoenzyme (CYP2B6) is involved in the metabolism of a small number of drugs (cyclophosphamide, tamoxifen, S-methadone p, bupropion p, efavirenz). CYP2B6 primarily metabolizes xenobiotics. The marker substrate for CYP2B6 is an anticonvulsant.
S-mephenytoin p in this case, CYP2B6 subjects S-mephenytoin p to N-demethylation (the determined metabolite is N-demethylmephenytoin). CYP2B6 takes part in the metabolism of endogenous steroids: it catalyzes 16α-16β-hydroxylation of testosterone.
Cytochrome P-450 subfamily CYPIIU
Of all the isoenzymes of the cytochrome CYPIIC subfamily, the most important role in the metabolism of drugs is played by the isoenzymes of cytochrome P-450 2C8, 2C9, 2C19. A common property of cytochromes of the CYPIIC subfamily is 4-hydroxylase activity in relation to mephenytoin p (an anticonvulsant drug). Mephenytoin p is a marker substrate of isoenzymes of the CYPIIC subfamily. That is why isoenzymes of the CYPIIC subfamily are also called mephenytoin-4-hydroxylases.
The cytochrome P-450 2C8 isoenzyme (CYP2C8) is involved in the metabolism of a number of drugs (NSAIDs, statins and other drugs). For many drugs, CYP2C8 is an “alternative” biotransformation pathway. However, for drugs such as repaglinide (a hypoglycemic drug taken orally) and taxol (cytostatic), CYP2C8 is the main metabolic enzyme. CYP2C8 catalyzes the 6a-hydroxylation reaction of taxol. The marker substrate of CYP2C8 is paclitaxel (cytostatic drug). During the interaction of paclitaxel with CYP2C8, 6-hydroxylation of the cytostatic occurs.
Cytochrome P-450 2C9 isoenzyme (CYP2C9) is found mainly in the liver. CYP2C9 is absent from the fetal liver and is not detected until one month after birth. The activity of CYP2C9 does not change throughout life. CYP2C9 metabolizes various drugs. CYP2C9 is the main metabolic enzyme
many NSAIDs, including selective cyclooxygenase-2 inhibitors, angiotensin receptor inhibitors (losartan and irbesartan), hypoglycemic drugs (sulfonylurea derivatives), phenytoin (diphenin ♠), indirect anticoagulants (warfarin 1, acenocoumarol 2), fluvastatin 3.
It should be noted that CYP2C9 has “stereoselectivity” and metabolizes mainly S-warfarin and S-acenocoumarol, while the biotransformation of R-warfarin and R-acenocoumarol occurs with the help of other cytochrome P-450 isoenzymes: CYP1A2, CYP3A4. Inducers of CYP2C9 are rifampicin and barbiturates. It should be noted that almost all sulfonamide antibacterial drugs inhibit CYP2C9. However, a specific inhibitor of CYP2C9 was discovered - sulfafenazole r. There is evidence that Echinacea purpurea extract inhibits CYP2C9 in studies in vitro And in vivo, and hydrolyzed soy extract (due to the isoflavones it contains) inhibits this isoenzyme in vitro. The combined use of CYP2C9 drug substrates with its inhibitors leads to inhibition of the metabolism of substrates. As a result, undesirable drug reactions of CYP2C9 substrates may occur (including intoxication). For example, the combined use of warfarin (a CYP2C9 substrate) with sulfonamide drugs (CYP2C9 inhibitors) increases the anticoagulant effect of warfarin. That is why, when combining warfarin with sulfonamides, it is recommended to strictly (at least 1-2 times a week) monitor the international normalized ratio. CYP2C9 has genetic polymorphism. “Slow” allelic variants of CYP2C9*2 and CYP2C9*3 are single-nucleotide polymorphisms of the CYP2C9 gene that have been most fully studied at present. In carriers of allelic variants CYP2C9*2 and CYP2C9*3, a decrease in CYP2C9 activity is noted; this leads to a decrease in the rate of biotransformation of drugs metabolized by this isoenzyme and to an increase in their concentration in plasma
1 Warfarin is a racematic mixture of isomers: S-warfarin and R-wafrarin. It should be noted that S-warfarin has greater anticoagulant activity.
2 Acenocoumarol is a racematic mixture of isomers: S-acenocoumarol and R-acenocoumarol. However, unlike warfarin, these two isomers have the same anticoagulant activity.
3 Fluvastatin is the only drug from the group of lipid-lowering drugs HMG-CoA reductase inhibitors, the metabolism of which occurs with the participation of CYP2C9, and not CYP3A4. In this case, CYP2C9 metabolizes both isomers of fluvastatin: the active (+)-3R,5S enantiomer and the inactive (-)-3S,5R enantiomer.
blood. Therefore, heterozygotes (CYP2C9*1/*2, CYP2C9*1/*3) and homozygotes (CYP2C9*2/*2, CYP2C9*3/*3, CYP2C9*2/*3) are “slow” metabolizers of CYP2C9. Thus, it is in this category of patients (carriers of the listed allelic variants of the CYP2C9 gene) that adverse drug reactions are most often observed when using drugs whose metabolism occurs under the influence of CYP2C9 (indirect anticoagulants, NSAIDs, hypoglycemic drugs used orally - sulfonylurea derivatives).
Cytochrome P-450 isoenzyme 2C18 (CYP2C18) is found mainly in the liver. CYP2Cl8 is absent from the fetal liver and is not detected until one month after birth. CYP2Cl8 activity does not change throughout life. CYP2Cl8 makes a certain contribution to the metabolism of drugs such as naproxen, omeprazole, piroxicam, propranolol, isotretinoin (retinoic acid) and warfarin.
Cytochrome P-450 isoenzyme 2C19 (CYP2C19) is the main enzyme in the metabolism of proton pump inhibitors. At the same time, the metabolism of individual drugs from the group of proton pump inhibitors has its own characteristics. Thus, two metabolic pathways were discovered for omeprazole.
Omeprazole is converted to hydroxyomeprazole by CYP2C19. Under the influence of CYP3A4, hydroxyomeprazole is converted to omeprazole hydroxysulfone.
Under the influence of CYP3A4, omeprazole is converted to omeprazole sulfide and omeprazole sulfone. Under the influence of CYP2C19, omeprazole sulfide and omeprazole sulfone are converted to omeprazole hydroxysulfone.
Thus, regardless of the route of biological transformation, the final metabolite of omeprazole is omeprazole hydroxysulfone. However, it should be noted that these metabolic pathways are characteristic primarily of the R-isomer of omeprazole (the S-isomer undergoes biotransformation to a much lesser extent). Understanding this phenomenon made it possible to create esoprazole r, a drug representing the S-isomer of omeprazole (inhibitors and inducers of CYP2C19, as well as genetic polymorphism of this isoenzyme, have a lesser effect on the pharmacokinetics of esoprazole r).
The metabolism of lansoprazole is identical to that of omeprazole. Rabeprazole is metabolized by CYP2C19 and CYP3A4 to dimethylrabeprazole and rabeprazole sulfone, respectively.
CYP2C19 is involved in the metabolism of tamoxifen, phenytoin, ticlopidine, and psychotropic drugs such as tricyclic antidepressants, diazepam, and some barbiturates.
CYP2C19 is characterized by genetic polymorphism. Slow metabolizers of CYP2Cl9 are carriers of “slow” allelic variants. The use of drugs that are substrates of this isoenzyme in slow metabolizers of CYP2CL9 leads to a more frequent occurrence of adverse drug reactions, especially when using drugs with a narrow therapeutic scope: tricyclic antidepressants, diazepam, some barbiturates (mephobarbital, hexobarbital). However, the largest number of studies are devoted to the effect of polymorphism of the CYP2C19 gene on the pharmacokinetics and pharmacodynamics of proton pump inhibitor blockers. As shown by pharmacokinetic studies conducted with the participation of healthy volunteers, the area under the pharmacokinetic curve, the values of the maximum concentration of omeprazole, lansoprazole and rabeprazole are significantly higher in heterozygotes and, especially, in homozygotes for “slow” allelic variants of the CYP2C19 gene. In addition, a more pronounced suppression of gastric secretion when using omeprazole, lansorprazole, rabeprazole was observed in patients (heterozygotes and homozygotes for “slow” allelic variants of CYP2C19) suffering from peptic ulcer and reflux esophagitis. However, the frequency of adverse drug reactions of proton pump inhibitors does not depend on the CYP2C19 genotype. Existing data suggest that to achieve “targeted” suppression of gastric secretion in heterozygotes and homozygotes for “slow” allelic variants of the CYP2C19 gene, lower doses of proton pump inhibitors are required.
Cytochrome P-450 subfamily CYPIID
The cytochrome P-450 CYPIID subfamily includes a single isoenzyme - 2D6 (CYP2D6).
