Hiatal hernia: signs, diagnosis and treatment methods. Treatment of axial hiatal hernia Paraesophageal or fixed hiatus
Hiatal hernia is a pathology that is characterized by protrusion of abdominal organs through the esophageal opening of the diaphragm. As a rule, displacement of the lower part of the esophagus, stomach, and slightly less often other organs occurs.
The pathology is accompanied by the fact that the listed organs are displaced into the chest instead of the abdomen. Another name for this disease is hiatal hernia (abbr.
What is a hiatal hernia? This is a protrusion of the abdominal organs (lower esophagus, stomach, less often other organs) through the natural opening of the diaphragm (esophageal).
That is, the organs included in the protrusion are not in the stomach, but in the chest. Another name for this pathology is hiatal hernia or, for short, hiatal hernia.
In medical practice, axial esophageal hernia is divided into degrees in accordance with the size of the prolapse and the symptoms of the disease.
Not every patient observes manifestations of the pathological process, especially in the initial stages of progression.
Not every patient notices the changes that appear as a result of the development of an axial hernia. In the early stages there are practically no symptoms.
Due to the absence of pronounced symptoms of hiatal hernia, treatment is almost always delayed. The development of the disease necessitates observation by a doctor and professional help.
The use of diets and pills in this case will not help the patient to recover, except perhaps to prevent complications in the form of gastroesophageal reflux disease from developing.
Diet means proper nutrition - in small portions, but often. The patient is prohibited from eating chocolate, flour, consuming animal fats, drinking coffee or soda. The patient should not take a horizontal position for at least 3 hours after eating.
To obtain the greatest effectiveness from non-surgical treatment, the patient must adhere to a healthy lifestyle, eliminating his bad habits. It is necessary to monitor the level of intra-abdominal pressure - it should not increase.
When the organs located below the diaphragm protrude through its natural esophageal opening, this leads to the development of a rather serious pathology of this section - an axial hernia.
This disease has long occupied a very important place among the ailments of the gastrointestinal tract, since in the absence of timely and adequate treatment it can provoke the development of serious complications.
Axial hiatal hernia (HH) is one of the most common types of deformity localized in the digestive organs.
Among all pathologies of the gastrointestinal tract, it ranks 3rd. If it is not detected at the earliest stage of development, then the treatment measures taken may not give the expected result.
A hernia is the exit of one organ from its cavity into the adjacent one through an opening without violating the integrity of the membrane. There are several types of hernias of the digestive system, but the axial one occurs in 90% of cases of disease, that is, in every twentieth.
Axial hiatal hernia
This type of hernia can be congenital or acquired. This disease is associated with pathology of the diaphragmatic opening. With age, the muscles of the diaphragm lose elasticity, so diseases associated with its work most often have an age-related nature.
Diagnosis of a hernia in athletes does not always entail leaving sports. Some types of physical activity will not only not harm the patient, but will also help improve your health. Naturally, we are not talking about professional sports.
The main cause of an axial hernia is large loads on the abdominal muscles if there is a congenital predisposition to weakness of the abdominal wall. Strength sports that require heavy lifting should be abandoned immediately.
You can go swimming and do sports exercises where the main load falls on the biceps and triceps. Not fast cycling and walking also does not cause complications of the disease. The main thing is to do everything in moderation.
Read more about the types and treatment of hiatal hernias here.
Axial hernia in newborns is extremely rare and is considered a pathology of intrauterine development of the fetus. The so-called thoracic gastric defect is characterized by a congenital form of a shortened esophagus.
In this case, the part of the stomach that is located above the diaphragm is not framed by the abdominal cavity.
READ ALSO: Postoperative ventral hernia ICD code
The first signs of the disease are manifested by frequent regurgitation of the baby; after six months, when complementary foods are introduced, vomiting may appear. Children with axial hernia suffer from underweight, growth retardation and malnutrition.
When diagnosing a hiatal hernia in newborns, doctors recommend surgical treatment in order to further avoid the progression of the disease and the development of concomitant diseases.
Proper nutrition is one of the most important factors in treating a hernia. Increased secretion of gastric juice and its reflux into the esophagus leads to irritation of the mucous membrane.
Therefore, it is necessary to reduce the acidity of gastric juice as much as possible by excluding the following foods: confectionery, spices, smoked foods, sweet desserts, spicy dishes and seasonings, fried foods.
Special breathing exercises will improve the patient’s general condition and help strengthen muscles. Breathing exercises should be done daily, two or three hours after eating.
While on your knees, bend left and right. While bending over, inhale; in the starting position, exhale. Then repeat the same exercise while standing. Do each exercise ten times. Lie on your right side, your legs should be 15 centimeters below your head. When you inhale, stick your stomach out as much as possible, and when you exhale, relax it. With each subsequent time, the breath becomes deeper. Do gymnastics for 10 minutes four times a day. After seven days of such training, as you exhale, you need to draw in your stomach. Lie on your back and twist from side to side. In this case, breathing should be measured.
By performing such exercises, improvements are observed after three months.
The symptoms of this pathology directly depend on its type and stage. It should be noted that initially the disease occurs with mild symptoms.
This greatly complicates diagnosis, which leads to certain complications and longer treatment. Therefore, doctors recommend that you be very attentive to your health and, if certain signs occur, consult a specialist in a timely manner.
This will allow you to recognize the disease in the initial stages and begin effective therapy.
Sometimes the presence of the disease may be indicated by regularly occurring hiccups - this symptom is observed in approximately 3% of patients.
With significant sizes of such formations, cardiorespiratory symptoms are often observed. Caused by compression of the lungs and heart. Such signs are rapid heartbeat, cyanosis (blue discoloration of the area around the mouth), shortness of breath and some others.
This pathology refers to internal abdominal hernias, and therefore, when it appears, there are no external manifestations. The symptom complex of diaphragmatic hernia is associated primarily with disruption of the functioning of organs that change their location.
For example, normally the work of the lower esophageal sphincter is ensured by the diaphragm, providing a supporting effect on it. When the cardiac part of the esophagus is displaced upward, insufficiency of this section is observed, which is manifested by gastroesophageal reflux (stomach contents retrogradely enter the esophagus) and is accompanied by irritation of the esophageal mucosa, which is not resistant to the effects of acidic gastric juice.
In severe cases, inflammation may be accompanied by hidden bleeding, which over time may only manifest as anemia.
The main symptom of a diaphragmatic hernia is constant heartburn, the intensity of which increases when changing body position (lying down, while bending the body), as well as after eating and during physical activity.
The second sign of a hiatal hernia, which is observed in approximately half of patients, is chest pain. It should be differentiated from manifestations of cardiovascular diseases.
In the presence of a hiatal hernia, the pain behind the sternum intensifies when bending over or during physical activity. However, when examining a patient, it is worth remembering that a hernia of the diaphragm can be combined with heart disease.
The above symptoms are often accompanied by belching of air or sour, sometimes the patient feels a lump in the throat or pain when swallowing, and there is a sudden increase in blood pressure.
With an axial hernia, characteristic symptoms are often observed.
The video shows an endoscopic analysis of a hiatal hernia. You will become familiar with the structure of this body.
There are two types of sliding hiatal hernia: non-fixed and fixed. An unfixed hernia is a less complex type of pathology, but also requires treatment.
READ ALSO: Bassini repair for inguinal hernia
As for fixed, it is difficult to diagnose, because in the first stages it is almost asymptomatic. As a rule, the patient learns about the disease by chance during an X-ray or medical examination.
Axial hernia of the second degree is manifested by pain in the epigastric region, heartburn, belching, hiccups, and anemia.
In some cases, patients confuse esophageal pain with pancreatic or heart pain. The doctor’s task in this case when diagnosing is to exclude pancreatitis, heart attack, angina pectoris, so you should know the main characteristics of pain symptoms in the disease:
- Moderate intensity of pain, intensifying with physical activity.
- The pain syndrome appears when the patient lies down, stands for a long time, when coughing, flatulence, after eating.
- The pain goes away completely after belching or vomiting.
A hiatal hernia is dangerous because respiratory tract diseases and various inflammations of the lower parts of the esophagus can develop. Prolonged hemorrhages lead to anemia, after which the patient increases the risk of developing esophageal cancer.
In most cases, after the disease develops, people experience reflux esophagitis. If, after the first signs, the disease is not treated for 7-10 years, then in patients, according to gastroenterological studies, the risk of developing esophageal cancer increases by 280%.
The pathology refers to internal hernias, so it does not manifest itself externally. Symptoms are associated with a violation of the position and functioning of internal organs. In addition, it depends on the type and degree of development of the disease.
Treatment of the disease
Symptoms of an axial hernia depend on its stage and the presence of concomitant pathologies. This disease is life-threatening and health-threatening, so it is important to make a timely diagnosis and begin proper treatment.
When the first signs of pathology appear, you should consult a gastroenterologist. With an axial hernia of 1st degree, no symptoms are observed.
The disease is detected during an X-ray examination. In the early stages of development of the pathology, minor pain may be noted.
The intensity of pain increases with physical activity and lying down.
The stomach is one of the key organs, the health of which directly affects the comfort and full functioning of a person. The appearance of a sliding hernia can have a noticeable negative impact on this organ.
This problem cannot be ignored, so it is important to familiarize yourself with the symptoms of the pathology and treatment methods.
Paraesophageal. We are talking about displacement of only part of the stomach without the participation of other organs in the process.