Cytochrome P-450 isoenzyme 2D6 (CYP2D6) is found mainly in the liver. CYP2D6 metabolizes about 20% of all known drugs, including antipsychotics, antidepressants, tranquilizers, and β-blockers. It has been proven: CYP2D6 is the main enzyme for the biotransformation of the tricyclic antidepressant amitriptyline. However, as studies have shown, a small part of amitriptyline is metabolized by other isoenzymes of cytochrome P-450 (CYP2C19, CYP2C9, CYP3A4) to inactive metabolites. Debrisoquine p, dextromethorphan and sparteine are marker substrates used for phenotyping the 2D6 isoenzyme. CYP2D6, unlike other cytochrome P-450 isoenzymes, does not have inducers.
The CYP2D6 gene has polymorphism. Back in 1977, Iddle and Mahgoub drew attention to the difference in the hypotensive effect in patients with arterial hypertension who used debrisoquine p (a drug from the group of α-blockers). At the same time, they formulated an assumption about the difference in the rate of metabolism (hydroxylation) of debrisoquine p in different individuals. In “slow” metabolizers of debrisoquine, the greatest severity of the hypotensive effect of this drug was recorded. Later, it was proven that “slow” metabolizers of debrisoquine β also have slow metabolism of some other drugs, including phenacetin, nortriptyline β, phenformin β, sparteine, encainide β, propranolol, guanoxane β and amitriptyline. As further studies have shown, “slow” CYP2D6 metabolizers are carriers (both homozygotes and heterozygotes) of functionally defective allelic variants of the CYP2D6 gene. The result of these options is the absence of synthesis of CYP2D6 (allelic variant CYP2D6x5), synthesis of inactive protein (allelic variants CYP2D6x3, CYP2D6x4, CYP2D6x6, CYP2D6x7, CYP2D6x8, CYP2D6x11, CYP2D6x12, CYP2D6x14, CYP2D6x15, CYP2D6x19, CYP2D6x20), synthesis of a defective protein with reduced activity yu (options CYP2D6x9, CYP2D6x10, CYP2D6x17,
CYP2D6x18, CYP2D6x36). Every year the number of found allelic variants of the CYP2D6 gene is growing (their carriage leads to changes in the activity of CYP2D6). However, Saxena (1994) pointed out that 95% of all “slow” metabolizers of CYP2D6 are carriers of the CYP2D6x3, CYP2D6x4, CYP2D6x5 variants; other variants are found much less frequently. According to Rau et al. (2004), the frequency of the CYP2D6x4 allelic variant among patients who experienced adverse drug reactions while taking tricyclic antidepressants (arterial hypotension, sedation, tremor, cardiotoxicity) is almost 3 times (20%) higher than that in patients whose treatment No complications were recorded with these drugs (7%). A similar effect of genetic polymorphism of CYP2D6 was found on the pharmacokinetics and pharmacodynamics of antipsychotics, as a result of which they demonstrated the presence of associations between the carriage of certain allelic variants of the CYP2D6 gene and the development of extrapyramidal disorders induced by antipsychotics.
However, carriage of “slow” allelic variants of the CYP2D6 gene may be accompanied not only by an increased risk of developing adverse drug reactions when using the drug;
rats metabolized by this isoenzyme. If a drug is a prodrug, and the active metabolite is formed precisely under the influence of CYP2D6, then low effectiveness of the drug is noted in carriers of “slow” allelic variants. Thus, in carriers of “slow” allelic variants of the CYP2D6 gene, a less pronounced analgesic effect of codeine is recorded. This phenomenon is explained by a decrease in O-demethylation of codeine (during this process, morphine is formed). The analgesic effect of tramadol is also due to the active metabolite O-demethyltramadol (formed by the action of CYP2D6). In carriers of “slow” allelic variants of the CYP2D6 gene, a significant decrease in the synthesis of O-demethyltramadol is noted; this may lead to insufficient analgesic effect (similar to the processes that occur when using codeine). Thus, Stamer et al. (2003), having studied the analgesic effect of tramadol in 300 patients who had undergone abdominal surgery, found that homozygotes for “slow” allelic variants of the CYP2D6 gene did not “respond” to tramadol therapy 2 times more often than patients who did not carry these alleles ( 46.7% versus 21.6%, respectively, p=0.005).
Currently, many studies have been carried out on the effect of genetic polymorphism of CYP2D6 on the pharmacokinetics and pharmacodynamics of β-blockers. The results of these studies have clinical significance for the individualization of pharmacotherapy for this group of drugs.
Cytochrome P-450 subfamily CYPIIB
Of the isoenzymes of the cytochrome IIE subfamily, the most important role in drug metabolism is played by the cytochrome P-450 2E1 isoenzyme. A common property of isoenzymes of the CYPIIE subfamily is the ability to induce under the influence of ethanol. That is why the second name of the CYPIIE subfamily is ethanol-inducible cytochromes.
Cytochrome P-450 isoenzyme 2E1 (CYP2E1) is found in the liver of adults. CYP2E1 accounts for about 7% of all cytochrome P-450 isoenzymes. CYP2E1 substrates are a small amount of drugs, as well as some other xenobiotics: ethanol, nitrosamines, “small” aromatic hydrocarbons such as benzene and aniline, aliphatic chlorocarbons. CYP2E1 catalyzes the conversion of dapsone to hydroxylamindapsone, n1-demethylation and N7-demethylation of caffeine, dehalogenation of chlorofluorocarbons and inhalational anesthetics (halothane), and several other reactions.
CYP2E1, together with CYP1A2, catalyze an important reaction that converts paracetamol (acetaminophen) to N-acetylbenzoquinoneimine, which has a potent hepatotoxic effect. There is evidence of the participation of cytochrome CYP2E1 in vaterogenesis. For example, it is known that CYP2E1 is the most important cytochrome P-450 isoenzyme that oxidizes low-density lipoprotein (LDL) cholesterol. Cytochromes and other cytochrome P-450 isoenzymes, as well as 15-lipoxygenase and NADPH-oxidases, also take part in the oxidation of LDL. Oxidation products: 7a-hydroxycholesterol, 7β-hydroxycholesterol, 5β-6β-epoxycholesterol, 5α-6β-epoxycholesterol, 7-ketocholesterol, 26-hydroxycholesterol. The process of LDL oxidation occurs in endothelial cells, smooth muscles of blood vessels, and macrophages. Oxidized LDL stimulates the formation of foam cells and thus contributes to the formation of atherosclerotic plaques.
Cytochrome P-450 subfamily CYPIIIA
The cytochrome P-450 subfamily CYPIIIA includes four isoenzymes: 3A3, 3A4, 3A5 and 3A7. Cytochromes of subfamily IIIA constitute 30% of all cytochrome P-450 isoenzymes in the liver and 70% of all isoenzymes in the wall of the digestive tract. At the same time, isoenzyme 3A4 (CYP3A4) is predominantly localized in the liver, and isoenzymes 3A3 (CYP3A3) and 3A5 (CYP3A5) are localized in the walls of the stomach and intestines. Isoenzyme 3A7 (CYP3A7) is found only in the fetal liver. Of the isoenzymes of the IIIA subfamily, CYP3A4 plays the most important role in drug metabolism.
The cytochrome P-450 3A4 isoenzyme (CYP3A4) metabolizes about 60% of all known drugs, including slow calcium channel blockers, macrolide antibiotics, some antiarrhythmics, statins (lovastatin, simvastatin, atorvastatin), clopidogrel 1 and other drugs.
CYP3A4 catalyzes the 6β-hydroxylation reaction of endogenous steroids, including testosterone, progesterone, and cortisol p. Marker substrates for determining CYP3A4 activity are dapsone, erythromycin, nifedipine, lidocaine, testosterone and cortisol p.
Metabolism of lidocaine occurs in hepatocytes, where monoethylglycine xylidide (MEGX) is formed through oxidative N-deethylation of CYP3A4.
1 Clopidogrel is a prodrug; under the influence of CYP3A4 it is converted into an active metabolite with an antiplatelet effect.
Determination of CYP3A4 activity by MEGX (lidocaine metabolite) is the most sensitive and specific test that allows you to assess the functional state of the liver in acute and chronic liver diseases, as well as in systemic inflammatory response syndrome (sepsis). In liver cirrhosis, MEGX concentration correlates with disease prognosis.
There is data in the literature on intraspecific variability in drug metabolism under the influence of CYP3A4. However, molecular evidence for CYP3A4 genetic polymorphisms has only recently emerged. Thus, A. Lemoin et al. (1996) described a case of intoxication with tacrolimus (a CYP3A4 substrate) in a patient after a liver transplant (CYP3A4 activity could not be detected in liver cells). Only after treatment of transplanted liver cells with glucocorticoids (CYP3A4 inducers) can CYP3A4 activity be determined. There is an assumption that disruption of the expression of transcription factors of the gene encoding CYP3A4 is the cause of variability in the metabolism of this cytochrome.
The cytochrome P-450 3A5 isoenzyme (CYP3A5), according to recent data, may play a significant role in the metabolism of certain drugs. It should be noted that CYP3A5 is expressed in the liver of 10-30% of adults. In these individuals, the contribution of CYP3A5 to the activity of all isoenzymes of the IIIA subfamily ranges from 33 (in Europeans) to 60% (in African Americans). As studies have shown, under the influence of CYP3A5, the processes of biotransformation of those drugs that are traditionally considered as substrates of CYP3A4 occur. It should be noted that inducers and inhibitors of CYP3A4 have similar effects on CYP3A5. CYP3A5 activity varies more than 30-fold between individuals. Differences in CYP3A5 activity were first described by Paulussen et al. (2000): they observed in vitro significant differences in the rate of metabolism of midazolam under the influence of CYP3A5.
Dihydropyrimidine dehydrogenase
The physiological function of dihydropyrimidine dehydrogenase (DPDH) is the reduction of uracil and thymidine - the first reaction of the three-step metabolism of these compounds to β-alanine. In addition, EMDR is the main enzyme that metabolizes 5-fluorouracil. This drug is used as part of combination chemotherapy for cancer of the breast, ovaries, esophagus, stomach, colon and rectum, liver, cervix, vulva. Also
5-fluorouracil is used in the treatment of cancer of the bladder, prostate, tumors of the head, neck, salivary glands, adrenal glands, and pancreas. Currently, the amino acid sequence and number of amino acid residues (there are 1025 in total) that make up EMDR are known; The molecular weight of the enzyme is 111 kDa. The EMDR gene, located on chromosome 1 (locus 1p22), was identified. The cytoplasm of cells of various tissues and organs contains EMPG; especially large amounts of the enzyme are found in liver cells, monocytes, lymphocytes, granulocytes, and platelets. However, EMDR activity has not been observed in erythrocytes (Van Kuilenburg et al., 1999). Since the mid-80s, there have been reports of serious complications arising from the use of 5-fluorouracil (the cause of complications is the hereditary low activity of EMDR). As shown by Diasio et al. (1988), low EMDR activity is inherited in an autosomal recessive manner. Thus, EMPG is an enzyme with genetic polymorphism. In the future, it is likely that EMDR phenotyping and genotyping methods will be introduced into oncological practice to ensure the safety of chemotherapy with 5-fluorouracil.
5.4. PHASE II ENZYMES OF DRUG BIOTRANSFORMATION
Glucuronyltransferases
Glucuronidation is the most important phase II reaction of drug metabolism. Glucuronidation is the addition (conjugation) of uridine diphosphate-glucuronic acid (UDP-glucuronic acid) to a substrate. This reaction is catalyzed by a superfamily of enzymes called "UDP-glucuronyltransferases" and referred to as UGT. The UDP-glucuronyltransferase superfamily includes two families and more than twenty isoenzymes localized in the endoplasmic system of cells. They catalyze the glucuronidation of a large number of xenobiotics, including drugs and their metabolites, pesticides and carcinogens. Compounds that undergo glucuronidation include ethers and esters; compounds containing carboxyl, carbamoyl, thiol and carbonyl groups, as well as nitro groups. Glucuronidation
leads to an increase in the polarity of chemical compounds, which facilitates their solubility in water and elimination. UDP-glucuronyltransferases are found in all vertebrates: from fish to humans. In the body of newborns, low activity of UDP-glucuronyltransferases is recorded, but after 1-3 months of life, the activity of these enzymes can be compared with that in adults. UDP-glucuronyltransferases are found in the liver, intestines, lungs, brain, olfactory epithelium, and kidneys, but the liver is the main organ in which glucuronidation occurs. The degree of expression of various UDP-glucuronyl transferase isoenzymes in organs varies. Thus, the UDP-glucuronyltransferase isoenzyme UGT1A1, which catalyzes the glucuronidation of bilirubin, is expressed mainly in the liver, but not in the kidneys. The UDP-glucuronyltransferase isoenzymes UGT1A6 and UGT1A9, responsible for the glucuronidation of phenol, are expressed equally in both the liver and kidneys. As mentioned above, based on the identity of the amino acid composition, the superfamily of UDP-glucuronyltransferases is divided into two families: UGT1 and UGT2. Isoenzymes of the UGT1 family are similar in amino acid composition by 62-80%, and isoenzymes of the UGT2 family are 57-93% similar. Isoenzymes that are part of the human UDP-glucuronyltransferase families, as well as the localization of genes and marker substrates of isoenzymes for phenotyping are presented in the table (Table 5-7).
The physiological function of UDP-glucuronyltransferases is glucuronidation of endogenous compounds. The product of heme catabolism, bilirubin, is the most well-studied endogenous substrate of UDP-glucuronyltransferase. Glucuronidation of bilirubin prevents the accumulation of toxic free bilirubin. In this case, bilirubin is excreted in the bile in the form of monoglucuronides and diglucuronides. Another physiological function of UDP-glucuronyltransferase is participation in hormone metabolism. Thus, thyroxine and triiodothyronine undergo glucuronidation in the liver and are excreted in the form of glucuronides in bile. UDP-glucuronyltransferases are also involved in the metabolism of steroid hormones, bile acids, and retinoids, but these reactions are currently insufficiently studied.
Drugs of different classes are subject to glucuronidation, many of them have a narrow therapeutic range, for example, morphine and chloramphenicol (Table 5-8).
Table 5-7. Composition of human UDP-glucuronyltransferase families, gene localization and marker substrates of isoenzymes
 Table 5-8. Medicines, metabolites and xenobiotics subject to glucuronidation by various UDP-glucuronyltransferase isoenzymes
Table 5-8. Medicines, metabolites and xenobiotics subject to glucuronidation by various UDP-glucuronyltransferase isoenzymes
 End of table 5-8
End of table 5-8
 Medicines (representatives of different chemical groups) subject to glucuronidation
Medicines (representatives of different chemical groups) subject to glucuronidation
Phenols: propofol, acetaminophen, naloxone.
Alcohols: chloramphenicol, codeine, oxazepam.
Aliphatic amines: cyclopiroxolamine p, lamotrigine, amitriptyline.
Carboxylic acids: ferpazone p, phenylbutazone, sulfinpyrazone.
Carboxylic acids: naproxen, zomepyral p, ketoprofen. Thus, compounds undergo glucuronidation
containing different functional groups that act as acceptors for UDP-glucuronic acid. As mentioned above, as a result of glucuronidation, polar inactive metabolites are formed that are easily excreted from the body. However, there is an example where glucuronidation results in the formation of an active metabolite. Glucuronidation of morphine leads to the formation of morphine-6-glucuronide, which has a significant analgesic effect and is less likely than morphine to cause nausea and vomiting. Glucuronidation may also contribute to the biological activation of carcinogens. Carcinogenic glucuronides include 4-aminobiphenyl N-glucuronide, N-acetylbenzidine N-glucuronide, and 4-((hydroxymethyl)-nitrosoamino)-1-(3-pyridyl)-1-butanone O-glucuronide.
The existence of hereditary disorders of bilirubin glucuronidation has long been known. These include Gilbert's syndrome and Crigler-Najjar syndrome. Gilbert's syndrome is a hereditary disease inherited in an autosomal recessive manner. The prevalence of Gilbert's syndrome in the population is 1-5%. The cause of the development of this disease is point mutations (usually substitutions in the nucleotide sequence) in the UGT1 gene. In this case, UDP-glucuronyltransferase is formed, which is characterized by low activity (25-30% of the normal level). Changes in the glucuronidation of drugs in patients with Gilbert's syndrome have been little studied. There is evidence of decreased clearance of tolbutamide, paracetamol (acetaminophen ♠) and rifampin p in patients with Gilbert's syndrome. We studied the frequency of side effects of the new cytotoxic drug irinotecan in patients suffering from both colorectal cancer and Gilbert's syndrome and in patients with colorectal cancer. Irinotecan (STR-11) is a new highly effective drug that has a cytostatic effect, inhibits topoisomerase I and is used for colorectal cancer in the presence of resistance to fluorouracil. Irinotecan in the liver, under the action of carboxylesterases, converts
into the active metabolite 7-ethyl-10-hydroxycamptothecin (SN-38). The main metabolic pathway of SN-38 is glucuronidation by UGT1A1. During studies, side effects of irinotecan (in particular, diarrhea) were significantly more often recorded in patients with Gilbert's syndrome. Scientists have proven that carriage of allelic variants UGT1A1x1B, UGT1A1x26, UGT1A1x60 is associated with a more frequent development of hyperbilirubinemia when using irinotecan, while low values of the area under the pharmacokinetic curve of glucuronide SN-38 were recorded. Currently, the US Food and Drug Administration (Food and drug administration- The FDA has approved the determination of allelic variants of the UGT1A1 gene to select irinotecan dosage regimens. There is data on the effect of carriage of allelic variants of genes encoding other isoforms of UGT on the pharmacokinetics and pharmacodynamics of various drugs.