Sliding hernia, also known as axial hernia. In this case, its cardiac part also moves into the chest cavity.
Mixed. We are talking about the signs of the first two types, which appear simultaneously.
Congenital. This diagnosis is made when a hernia is detected, the formation of which occurs against the background of a small esophagus located in the shape of a “thoracic ventricle”. This situation is anomalous.
1. The stomach is located under the diaphragm, the cardia is at the level with it, and the abdominal segment of the esophagus is above the level of the diaphragm.
2. A hiatal hernia of the 2nd degree is distinguished by the fact that the esophagus is compressed evenly, and the cardinal part of the stomach protrudes into the mediastinum.
3. There is a pronounced contraction of the esophagus, and the entire stomach or its component protrudes into the mediastinum.
The key symptoms can be defined as pain that appears with varying frequency and intensity. At the same time, they can be both dull and burning.
Sometimes painful sensations radiate to the heart area, as a result of which patients begin to suspect heart failure. In some cases, a hiatal hernia can cause pain in the interscapular area.
If the disease is caused by a congenital problem such as an insufficiently wide esophagus, then the symptoms may resemble those of an axial hernia. We are talking about heartburn that appears after eating, pain in the chest, worsening in a horizontal position, and pain in other parts of the body.
Difficulty in swallowing food;
Heartburn after exercise or eating;
Pain in the chest area;
Signs of a hiatal hernia may take the form of belching air or stomach contents.
These symptoms are sometimes misjudged by patients. As reviews show, people think that these are signs of other diseases and self-medicate.
Hiatal hernia (HHH, hiatal hernia) is a displacement of the stomach and other organs from the abdominal cavity into the chest cavity through an enlarged esophageal opening. The disease occurs quite often. It is found in 2–16% of persons suffering from gastrointestinal disorders and in 5–15% of patients undergoing X-ray examination for diseases of the digestive tract. In old age, the incidence of the disease reaches 50%. Mostly women over 50 years of age are affected. A sliding (axial) hiatal hernia is the most common type of this pathology.
Show all
Causes
The causes and mechanisms of development of hiatal hernia are complex and depend on various aspects. This pathological condition develops with a combination of the following factors:
- increased intra-abdominal pressure;
- changes on the part of the diaphragm.
Some scientists consider another factor involved in the origin of hiatal hernia - dyskinesia (impaired motility) of the esophagus, as well as reflex and symptomatic esophagospasm (narrowing of its lumen).
Reflex esophagospasm is a common disease that occurs against the background of various lesions of the cervical and thoracic spine, esophagus, stomach, gallbladder, and duodenum.
The following conditions lead to increased pressure inside the abdominal cavity:
- obesity;
- binge eating;
- flatulence;
- persistent cough;
- constipation;
- ascites;
- large intra-abdominal tumors;
- pregnancy;
- lifting weights.
The occurrence of congenital hernias is most often caused by embryonic disorders and developmental anomalies of the gastrointestinal tract; their clinical manifestations are detected in childhood. Acquired hiatal hernias develop predominantly in adults, which is most often associated with involutional anatomical changes in the tissues that form the esophageal opening in the diaphragm.
The earlier appearance of regressive changes in the diaphragm is facilitated by insufficient functional load of this powerful muscle in people who lead a predominantly sedentary lifestyle. Pulmonary emphysema has a significant impact on the process of lowering the diaphragm; some authors point to the dependence of age-related involution of the diaphragm and the development of atherosclerosis.
There is a hereditary predisposition to this pathology, which is associated with the characteristics of connective tissue.
Constitutional weakness of connective tissue is important in the origin of hiatal hernia. This is confirmed by the frequent combination of the disease with flat feet, hernias of other localizations, and varicose veins of hemorrhoidal and saphenous veins. With age, the developing expansion of the esophageal opening and relaxation of the fascial fixation of the esophagus create an unfavorable background on the basis of which hiatal hernias form. Also, the difference in pressure in the thoracic and abdominal cavities plays a significant role in the development of hiatal hernia.
In some cases, severe abdominal tension itself can lead to the development of hiatal hernia, as well as other abdominal hernias. This mechanism of hernia formation is observed more often in young patients.
Classification
The basis of all modern typologies is the classification of Akerlud and Sealy. The authors identified 3 main types of this pathology:
- 1. Sliding (axial, axial) hernia. It is observed in almost 90% of patients with hiatal hernia. With this type, the cardia is located above the esophageal opening of the diaphragm, therefore the relationship between the esophagus and the stomach changes and the closing function of the cardiac sphincter is sharply disrupted.
- 2. Paraesophageal hernia. Occurs in approximately 5% of patients. It is characterized by the fact that the cardia does not change its position, and the fundus and greater curvature of the stomach emerge through the enlarged opening.