Acetyltransferases
Acetylation represents one of the earliest adaptation mechanisms in evolution. The acetylation reaction is necessary for the synthesis of fatty acids, steroids, and the functioning of the Krebs cycle. An important function of acetylation is the metabolism (biotransformation) of xenobiotics: drugs, household and industrial poisons. Acetylation processes are influenced by N-acetyltransferase, as well as coenzyme A. Control of the intensity of acetylation in the human body occurs with the participation of β 2 -adrenergic receptors and depends on metabolic reserves (pantothenic acid, pyridoxine, thiamine, lipoic acid *) and genotype. In addition, the intensity of acetylation depends on the functional state of the liver and other organs containing N-acetyltransferase (although acetylation, like other phase II reactions, changes little in liver diseases). Meanwhile, acetylation of drugs and other xenobiotics occurs predominantly in the liver. Two N-acetyltransferase isoenzymes have been isolated: N-acetyltransferase 1 (NAT1) and N-acetyltransferase 2 (NAT2). NAT1 acetylates a small number of arylamines and does not exhibit genetic polymorphism. Thus, the main acetylation enzyme is NAT2. The NAT2 gene is located on chromosome 8 (loci 8p23.1, 8p23.2 and 8p23.3). NAT2 acetylates various drugs, including isoniazid and sulfonamides (Table 5-9).
Table 5-9. Medicines subject to acetylation
 The most important property of NAT2 is considered to be genetic polymorphism. The acetylation polymorphism was first described in the 1960s by Evans; he isolated slow and fast acetylators of isoniazid. It was also noted that in “slow” acetylators, due to the accumulation (cumulation) of isoniazid, polyneuritis occurs more often. Thus, in “slow” acetylators, the half-life of isoniazid is 3 hours, while in “fast” acetylators it is 1.5 hours. The development of polyneuritis is due to the influence of isoniazid: the drug inhibits the transition of pyridoxine (vitamin B 6) to the active coenzyme dipyridoxine phosphate, which is necessary for myelin synthesis. It was assumed that in “fast” acetylators, the use of isoniazid is more likely to lead to the development of a hepatotoxic effect due to more intense formation of acetylhydrazine, but this assumption has not received practical confirmation. The individual rate of acetylation does not significantly affect the dosage regimen of the drug when taken daily, but may reduce the effectiveness of therapy with periodic use of isoniazid. After analyzing the results of treatment with isoniazid in 744 patients with tuberculosis, it was found that with “slow” acetylators, the closure of cavities in the lungs occurs faster. As shown by a study conducted by Sunahara in 1963, “slow” acetylators are homozygotes for the “slow” NAT2 allele, and “fast” metabolizers are homozygotes or heterozygotes for the “fast” NAT2 allele. In 1964, Evans published data showing that acetylation polymorphism is characteristic not only of isoniazid, but also of hydralazine and sulfonamides. Then the presence of polymorphism of acetyl-
The most important property of NAT2 is considered to be genetic polymorphism. The acetylation polymorphism was first described in the 1960s by Evans; he isolated slow and fast acetylators of isoniazid. It was also noted that in “slow” acetylators, due to the accumulation (cumulation) of isoniazid, polyneuritis occurs more often. Thus, in “slow” acetylators, the half-life of isoniazid is 3 hours, while in “fast” acetylators it is 1.5 hours. The development of polyneuritis is due to the influence of isoniazid: the drug inhibits the transition of pyridoxine (vitamin B 6) to the active coenzyme dipyridoxine phosphate, which is necessary for myelin synthesis. It was assumed that in “fast” acetylators, the use of isoniazid is more likely to lead to the development of a hepatotoxic effect due to more intense formation of acetylhydrazine, but this assumption has not received practical confirmation. The individual rate of acetylation does not significantly affect the dosage regimen of the drug when taken daily, but may reduce the effectiveness of therapy with periodic use of isoniazid. After analyzing the results of treatment with isoniazid in 744 patients with tuberculosis, it was found that with “slow” acetylators, the closure of cavities in the lungs occurs faster. As shown by a study conducted by Sunahara in 1963, “slow” acetylators are homozygotes for the “slow” NAT2 allele, and “fast” metabolizers are homozygotes or heterozygotes for the “fast” NAT2 allele. In 1964, Evans published data showing that acetylation polymorphism is characteristic not only of isoniazid, but also of hydralazine and sulfonamides. Then the presence of polymorphism of acetyl-
The results have also been proven for other drugs. The use of procainamide and hydralazine in “slow” acetylators much more often causes liver damage (hepatotoxicity), thus, these drugs are also characterized by acetylation polymorphism. However, in the case of dapsone (also subject to acetylation), it was not possible to detect differences in the incidence of lupus-like syndrome when using this drug with “slow” and “fast” acetylators. The prevalence of “slow” acetylators varies: from 10-15% among Japanese and Chinese to 50% among Caucasians. Only in the late 80s did they begin to identify allelic variants of the NAT2 gene, the carriage of which causes slow acetylation. Currently, about 20 mutant alleles of the NAT2 gene are known. All of these allelic variants are inherited in an autosomal recessive manner.
The type of acetylation is determined using NAT2 phenotyping and genotyping methods. Dapsone, isoniazid and sulfadimine (sulfadimezine *) are used as marker substrates for acetylation. The ratio of the concentration of monoacetyldapsone to the concentration of dapsone in the blood plasma of less than 0.35 6 hours after administration of the drug is typical for “slow” acetylators, and more than 0.35 for “fast” acetylators. If sulfadimine is used as a marker substrate, then the presence of less than 25% of sulfadimine in blood plasma (analysis performed after 6 hours) and less than 70% in urine (collected 5-6 hours after drug administration) indicates a “slow” acetylation phenotype.
Thiopurine S-methyltransferase
Thiopurine S-methyltransferase (TPMT) is an enzyme that catalyzes the reaction of S-methylation of thiopurine derivatives - the main metabolic pathway for cytostatic substances from the group of purine antagonists: 6-mercaptopurine, 6-thioguanine, azathioprine. 6-mer-captopurine is used as part of combination chemotherapy for myeloblastic and lymphoblastic leukemia, chronic myeloid leukemia, lymphosarcoma, and soft tissue sarcoma. For acute leukemia, 6-thioguanine is usually used. Currently, the amino acid sequence and the number of amino acid residues that make up TRMT are known - 245. The molecular weight of TRMT is 28 kDa. The TPMT gene, located on chromosome 6 (locus 6q22.3), was also identified. TPMT is located in the cytoplasm of hematopoietic cells.
In 1980, Weinshiboum studied TPMT activity in 298 healthy volunteers and found significant differences in TPMT activity among humans: 88.6% of subjects had high TPMT activity, 11.1% had intermediate activity. Low TPMT activity (or complete absence of enzyme activity) was recorded in 0.3% of the examined volunteers. This is how the genetic polymorphism of TRMT was described for the first time. More recent studies have shown that people with low TPMT activity have increased sensitivity to 6-mercaptopurine, 6-thioguanine, and azathioprine; At the same time, life-threatening hematotoxic (leukopenia, thrombocytopenia, anemia) and hepatotoxic complications develop. Under conditions of low TPMT activity, the metabolism of 6-mercaptopurine proceeds along an alternative pathway - to the highly toxic compound 6-thioguanine nucleotide. Lennard et al. (1990) studied the concentration of 6-thioguanine nucleotide in blood plasma and TPMT activity in the erythrocytes of 95 children who received 6-mercaptopurine for acute lymphoblastic leukemia. The authors found that the lower the activity of TPMT, the higher the concentrations of 6-TGN in the blood plasma and the more pronounced the side effects of 6-mercaptopurine. It has now been proven that low TPMT activity is inherited in an autosomal recessive manner, with homozygotes having low TPMT activity and intermediate activity in heterozygotes. Genetic studies in recent years, carried out using the polymerase chain reaction method, have made it possible to detect mutations in the TPMT gene, which determine the low activity of this enzyme. Safe doses of 6-mercaptopurine: with high TPMT activity (normal genotype) 500 mg/(m 2 × day) is prescribed, with intermediate TPMT activity (heterozygotes) - 400 mg/(m 2 × day), with slow activity TRMT (homozygotes) - 50 mg/(m 2 × day).