- 3. Short esophagus. It is rare as an independent disease and represents a developmental anomaly. It is usually observed in combination with a sliding hernia and is a consequence of various changes in the wall of the esophagus.


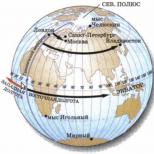
On the left is the normal location of the stomach and esophagus. In the center and on the right - options for sliding hernias

Short esophagus
There is also a classification depending on the volume of penetration of the stomach into the chest cavity. This division is based on the radiological manifestations of the disease.
There are 3 degrees of hiatal hernia:
- 1. 1st - the abdominal section of the esophagus is located in the chest cavity, and the cardia is at the level of the diaphragm. The stomach is elevated and directly adjacent to the diaphragm.
- 2. 2nd - the abdominal section of the esophagus is located in the chest cavity, and directly in the area of the esophageal opening of the diaphragm is already part of the stomach.
- 3. 3rd - the abdominal section of the esophagus, cardia and part of the stomach (fundus and body, and in severe cases even the antrum) are located above the diaphragm.

Symptoms
The clinical symptoms of sliding (axial) hiatal hernias are caused by insufficiency of the cardiac sphincter, resulting in gastroesophageal reflux (GER) and esophagitis.
The main symptoms are pain, heartburn, regurgitation, belching, dysphagia, and anemia.
The most common and painful symptom is pain. It is usually localized in the lower third of the sternum, in the area of the xiphoid process and radiates to the back, left shoulder, and left arm. The frequency, intensity and duration of pain in the same patient are different. More often it is described as burning.
In some patients, it is difficult to distinguish it from pain due to angina or myocardial infarction, and only an electrocardiogram allows one to differentiate these diseases. Although in some cases, a hiatal hernia can cause spasm of the coronary vessels with the subsequent development of morphological changes in the heart muscle. Bergman described epiphrenal syndrome, characterized by chest pain, disturbance of heart rhythm, caused by compression of the trunks of the vagus nerves in the esophageal opening of the diaphragm by the stomach extending into the chest cavity.
Typically, pain appears after lifting weights, when bending the body forward (the “laces” symptom, as defined by French authors), as well as under the influence of other factors that contribute to an increase in intra-abdominal pressure. In many patients, the pain intensifies after eating, in a horizontal position, or at night.
The consequence of insufficiency of the closing function of the cardiac sphincter is the reflux of acidic gastric contents into the esophagus and the occurrence of heartburn. The latter is persistent and painful in nature and, like pain, most often occurs in a horizontal position of the patient. In some patients it predominates at night. Heartburn decreases after eating, eating dairy products, butter and increases after eating spicy foods. It should be remembered that not all people have heartburn when even very acidic gastric contents are thrown into the esophagus.
In some patients, swallowed food returns to the oral cavity without gagging.
If the gastric contents reach the pharynx and oral cavity, then they speak of regurgitation. The latter is observed in a third of patients. More often, the backflow of sour or bitter liquid occurs suddenly when the patient is in a horizontal position or when the body is tilted and is not accompanied by nausea. Such suddenness can cause aspiration, which leads to a coughing fit and/or an unpleasant feeling of “soreness” in the throat.
A common symptom of hiatal hernia is belching. It may be the only symptom of the disease; in severe cases, patients cannot appear in public places because of this. Regurgitation occurs either with sour contents or with air. Belching often brings relief, reducing the feeling of fullness in the epigastric region, although in some patients this is followed by burning pain in the chest. This symptom in most cases occurs immediately after eating or after 20-30 minutes, which can be explained by an increase in intraluminal pressure due to gastric overfilling. Some patients experience belching when bending their torso forward.
Up to a third of patients with different types of hiatal hernia complain of dysphagia. This symptom in the initial stages of the disease usually occurs as a result of spasm of the lower segment of the esophagus, and in later stages - due to the formation of peptic strictures of the esophagus. Patients localize the sensation of food retention at the level of the xiphoid process. With axial hernias, dysphagia usually does not reach significant severity, appears periodically and often worsens when eating in a hurry and in stressful situations.
Nausea, vomiting, shortness of breath, hiccups, burning tongue are very rare symptoms of a sliding hernia.
A special symptom is episodic aphagia. It occurs suddenly and is caused by eating and drinking liquids. During an attack, the patient is completely unable to swallow. The attack usually lasts several hours. There is pain and a significant amount of mucus is formed. Aphagia stops suddenly or decreases gradually.

Diagnostics
The main method of diagnosis, along with clinical data, are x-ray examination methods.
In case of large fixed hernias, even with a plain radiography of the abdominal organs, clearing and a horizontal fluid level can be observed against the background of the shadow of the heart. A gas bubble with a horizontal liquid level is especially clearly visible in the lateral projection.