Sulfotransferases
Sulfation is the reaction of addition (conjugation) of a sulfuric acid residue to a substrate, resulting in the formation of sulfuric acid esters or sulfomates. Exogenous compounds (mainly phenols) and endogenous compounds (thyroid hormones, catecholamines, some steroid hormones) are subject to sulfation in the human body. 3"-phosphoadenyl sulfate acts as a coenzyme for the sulfation reaction. Then the conversion of 3"-phosphoadenyl sulfate into adenosine-3,5"-bisphosphonate occurs. The sulfation reaction is catalyzed by
a family of enzymes called sulfotransferases (SULTs). Sulfotransferases are localized in the cytosol. Three families have been found in the human body. Currently, about 40 sulfotransferase isoenzymes have been identified. Sulfotransferase isoenzymes in the human body are encoded by at least 10 genes. The greatest role in the sulfation of drugs and their metabolites belongs to sulfotransferase isoenzymes family 1 (SULT1). SULT1A1 and SULT1A3 are the most important isoenzymes of this family. SULT1 isoenzymes are localized mainly in the liver, as well as the large and small intestines, lungs, brain, spleen, placenta, and leukocytes. SULT1 isoenzymes have a molecular weight of about 34 kDa and consist of 295 amino acid residues; the SULT1 isoenzyme gene is localized on chromosome 16 (locus 16p11.2). SULT1A1 (thermostable sulfotransferase) catalyzes the sulfation of “simple phenols”, including drugs with a phenolic structure (minoxidil r, acetaminophen, morphine, salicylamide, isoprenaline and some others). It should be noted that sulfation of minoxidil p leads to the formation of its active metabolite - minoxidil sulfate. SULT1A1 sulfates the metabolites of lidocaine: 4-hydroxy-2,6-xylidine (4-hydroxyl) and ropivacaine: 3-hydroxyropivacaine, 4-hydroxyropivacaine, 2-hydroxymethylropivacaine. In addition, SULT1A1 sulfates 17β-estradiol. The marker substrate of SULT1A1 is 4-nitrophenol. SULT1A3 (heat-labile sulfotransferase) catalyzes the sulfation reactions of phenolic monoamines: dopamine, norepinephrine, serotonin. The marker substrate of SULT1A3 is dopamine. Sulfotransferase isoenzymes family 2 (SULT2) provide sulfation of dihydroepiandrosterone, epiandrosterone, and androsterone. SULT2 isoenzymes are involved in the biological activation of carcinogens, for example, PAHs (5-hydroxymethylchrysene, 7,12-dihydroxymethylbenz[a]anthracene), N-hydroxy-2-acetylaminofluorene. Sulfotransferase family 3 (SULT3) isoenzymes catalyze the N-sulfation of acyclic arylamines.
Epoxide hydrolase
Aqueous conjugation plays an important role in the detoxification and biological activation of a large number of xenobiotics, such as arenes, aliphatic epoxides, PAHs, aflatoxin B1. Aqueous conjugation reactions are catalyzed by a special enzyme - epoxide hydrolase.
(ERNH). The largest amount of this enzyme is found in the liver. Scientists have isolated two isoforms of epoxide hydrolase: ERNX1 and ERNX2. ERNX2 consists of 534 amino acid residues and has a molecular weight of 62 kDa; the ERNX2 gene is located on chromosome 8 (8p21-p12 locus). ERNX2 is localized in the cytoplasm and peroxisomes; this isoform of epoxide hydrolase plays a minor role in the metabolism of xenobiotics. Most aqueous conjugation reactions are catalyzed by ERNX1. ERNX1 consists of 455 amino acid residues and has a molecular weight of 52 kDa. The ERNX1 gene is located on chromosome 1 (locus 1q42.1). ERNX1 is of great importance in the aqueous conjugation of toxic metabolites of drugs. The anticonvulsant phenytoin is oxidized by cytochrome P-450 to two metabolites: parahydroxylate and dihydrodiol. These metabolites are active electrophilic compounds capable of covalently binding to cell macromolecules; this leads to cell death, the formation of mutations, malignancy, and mitotic defects. In addition, parahydroxylate and dihydrodiol, acting as haptens, can also cause immunological reactions. Gingival hyperplasia, as well as teratogenic effects - toxic reactions of phenytoin have been recorded in animals. It has been proven that these effects are due to the action of phenytoin metabolites: parahydroxylate and dihydrodiol. As shown by Buecher et al. (1990), low ERNX1 activity (less than 30% of normal) in amniocytes is a serious risk factor for the development of congenital fetal anomalies in women taking phenytoin during pregnancy. It has also been proven that the main reason for the decrease in ERNX1 activity is a point mutation in exon 3 of the ERNX1 gene; as a result, a defective enzyme is synthesized (tyrosine at position 113 is replaced by histidine). The mutation is inherited in an autosomal recessive manner. A decrease in ERNX1 activity is observed only in homozygotes for this mutant allele. There are no data on the prevalence of homozygotes and heterozygotes for this mutation.
Glutathione transferases
Xenobiotics with different chemical structures undergo conjugation with glutathione: epoxides, arene oxides, hydroxylamines (some of them have carcinogenic effects). Among medicinal substances, ethacrynic acid (uregit ♠) and the hepatotoxic metabolite of paracetamol (acetaminophen ♠) - N-acetylbenzoquinoneimine, are subject to conjugation with glutathione, converting
transforming into a non-toxic compound. As a result of the conjugation reaction with glutathione, cysteine conjugates called “thioesters” are formed. Conjugation with glutathione is catalyzed by the enzymes glutathione SH-S-transferase (GST). This group of enzymes is localized in the cytosol, although microsomal GST has also been described (however, its role in the metabolism of xenobiotics has been little studied). The activity of GST in human erythrocytes varies by 6 times between different individuals, but there is no dependence of enzyme activity on gender). However, research has shown that there is a clear correlation between GST activity in children and their parents. According to the identity of the amino acid composition in mammals, 6 classes of GST are distinguished: α- (alpha-), μ- (mu-), κ- (kappa-), θ- (theta-), π- (pi-) and σ- (sigma -) GST. In the human body, GST classes μ (GSTM), θ (GSTT and π (GSTP) are mainly expressed. Among them, GST class μ, designated as GSTM, are of greatest importance in the metabolism of xenobiotics. Currently, 5 GSTM isoenzymes have been identified: GSTM1, GSTM2, GSTM3, GSTM4 and GSTM5. The GSTM gene is localized on chromosome 1 (locus 1p13.3). GSTM1 is expressed in the liver, kidneys, adrenal glands, stomach; weak expression of this isoenzyme is found in skeletal muscles, myocardium. GSTM1 is not expressed in the fetal liver, fibroblasts, erythrocytes, lymphocytes and platelets. GSTM2 ("muscle" GSTM) is expressed in all of the above tissues (especially muscle), except fibroblasts, erythrocytes, lymphocytes, platelets and fetal liver. GSTM3 ("brain" GSTM) is expressed in all tissues of the body, especially in the central nervous system. GSTM1 plays an important role in the inactivation of carcinogens. Indirect confirmation of this is considered to be a significant increase in the frequency of malignant diseases among carriers of null alleles of the GSTM1 gene, who lack GSTM1 expression. Harada et al. (1987), having studied liver samples taken from 168 corpses, found that the null allele of the GSTM1 gene was significantly more common in patients with hepatocarcinoma. Board et al. (1987) first put forward a hypothesis: inactivation of some electrophilic carcinogens does not occur in the body of carriers of GSTM1 null alleles. According to Board et al. (1990), the prevalence of the GSTM1 null allele among the European population is 40-45%, while among representatives of the Negroid race it is 60%. There is evidence of a higher incidence of lung cancer in carriers of the GSTM1 null allele. As shown by Zhong et al. (1993),
70% of patients with colon cancer are carriers of the GSTM1 null allele. Another GST isoenzyme belonging to the π class, GSTP1 (localized mainly in the liver and blood-brain barrier structures) is involved in the inactivation of pesticides and herbicides widely used in agriculture.
5.5. FACTORS AFFECTING BIOTRANSFORMATION OF DRUGS
Genetic factors influencing the biotransformation system and drug transporters
Genetic factors representing single nucleotide polymorphisms of genes encoding biotransformation enzymes and drug transporters can significantly influence the pharmacokinetics of drugs. Interindividual differences in the rate of drug metabolism, which can be assessed by the ratio of the concentration of a drug substrate to the concentration of its metabolite in the blood plasma or urine (metabolic ratio), make it possible to identify groups of individuals that differ in the activity of one or another metabolic isoenzyme.
"Extensive" metabolizers (extensive metabolism, EM) - persons with a “normal” rate of metabolism of certain drugs, as a rule, homozygotes for the “wild” allele of the gene for the corresponding enzyme. The majority of the population belongs to the group of “extensive” metabolizers.
"Slow" metabolizers (poor metabolism, PM) - persons with a reduced metabolic rate of certain drugs, usually homozygotes (with an autosomal recessive type of inheritance) or heterozygotes (with an autosomal dominant type of inheritance) for the “slow” allele of the gene for the corresponding enzyme. In these individuals, the synthesis of a “defective” enzyme occurs, or there is no synthesis of the metabolic enzyme at all. As a result, there is a decrease in enzymatic activity. Often a complete absence of enzymatic activity is detected. In this category of people, high ratios of the concentration of the drug to the concentration of its metabolite are recorded. Consequently, in “slow” metabolizers, drugs accumulate in the body in high concentrations; this leads to the development
There are severe adverse drug reactions, including intoxication. That is why such patients (slow metabolizers) need to carefully select the dose of drugs. “Slow” metabolizers are prescribed lower doses of drugs than “active” ones. "Superactive" or "fast" metabolizers (ultraextensive metabolism, UM) - persons with an increased metabolic rate of certain drugs, as a rule, homozygotes (with an autosomal recessive type of inheritance) or heterozygotes (with an autosomal dominant type of inheritance) for the “fast” allele of the gene for the corresponding enzyme or, what is more often observed, carrying copies of functional alleles. In this category of people, low values of the ratio of the concentration of the drug to the concentration of its metabolite are recorded. As a result, the concentration of drugs in the blood plasma is insufficient to achieve a therapeutic effect. Such patients (“overactive” metabolizers) are prescribed higher doses of drugs than “active” metabolizers. If there is genetic polymorphism of a particular biotransformation enzyme, then the distribution of individuals according to the rate of metabolism of drug substrates for this enzyme becomes bimodal (if there are 2 types of metabolizers) or trimodal (if there are 3 types of metabolizers) in nature.
Polymorphism is also characteristic of genes encoding drug transporters, and the pharmacokinetics of a drug can vary depending on the function of this transporter. The clinical significance of the most significant biotransformation enzymes and transporters is discussed below.
Induction and inhibition of the biotransformation system and transporters
The induction of a biotransformation enzyme or transporter is understood as an absolute increase in its quantity and (or) activity due to the influence of a certain chemical agent, in particular a drug. In the case of biotransformation enzymes, this is accompanied by hypertrophy of the ER. Both phase I enzymes (cytochrome P-450 isoenzymes) and phase II biotransformation (UDP-glucuronyltransferase, etc.), as well as drug transporters (glycoprotein-P, transporters of organic anions and cations), can be induced. Drugs that induce biotransformation enzymes and transporters do not have obvious structural similarities, but they are characterized by
thorns are some common signs. Such substances are fat soluble (lipophilic); serve as substrates for enzymes (which they induce) and most often have a long half-life. Induction of biotransformation enzymes leads to acceleration of biotransformation and, as a rule, to a decrease in pharmacological activity, and, consequently, to the effectiveness of drugs used together with the inducer. Induction of drug transporters can lead to various changes in the concentration of drugs in the blood plasma, depending on the functions of this transporter. Various substrates are capable of inducing drug biotransformation enzymes and drug transporters with different molecular weights, substrate specificities, immunochemical and spectral characteristics. In addition, there are significant interindividual differences in the intensity of induction of biotransformation enzymes and drug transporters. The same inducer can increase the activity of an enzyme or transporter in different individuals by 15-100 times.
Basic types of induction
“Phenobarbital” type of induction - direct effect of the inducer molecule on the regulatory region of the gene; this leads to the induction of a biotransformation enzyme or drug transporter. This mechanism is most typical for autoinduction. Autoinduction is understood as an increase in the activity of an enzyme that metabolizes a xenobiotic under the influence of the xenobiotic itself. Autoinduction is considered as an adaptive mechanism developed in the process of evolution for the inactivation of xenobiotics, including those of plant origin. Thus, garlic phytoncide - dialyl sulfide - has autoinduction towards cytochromes of subfamily IIB. Barbiturates (inducers of cytochrome P-450 isoenzymes 3A4, 2C9, subfamily IIB) are typical autoinducers (among medicinal substances). That is why this type of induction is called “phenobarbital”.
“Rifampicin-dexamethasone” type - induction of cytochrome P-450 isoenzymes 1A1, 3A4, 2B6 and glycoprotein-P is mediated by the interaction of the inducer molecule with specific receptors, they belong to the class of transcription regulator proteins: pregnane X receptor (PXR), Ah- receptor, CAR receptor. By combining with these receptors, drug inducers form a complex that, penetrating into the cell nucleus, affects
Regulatory region of the gene. As a result, the drug biotransformation enzyme, or transporter, is induced. By this mechanism, rifampins, glucocorticoids, St. John's wort preparations and some other substances induce cytochrome P-450 and glycoprotein P isoenzymes. “Ethanol” type - stabilization of the drug biotransformation enzyme molecule due to the formation of a complex with some xenobiotics (ethanol, acetone). For example, ethanol induces the 2E1 isoenzyme of cytochrome P-450 at all stages of its formation: from transcription to translation. It is believed that the stabilizing effect of ethanol is associated with its ability to activate the phosphorylation system in hepatocytes through cyclic AMP. By this mechanism, isoniazid induces the 2E1 isoenzyme of cytochrome P-450. The process of induction of the 2E1 isoenzyme of cytochrome P-450 during fasting and diabetes mellitus is associated with the “ethanol” mechanism; in this case, ketone bodies act as inducers of the 2E1 isoenzyme of cytochrome P-450. Induction leads to an acceleration of the biotransformation of drug substrates of the corresponding enzymes, and, as a rule, to a decrease in their pharmacological activity. Among the inducers most often used in clinical practice are rifampicin (inducer of isoenzymes 1A2, 2C9, 2C19, 3A4, 3A5, 3A6, 3A7 of cytochrome P-450; glycoprotein-P) and barbiturates (inducers of isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 3A4 , 3A5, 3A6, 3A7 cytochrome P-450). The inducing effect of barbiturates takes several weeks to develop. Unlike barbiturates, rifampicin, as an inducer, acts quickly. The effect of rifampicin can be detected after 2-4 days. The maximum effect of the drug is recorded after 6-10 days. Induction of enzymes or drug transporters caused by rifampicin and barbiturates sometimes leads to a decrease in the pharmacological effectiveness of indirect anticoagulants (warfarin, acenocoumarol), cyclosporine, glucocorticoids, ketoconazole, theophylline, quinidine, digoxin, fexofenadine and verapamil (this requires correction of the dosage regimen of these drugs t i.e. increasing the dose). It should be emphasized that when an inducer of drug biotransformation enzymes is discontinued, the dose of the combined drug should be reduced, as its concentration in the blood plasma increases. An example of such an interaction is a combination of indirect anticoagulants and phenobarbital. Studies have shown that in 14% of cases of bleeding during treatment
indirect anticoagulants develop due to the withdrawal of drugs that induce biotransformation enzymes.
Some compounds can inhibit the activity of biotransformation enzymes and drug transporters. Moreover, with a decrease in the activity of enzymes that metabolize drugs, the development of side effects associated with long-term circulation of these compounds in the body is possible. Inhibition of drug transporters can lead to various changes in the concentration of drugs in the blood plasma depending on the functions of this transporter. Some medicinal substances are capable of inhibiting both enzymes of phase I of biotransformation (isoenzymes of cytochrome P-450) and phase II of biotransformation (N-acetyltransferase, etc.), as well as drug transporters.
Basic mechanisms of inhibition
Binding to the regulatory region of the gene for a biotransformation enzyme or drug transporter. According to this mechanism, drug biotransformation enzymes are inhibited under the influence of a large amount of the drug (cimetidine, fluoxetine, omeprazole, fluoroquinolones, macrolides, sulfonamides, etc.).
Some drugs with high affinity (affinity) for certain isoenzymes of cytochrome P-450 (verapamil, nifedipine, isradipine, quinidine) inhibit the biotransformation of drugs with lower affinity for these isoenzymes. This mechanism is called competitive metabolic interaction.
Direct inactivation of cytochrome P-450 isoenzymes (gastoden p). Inhibition of the interaction of cytochrome P-450 with NADP-H-cytochrome P-450 reductase (fumarocoumarins from grapefruit and lime juice).
A decrease in the activity of drug biotransformation enzymes under the influence of appropriate inhibitors leads to an increase in the concentration of these drugs (substrates for enzymes) in the blood plasma. In this case, the half-life of drugs is prolonged. All this causes the development of side effects. Some inhibitors affect several biotransformation isoenzymes simultaneously. Large concentrations of inhibitor may be required to inhibit multiple enzyme isoforms. Thus, fluconazole (an antifungal drug) at a dose of 100 mg per day inhibits the activity of the 2C9 isoenzyme of cytochrome P-450. When the dose of this drug is increased to 400 mg, depression is also noted
activity of isoenzyme 3A4. In addition, the higher the dose of the inhibitor, the faster (and the higher) its effect develops. Inhibition generally develops faster than induction; it can usually be detected within 24 hours from the moment the inhibitors are prescribed. The rate of inhibition of enzyme activity is also affected by the route of administration of the drug inhibitor: if the inhibitor is administered intravenously, the interaction process will occur faster.
Not only drugs, but also fruit juices (Table 5-10) and herbal medicines can serve as inhibitors and inducers of biotransformation enzymes and drug transporters (Appendix 2)- all this has clinical significance when using drugs that act as substrates for these enzymes and transporters.