A study with a contrast agent makes it possible to definitively detect the part of the stomach with typical folds of the mucous membrane located above the diaphragm. In this case, there is also a gaping of the cardial opening with the throwing of the contrast agent into the esophagus. The movement of the stomach above the level of the diaphragm is especially clearly noticeable.
Insufficiency of the cardiac sphincter is determined in the Trendelenburg position with dosed compression of the abdomen. This technique is mandatory when diagnosing small, unfixed hiatal hernias.

X-ray contrast examination of the gastrointestinal tract. The arrow indicates a sliding hernia (the cardiac part of the stomach is located in the chest)
In rare cases, when performing a chest CT scan for another reason, a hiatal hernia may be accidentally detected.
For complaints indicating reflux esophagitis, FEGDS is performed. The procedure is carried out to assess the condition of the esophageal mucosa and exclude a malignant disease.
Treatment
For small asymptomatic hernias, therapy is not indicated. In the case of hernias that cause minor patient complaints, conservative treatment is recommended aimed at reducing intra-abdominal pressure (eliminating constipation, prolonged cough and combating obesity). Drugs are prescribed to reduce GER, suppress gastric acidity, eliminate esophagitis and esophageal motility disorders.
Contraindicated for hiatal hernia:
- smoking;
- heavy physical activity;
- wearing bandages and tight belts that increase intra-abdominal pressure.
The patient must sleep with the head of the bed elevated. It is recommended to adhere to a certain diet, the main features of which are the following:
- you need to eat in small portions and often (about 5-6 times a day);
- take your last meal 3-4 hours before bedtime;
- food should be mechanically, thermally and chemically gentle.
Drug therapy consists of taking proton pump inhibitors (Omeprazole, etc.), H2-histamine receptor blockers (Ranitidine, Famotidine, etc.) or antacids (Almagel, etc.).
Combinations of these drugs are widely used, taking into account the severity of reflux esophagitis and concomitant diseases. If motility of the esophagus and stomach is impaired, antispasmodics (papaverine hydrochloride, No-spa), as well as Metoclopramide, are used. Additionally, physiotherapeutic procedures are used (Shcherbakov collar, electrophoresis with novocaine).
Surgical treatment is indicated for:
- the presence of large hernias that cannot be treated conservatively;
- peptic painful esophagitis with symptoms of angina pectoris;
- severe dysphagia;
- bleeding;
- peptic stricture of the esophagus;
- severe regurgitation;
- metaplasia;
- pulmonary complications.
Today, the most common operations are Nissen, Hill and Beley.
Complications of hiatal hernia
Complications of hiatal hernias are the following conditions:
1.Reflux esophagitis:
- erosion and ulcer of the esophagus;
- peptic stricture of the esophagus;
- esophageal bleeding (acute or chronic);
- anemia - as a consequence of chronic esophageal bleeding;
- esophageal carcinoma;
- complications from the respiratory system - aphonia (as a result of a chemical “burn” of the vocal cords), cough, bronchitis, asthmatic bronchitis, pneumonia, hemoptysis, shortness of breath, diffuse pulmonary fibrosis.
2. Prolapse of the gastric mucosa into the esophagus.
3. Invagination of the esophagus into the stomach.
4. Strangulated hernia.
5. Perforation of the esophagus.
Sliding hernias are never strangulated, while in paraesophageal hernias this complication is common.
What is an axial hiatal hernia? It is characterized by the movement of the stomach into the chest cavity. This disease is diagnosed in older patients, and most often it occurs without obvious clinical signs.
Normally, the abdominal organs (stomach and spleen) are located in the abdominal cavity. If new growths appear on them, they protrude under the skin. If there is an axial hiatal hernia, it is impossible to diagnose it during an external examination of the patient, because the abdominal organs, when enlarged, extend into the inner part of the chest.
Pain may occur when changing body position. Advanced forms of axial hiatal hernia are characterized by the opening of internal bleeding from the vessels of the esophagus. Patients experience signs of anemia and anemia.
There are several reasons that lead to the development of this pathology:

Classification
Axial hiatal hernia, what it is, the doctor will help you figure it out, is divided into several types:

Clinical manifestations
For such a series of diseases as axial cardiac hiatal hernia, fixed axial hiatal hernia, axial hiatal hernia, different clinical manifestations are characteristic. If you notice the first symptoms, you should immediately seek help from a doctor.

Self-medication and purchasing medications without a prescription are strictly prohibited because there is a high risk of serious complications.

Heartburn
Patients experience a burning sensation in the stomach and larynx. You need to pay special attention to this symptom. As gastroesophageal reflux progresses, discomfort appears after eating food because it moves from the stomach back into the esophagus and irritates the mucous membrane. The tone of the esophageal sphincter becomes weak and does not perform its functions. Heartburn in patients most often occurs in a horizontal position at night.