Table 5-10. The influence of fruit juices on the activity of the biotransformation system and drug transporters
 5.6. EXTRAHEPATIC BIOTRANSFORMATION
5.6. EXTRAHEPATIC BIOTRANSFORMATION
The role of the intestine in the biotransformation of drugs
The intestine is considered the second most important organ (after the liver) that performs the biotransformation of drugs. Both phase I and phase II reactions of biotransformation take place in the intestinal wall. The biotransformation of drugs in the intestinal wall is of great importance in the first-pass effect (presystemic biotransformation). The significant role of biotransformation in the intestinal wall in the first-pass effect of drugs such as cyclosporine A, nifedipine, midazolam, and verapamil has already been proven.
Phase I enzymes of drug biotransformation in the intestinal wall
Among the phase I enzymes of drug biotransformation, cytochrome P-450 isoenzymes are mainly localized in the intestinal wall. The average content of cytochrome P-450 isoenzymes in the human intestinal wall is 20 pmol/mg microsomal protein (in the liver - 300 pmol/mg microsomal protein). A clear pattern has been established: the content of cytochrome P-450 isoenzymes decreases from the proximal to the distal parts of the intestine (Table 5-11). In addition, the content of cytochrome P-450 isoenzymes is maximum at the top of the intestinal villi and minimum in the crypts. The predominant cytochrome P-450 isoenzyme in the intestine is CYP3A4, accounting for 70% of all intestinal cytochrome P-450 isoenzymes. According to different authors, the content of CYP3A4 in the intestinal wall varies, which is explained by interindividual differences in cytochrome P-450. Methods for purifying enterocytes are also important.
Table 5-11. Content of cytochrome P-450 isoenzyme 3A4 in the human intestinal wall and liver
 Other isoenzymes have also been identified in the intestinal wall: CYP2C9 and CYP2D6. However, compared to the liver, the content of these enzymes in the intestinal wall is insignificant (100-200 times less). The conducted studies demonstrated insignificant, compared to the liver, metabolic activity of cytochrome P-450 isoenzymes of the intestinal wall (Table 5-12). As shown by studies examining the induction of cytochrome P-450 isoenzymes of the intestinal wall, the inducibility of intestinal wall isoenzymes is lower than that of liver cytochrome P-450 isoenzymes.
Other isoenzymes have also been identified in the intestinal wall: CYP2C9 and CYP2D6. However, compared to the liver, the content of these enzymes in the intestinal wall is insignificant (100-200 times less). The conducted studies demonstrated insignificant, compared to the liver, metabolic activity of cytochrome P-450 isoenzymes of the intestinal wall (Table 5-12). As shown by studies examining the induction of cytochrome P-450 isoenzymes of the intestinal wall, the inducibility of intestinal wall isoenzymes is lower than that of liver cytochrome P-450 isoenzymes.
Table 5-12. Metabolic activity of cytochrome P-450 isoenzymes of the intestinal wall and liver
 Phase II enzymes of drug biotransformation in the intestinal wall
Phase II enzymes of drug biotransformation in the intestinal wall
UDP-glucuronyltransferase and sulfotransferase are the most well-studied phase II enzymes of drug biotransformation located in the intestinal wall. The distribution of these enzymes in the intestine is similar to cytochrome P-450 isoenzymes. Cappiello et al. (1991) studied the activity of UDP-glucuronyltransferase in the human intestinal wall and liver according to the metabolic clearance of 1-naphthol, morphine and ethinyl estradiol (Table 5-13). Studies have shown that the metabolic activity of intestinal wall UDP-glucuronyltransferase is lower than liver UDP-glucuronyltransferase. A similar pattern is characteristic of the glucuronidation of bilirubin.
Table 5-13. Metabolic activity of UDP-glucuronyltransferase in the intestinal wall and liver
 Cappiello et al. (1987) also studied the activity of sulfotransferase of the intestinal wall and liver according to the metabolic clearance of 2-naphthol. The data obtained indicate the presence of differences in metabolic clearance rates (and the clearance of 2-naphthol in the intestinal wall is lower than in the liver). In the ileum, the value of this indicator is 0.64 nmol/(minxmg), in the sigmoid colon - 0.4 nmol/(minxmg), in the liver - 1.82 nmol/(minxmg). However, there are drugs whose sulfation occurs mainly in the intestinal wall. These include, for example, β 2 -adrenergic agonists: terbutaline and isoprenaline (Table 5-14).
Cappiello et al. (1987) also studied the activity of sulfotransferase of the intestinal wall and liver according to the metabolic clearance of 2-naphthol. The data obtained indicate the presence of differences in metabolic clearance rates (and the clearance of 2-naphthol in the intestinal wall is lower than in the liver). In the ileum, the value of this indicator is 0.64 nmol/(minxmg), in the sigmoid colon - 0.4 nmol/(minxmg), in the liver - 1.82 nmol/(minxmg). However, there are drugs whose sulfation occurs mainly in the intestinal wall. These include, for example, β 2 -adrenergic agonists: terbutaline and isoprenaline (Table 5-14).
Thus, despite a certain contribution to the biotransformation of drugs, the intestinal wall in its metabolic capacity is significantly inferior to the liver.
Table 5-14. Metabolic clearance of terbutaline and isoprenaline in the intestinal wall and liver
 The role of the lungs in the biotransformation of drugs
The role of the lungs in the biotransformation of drugs
In the human lungs there are both phase I enzymes of biotransformation (cytochrome P-450 isoenzymes) and phase II enzymes
(epoxide hydrolase, UDP-glucuronyltransferase, etc.). In human lung tissue, it was possible to identify various isoenzymes of cytochrome P-450: CYP1A1, CYP1B1, CYP2A, CYP2A10, CYP2A11, CYP2B, CYP2E1, CYP2F1, CYP2F3. The total content of cytochrome P-450 in human lungs is 0.01 nmol/mg microsomal protein (this is 10 times less than in the liver). There are cytochrome P-450 isoenzymes that are expressed predominantly in the lungs. These include CYP1A1 (found in humans), CYP2B (in mice), CYP4B1 (in rats) and CYP4B2 (in cattle). These isoenzymes are of great importance in the biological activation of a number of carcinogens and pulmonary toxic compounds. Information on the participation of CYP1A1 in the biological activation of PAHs is presented above. In mice, oxidation of butylated hydroxytoluene by the CYP2B isoenzyme leads to the formation of a pneumotoxic electrophilic metabolite. Isoenzymes CYP4B1 in rats and CYP4B2 in cattle promote the biological activation of 4-ipomenol (4-ipomenol is a potent pneumotoxic furanoterpenoid of the fungus of raw potatoes). It was 4-impomenol that caused the mass death of cattle in the 70s in the USA and England. In this case, 4-ipomenol, oxidized by the CYP4B2 isoenzyme, caused interstitial pneumonia, leading to death.
Thus, the expression of specific isoenzymes in the lungs explains the selective pulmonary toxicity of some xenobiotics. Despite the presence of enzymes in the lungs and other parts of the respiratory tract, their role in the biotransformation of drugs is negligible. The table shows drug biotransformation enzymes found in the human respiratory tract (Table 5-15). Determining the localization of biotransformation enzymes in the respiratory tract is difficult due to the use of lung homogenizate in studies.
Table 5-15. Biotransformation enzymes found in the human respiratory tract
 The role of the kidneys in the biotransformation of drugs
The role of the kidneys in the biotransformation of drugs
Research carried out over the past 20 years has shown that the kidneys are involved in the metabolism of xenobiotics and drugs. In this case, as a rule, there is a decrease in biological and pharmacological activity, but in some cases the process of biological activation (in particular, bioactivation of carcinogens) is also possible.
Both phase I and phase II enzymes of biotransformation were found in the kidneys. Moreover, biotransformation enzymes are localized in both the cortex and medulla of the kidneys (Table 5-16). However, as studies have shown, it is the renal cortex that contains the greater number of cytochrome P-450 isoenzymes, rather than the medulla. The maximum content of cytochrome P-450 isoenzymes was found in the proximal renal tubules. Thus, the kidneys contain the isoenzyme CYP1A1, previously considered specific to the lungs, and CYP1A2. Moreover, these isoenzymes in the kidneys are subject to induction by PAHs (for example, β-naphtholavone, 2-acetylaminoflurin) in the same way as in the liver. CYP2B1 activity was detected in the kidneys; in particular, the oxidation of paracetamol (acetaminophen ♠) in the kidneys under the influence of this isoenzyme was described. Later, it was demonstrated that it is the formation of the toxic metabolite N-acetibenzaquinone imine in the kidneys under the influence of CYP2E1 (by analogy with the liver) that is the main cause of the nephrotoxic effect of this drug. When paracetamol is used together with CYP2E1 inducers (ethanol, testosterone, etc.), the risk of kidney damage increases several times. CYP3A4 activity in the kidneys is not always recorded (only in 80% of cases). It should be noted: the contribution of kidney cytochrome P-450 isoenzymes to the biotransformation of drugs is modest and, apparently, in most cases has no clinical significance. However, for some drugs, biochemical transformation in the kidneys is the main route of biotransformation. Studies have shown that tropisetron p (an antiemetic drug) is mainly oxidized in the kidneys under the influence of the isoenzymes CYP1A2 and CYP2E1.
Among the phase II enzymes of biotransformation in the kidneys, UDP-glucuronyltransferase and β-lyase are most often determined. It should be noted that β-lyase activity in the kidneys is higher than in the liver. The discovery of this feature made it possible to develop some “prodrugs”, upon activation of which active meta-
pain that selectively affects the kidneys. Thus, they created a cytostatic drug for the treatment of chronic glomerulonephritis - S-(6-purinyl)-L-cysteine. This compound, initially inactive, is converted in the kidneys by β-lyase to the active 6-mer captopurine. Thus, 6-mercuptopurine produces its effect exclusively in the kidneys; this significantly reduces the frequency and severity of adverse drug reactions.
Drugs such as paracetamol (acetaminophen ♠), zidovudine (azidothymidine ♠), morphine, sulfamethasone r, furosemide (Lasix ♠) and chloramphenicol (chloramphenicol ♠) are subject to glucuronidation in the kidneys.
Table 5-16. Distribution of drug biotransformation enzymes in the kidney (Lohr et al., 1998)
 * - enzyme content is significantly higher.
* - enzyme content is significantly higher.
Literature
Kukes V.G. Metabolism of drugs: clinical and pharmacological aspects. - M.: Reafarm, 2004. - P. 113-120.
Seredenin S.B. Lectures on pharmacogenetics. - M.: MIA, 2004. -
Diasio R.B., Beavers T.L., Carpenter J.T. Familial deficiency of dihydropyrimidine dehydrogenase: biochemical basis for familial pyrimidinemia and severe 5-fluorouracil-induced toxicity // J. Clin. Invest. - 1988. - Vol. 81. -
Lemoine A., Daniel A., Dennison A., Kiffel L. et al. FK 506 renal toxicity and lack of detectable cytochrome P-450 3A in the liver graft of a patient undergoing liver transplantation // Hepatology. - 1994. - Vol. 20. - P. 1472-1477.
Lewis D.F.V., Dickins M., Eddershaw P.J. et al. Cytochrome-P450 Substrate Specificities, Substrate structural Templates and Enzyme Active Site Geometries // Drug Metabol. Drug Interact. - 1999. - Vol. 15. - P. 1-51.
As a result of chemical modification, drugs usually lose their biological activity. Thus, these reactions limit the effect of drugs in time. In liver pathology, accompanied by a decrease in the activity of microsomal enzymes, the duration of action of a number of medicinal substances increases. Some drugs reduce the activity of the monooxygenase system. For example, chloramphenicol and butadiene inhibit microsomal oxidation enzymes. Anticholinesterase drugs, monoamine oxidase inhibitors, disrupt the functioning of the conjugation phase, so they prolong the effects of drugs that are inactivated by these enzymes. In addition, the rate of each of the drug biotransformation reactions depends on genetic, physiological factors and the ecological state of the environment.
Age characteristics. Sensitivity to drugs varies with age. For example, drug metabolism activity in newborns in the first month of life is significantly different from that in adults. This is due to the deficiency of many enzymes involved in the biotransformation of drugs, kidney function, increased permeability of the blood-brain barrier, and underdevelopment of the central nervous system. Thus, newborns are more sensitive to certain substances that affect the central nervous system (in particular, morphine). Levomycetin is very toxic for them; this is explained by the fact that in the liver of newborns the enzymes necessary for its biotransformation are inactive. In old age, the metabolism of drugs is less efficient: the functional activity of the liver decreases, and the rate of drug excretion by the kidneys is impaired. In general, sensitivity to most drugs in old age is increased, and therefore their dose should be reduced.
Genetic factors. Individual differences in the metabolism of a number of drugs and in reactions to drugs are explained by genetic polymorphism, i.e. the existence of isoforms of some biotransformation enzymes in the population. In some cases, increased sensitivity to drugs may be due to hereditary deficiency of certain enzymes involved in chemical modification. For example, with genetic deficiency of blood plasma cholinesterase, the duration of action of the muscle relaxant ditilin increases sharply and can reach 6-8 hours or more (under normal conditions, dithilin acts for 5-7 minutes). It is known that the rate of acetylation of the antituberculosis drug isoniazid varies quite widely. There are individuals with fast and slow metabolizing activity. It is believed that in persons with slow inactivation of isoniazid, the structure of proteins that regulate the synthesis of the enzyme acetyltransferase, which ensures the conjugation of isoniazid with the acetyl residue, is disrupted.
Environmental factors. Environmental factors, such as ionizing radiation, temperature, food composition, and especially various chemicals (xenobiotics), including the medicinal substances themselves, also have a significant impact on the metabolism of medicinal substances in the body.
Binding of drugs to plasma proteins
Distribution of drugs in the body
After absorption (absorption), the drug enters the systemic circulatory system and is distributed throughout the organs and tissues of the body.
Biological barriers affecting drug distribution:
1. capillary wall;
2. cell membranes;
3. blood-brain barrier;
4. placental barrier.
Factors influencing the distribution of drugs in the body:
1. solubility of drugs in water and lipids:
Hydrophilic drugs penetrate only through capillary membranes and accumulate in the extracellular space;
Lipophilic drugs penetrate all biomembranes;
Drugs insoluble in water and lipids penetrate into cells through pores in membranes or by active transport;
2. ability to bind to blood plasma proteins;
3. features of regional blood flow (first of all, drugs enter well-supplied organs - heart, lungs, liver, kidneys);
4. the ability of drugs to diffuse into organs and tissues;
5. functional state of the cardiovascular system.
Drugs in blood and lymphatic vessels, depending on the characteristics of their chemical structure, interact and bind to blood plasma proteins, as a result of which they lose the ability to penetrate cell membranes. Thus, in the circulation the drug is in active and inactive forms, which are, as a rule, in equilibrium with the same affinity of the drug for plasma proteins and body tissues. Plasma proteins play the role of drug depot. The bonds of drugs with proteins are fragile and there is competition between drugs, which can lead to an increase in the concentration of drugs freed from the protein bond.
The connection of drugs with plasma proteins leads to:
1. increase in the concentration of drugs in the blood;
2. formation of a drug depot in the blood;
3. increasing the half-life of drugs.
Factors limiting the ability of plasma proteins to bind to drugs:
1. uremia;
2. hypoalbuminemia (less than 30 g/l);
3. hyperbilirubinemia and liver failure;
4. free fatty acids, more palmitic than oleic
Factors that enhance the ability of plasma proteins to bind to drugs
1. acute inflammation;
2. initial stage of an infectious disease;
3. increase in ESR (more than 20 mm/h).
Some drugs can bind to tissue proteins and accumulate in them (cardiac glycosides), as well as with erythrocyte membranes.
The bioavailability of a drug is the content of free (not bound to proteins) drug in the blood plasma.
Biotransformation (metabolism) is a complex of physicochemical and/or biochemical reactions that convert drugs into water-soluble compounds (metabolites) that are easily excreted from the body. As a rule, the resulting metabolites are less active and toxic, but the opposite may be true.
Biotransformation can occur in many organs and tissues (intestinal wall, blood plasma, kidneys, lungs), but in most cases in the liver (in microsomes - microsomal biotransformation, in mitochondria and cytoplasm - non-microsomal biotransformation).
Types of drug biotransformation:
1. metabolic transformation - the transformation of substances into metabolites as a result of oxidation, reduction, hydrolysis;
2. conjugation - a process accompanied by the addition of a number of chemical groups or molecules of endogenous compounds to a drug or its metabolites.
Biotransformation phases:
1. Phase I of non-synthetic chemical reactions (formation of an active radical);
2. Phase II of synthetic chemical reactions (attachment to the active radical of endogenous molecules of glucuronic acid, glycine, sulfate, water, etc. and the formation of water-soluble compounds that are excreted in the urine).
Metabolism of drugs leads to:
1. reducing the solubility of drugs in lipids;
2. reducing the biological activity of the drug.
The main places and methods of metabolism of medicinal and toxic substances in the body (diagram)
Factors influencing biotransformation:
1. age;
2. floor;
3. dietary habits (intake of fatty foods, alcohol, coffee, tea enhances drug metabolism; intake of low-protein foods inhibits metabolism);
4. bad habits (increased drug metabolism - alcohol, smoking);
5. simultaneous use of other medications (increased metabolism - phenobarbital, reserpine; inhibition - cimetidine);
6. functional state of the liver;
7. blood supply to the liver, etc.