Hiccups and intestinal discomfort
Hiccups refer to spontaneous spasms of the diaphragm. As the hernia increases in size, it irritates the diaphragmatic nerve fibers. Hiccups appear after eating and last for several minutes. Pressing and sharp pain in the intestines, as well as the chest, appears in the morning after sleep, when the hernia descends to the diaphragmatic opening.
When a person engages in active exercises, the body position changes, the torso bends, and when walking quickly, the pain intensifies. With spasms, the likelihood of reflux of stomach contents into the oral cavity through the esophagus increases.

Belching
If oxygen enters the stomach when chewing food, patients experience belching. In the absence of pathological disorders in the body of a healthy person, air gradually and slowly escapes through the mouth. An axial hernia causes high pressure inside the stomach. That is why the air quickly and with some effort comes back out.
When a patient has an increased level of acidity in the stomach, a sour taste appears in the mouth. During sleep, patients with axial hernia often belch with food. There is a high probability of pieces of food getting into the respiratory tract, so a person experiences a characteristic suffocating cough, shortness of breath, and pneumonia.
Dysphagia
 Difficulties in swallowing are observed in patients who do not chew food well, drink very hot tea, or quickly eat ice cream. A person feels sharp pain and discomfort, so this symptom should not be ignored.
Difficulties in swallowing are observed in patients who do not chew food well, drink very hot tea, or quickly eat ice cream. A person feels sharp pain and discomfort, so this symptom should not be ignored.
If complications develop, a person will not be able to swallow dry and solid foods, so they take liquid or pureed food.
This disease can cause hemorrhage in internal organs. Patients' general health sharply deteriorates, weakness and malaise occur.
Diagnosis of the disease
Axial hiatal hernia can be diagnosed using the following methods:
- X-ray. It is carried out in a vertical position. When diagnosing a defect such as axial hiatal hernia of the 1st degree, the patient lies on his back. A contrast agent is injected into the blood to differentiate an axial or paraesophageal hernia.
- CT scan chest. The doctor examines the internal organs and their contents layer by layer.
- Endoscopic examination– checking the condition of the mucous membranes of the esophagus and stomach.
- Esophagomanometry. In laboratory conditions, internal pressure and contractility in the esophagus are measured.

Treatment with medications
Treatment of axial hiatal hernia begins with conservative methods. At the initial stage, this pathology has similar symptoms to gastroesophageal reflux. It is strictly forbidden to buy medicines without a doctor’s prescription or on the recommendation of friends.
 Patients are prescribed complex therapy:
Patients are prescribed complex therapy:
- taking antacid medications containing magnesium and aluminum hydroxide;
- H2 blockers production of histamine receptors (ranitidine);
- Omeprazole, Esomeprazole, Pantoprazole.
During treatment with medications, it is important for patients to normalize their own weight, adhere to a strict diet, eat small portions 4-5 times a day . It is forbidden to sleep after eating. In bed, you need to raise the head of the bed and not engage in physical activity.
Useful video
How axial hiatal hernia of the 2nd degree, axial fixed hiatal hernia, axial hiatal hernia of the 1st degree are treated worries many. Let's figure it out.
Surgery
If drug therapy does not bring the expected effect, then doctors decide on the advisability of surgical intervention. The main task is to restore the natural anatomical features of the gastrointestinal tract.
Surgery is indicated in the following situations:

During surgery, a specialist removes the hernia and restores the areflux mechanism (to prevent the re-reflux of food from the stomach into the esophagus). The operation is indicated for patients who have serious complications, the hernia regularly increases, and the mucous membrane of the esophagus is deformed. After receiving the diagnostic results, patients are prescribed one of the following surgical operations:

If acute cramps in the abdomen or chest appear during sleep, you should consult a physician. It will help to make a correct diagnosis electrocardiography And esophagoduodenoscopy. Some patients have an x-ray of the esophagus, but a radiopaque contrast agent is injected into the blood before the procedure.
Once the diagnosis is confirmed, further treatment is carried out by a gastroenterologist. If there is a high risk of complications and with an advanced form of the disease, patients undergo surgical intervention. Additionally, it is recommended to consult a cardiologist to exclude the development of cardiac pathology.
When the organs located below the diaphragm protrude through its natural esophageal opening, this leads to the development of a rather serious pathology of this section - an axial hernia. This disease has long occupied a very important place among the ailments of the gastrointestinal tract, since in the absence of timely and adequate treatment it can provoke the development of serious complications. Axial hiatal hernia (HH) is one of the most common types of deformity localized in the digestive organs. Among all pathologies of the gastrointestinal tract, it ranks 3rd. If it is not detected at the earliest stage of development, then the treatment measures taken may not give the expected result.
Main types and stages of pathology
Such hernias are called hiatal hernias and are a pathological protrusion of the peritoneal organs through a natural opening located in it. This is mainly the stomach and lower part of the esophagus. When a person develops this disease, they end up in the sternum instead of the abdominal cavity. The disease can be both congenital and acquired, and according to morphological characteristics, hiatal hernias of the PAD are divided into 2 types:
- Sliding (axial, also called axial). The most common type of pathology. According to statistics, it is diagnosed in 90% of cases. An axial hiatal hernia gets its name because it causes the upper stomach and lower alimentary sphincter (LES) to freely slip into the chest cavity and return. This type of digestive disease is divided into several varieties - total gastric, esophageal, subtotal and cardiac hernia. Most often, this pathological movement occurs when a sick person changes body position.
- Paraesophageal (fixed) hernia is much less common than sliding one. It represents a movement into the chest cavity of the cardiac part of the main digestive organ, which does not descend back, but remains there forever. That is why this type of pathology has constant symptoms. A fixed type paraesophageal hernia is more dangerous than a sliding hernia and more often causes the development of a large number of serious complications, which require emergency treatment to get rid of.
Also, this disease is usually divided according to the degrees of development. A hernia of the first stage is characterized by the fact that the abdominal part of the esophagus is located directly above the diaphragm, and the stomach is slightly elevated and pressed tightly against it. In degree II, part of the main digestive organ has already been moved to the POD, and III, the heaviest, is characterized by the presence above the diaphragm of not only the cardia of the stomach, but often its body, or bottom.
Reasons for the development of the disease
Both congenital and acquired conditions can lead to the formation of a hernial opening in the diaphragm. Among the first, experts highlight underdevelopment of the diaphragmatic muscle and hernial pockets formed during intrauterine development. Acquired causes include the influence of age-related changes, serious injuries to the sternum, constantly increased intra-abdominal pressure and the occurrence of an inflammatory process near the diaphragm.
There are also factors that increase the risk of developing pathology. Among them are the following circumstances that provoke a one-time sharp or constant increase in intra-abdominal pressure:
- last degree of obesity;
- blunt abdominal trauma;
- lifting excessive weights;
- hard physical work;
- ascites;
- prolonged uncontrollable vomiting;
- constant constipation.
A professional heavyweight athlete can also get a hernia, especially if he does not follow safety rules when lifting weights. Also of no small importance in the development of this disease is the hypermotor dyskinesia of the esophagus that accompanies chronic gastroduodenitis or pancreatitis, calculous cholecystitis and gastric or duodenal ulcers, namely the disruption of its motor function.
It causes a person to develop an axial hernia of the esophagus and its longitudinal shortening, which occurs due to the appearance of scar-inflammatory deformation, the occurrence of which is provoked by a thermal or chemical burn, esophageal peptic ulcer and reflux esophagitis.
Signs of the disease
In almost half of the cases, the disease is completely asymptomatic or has such minor manifestations that people with a developing disease do not pay attention to them and the pathology continues to progress, carrying the threat of complications. Such hernias of the esophagus are diagnosed completely by chance, when an X-ray examination of the esophagus is performed for a completely different reason.
But still, patients of the gastroenterology department who are at risk for developing this disease of the digestive organs should know its main possible symptoms. First of all, it includes pain, localized in the epigastric region and having a pressing and dull nature. It can radiate along the esophagus to the area between the shoulder blades.
Most often, exacerbation of pain occurs in a lying position, with excessive physical exertion or severe coughing and after a heavy meal. Also characteristic symptoms of pathology may be:
- Hiccups that occur because the hernial sac begins to irritate the phrenic nerve.
- Heartburn and belching. They are the most common negative manifestations of this disease and are provoked by acidic stomach contents entering the esophagus due to gastroesophageal reflux.
- Burning pain behind the sternum and squeezing in the intestines. Their appearance most often occurs in the morning and is associated with the movement of the hernial sac through the hole in the diaphragm.
- Dysphagia (impaired swallowing process). Patients with a history of this disease find it most difficult to swallow, no matter how strange it may be, liquid food. This symptom can occur when eating very hot or cold foods, or eating food too quickly.
Very often, the negative symptoms of this pathology are similar to the main signs of cardiac diseases, and this can complicate diagnosis and may cause the treatment to be prescribed incorrectly and not give the expected effect.
Diagnosis and basic therapeutic measures
Hernial sacs of the esophagus are most often discovered during an endoscopic examination or radiography of the abdominal or chest organs. The main signs indicating the presence of the disease during such a study are considered:
- increased location of the esophageal sphincter;
- the absence of a subdiaphragmatic section in this digestive organ;
- cardia, located directly above the diaphragm;
- expanded diameter of the esophageal opening;
- delay in a hernia injected directly for barium suspension contrast.
When performing endoscopy, the development of this disease is indicated by signs of diseases such as ulcers, erosion, gastritis or esophagitis, as well as the presence of the esophageal-gastric line above the diaphragm. In order to exclude the presence of malignant neoplasms, a biopsy is mandatory in patients with suspected hiatal hernia. To detect internal bleeding from the gastrointestinal tract, stool is examined for occult blood.
After carrying out all these diagnostic measures and confirming the diagnosis, the specialist selects a treatment protocol for the disease that is appropriate for each specific patient and begins to treat the axial hernia.
Treatment of the disease
Treatment of pathological protrusion of the diaphragm is carried out in two ways - surgical and conservative. The second, non-surgical method, is indicated in cases where the hernia is small in size and occurs without obvious symptoms. An integral part of such therapy is the correction of lifestyle and diet, as well as the appointment of medication, the same as for gastroesophageal reflux. Reviews from patients who have undergone this treatment are only positive. Almost all of them achieved complete recovery or transition of the pathology into a state of long-term remission.
But unfortunately, conservative therapy is not suitable for everyone. In this case, surgical intervention is prescribed. Indications for it are severe esophagitis that cannot be treated with medication, insufficiency of the lower diaphragmatic sphincter, and significant narrowing of the esophagus. This operation serves the following purposes:
- creation of an anti-reflux mechanism that prevents the reflux of acidic gastric enzyme into the esophagus;
- restoration of the anatomical structures of damaged digestive organs, as well as the natural relationship between the stomach and esophagus.
There are several operations to get rid of this pathology, and each has its own advantages and disadvantages. Access to a protruding hernial sac can be performed laparoscopically or openly.
After surgery, the patient must be prescribed a course of medications, including histamine receptor blockers, proton pump inhibitors, antacids and prokinetics.
A complete revision of the lifestyle and habits of the sick person is also necessary:
- physical activity, if any, should be reduced;
- a fixing bandage is worn for long-term wear;
- a diet is prescribed to spare the digestive organs and also reduce weight.
Also, after surgery, patients should completely avoid situations that contribute to increased intra-abdominal pressure and completely stop smoking. Among the possible complications of the pathology that develop when the recommendations of the attending physician are ignored and the therapeutic course is violated, the occurrence of such pathologies as massive bleeding from the esophagus, peptic ulcer, cicatricial stenosis and reflux esophagitis is noted.
The choice of treatment tactics for this disease is the prerogative of a specialist. In order to cope with negative symptoms and stop the development of a hernia without surgery, the patient must strictly follow all the recommendations of the attending physician. After the therapeutic course, visits to a gastroenterologist for routine examinations will be necessary for a certain period of time. They are held every six months.
A hiatal hernia appears in the area of the diaphragmatic opening of the esophagus. This is the most common pathology among all diaphragmatic hernias. It is most often diagnosed in women and the risk of its occurrence increases with age. Another name for it.
What is a hiatal hernia? This is a chronic disease of a recurrent nature, in which, through an enlarged diaphragmatic opening, protrusion into the chest cavity of the lower (abdominal) portion of the esophagus, stomach, and less commonly other organs of the abdominal cavity occurs.
Classification
There are several types of hiatal hernia:
- Sliding or axial hernia. With this pathology, the abdominal section of the esophagus and the cardiac part of the stomach move without problems through the diaphragmatic opening of the esophagus into the chest cavity and back. Normally, these organs should be localized in the abdominal cavity.
- A paraesophageal hernia is a rare type of hiatal hernia, in which the stomach seems to turn over and its lower section, sometimes along with other organs, passes through the opening of the diaphragm, while the correct section of the stomach is in the anatomical position.
- Combined hernia. With this pathology, symptoms of sliding and paraesophageal hernia are observed.
Types of hiatal hernia
Depending on the severity of the pathology, axial hernia can be grade 1 or 2.
What is a grade 1 sliding hiatal hernia? With this course of the disease, only the esophagus protrudes into the chest cavity, and the stomach is localized above its anatomical position closer to the diaphragm. If a sliding hernia of the 1st degree is found in patients of an older age group, then it is considered a borderline condition that develops as a result of age-related changes.
With the development of a grade 2 hiatal hernia, the esophagus and stomach simultaneously protrude into the chest cavity.
Causes
The reasons for the formation of a hiatal hernia are varied:
- age-related changes;
- malignant neoplasms;
- injuries;
- surgical interventions;
- gastrointestinal motility disorder;
- chronic diseases of the liver, pancreas and stomach;
- genetic predisposition;
- congenital pathologies, such as underdevelopment of the diaphragm, the appearance of hernias in the prenatal period.
Any factors that increase intra-abdominal pressure also provoke the appearance of a hernia. For example, protrusion of the esophagus is possible during physical activity or coughing.
Important! Wearing tight clothing can provoke the development of the disease.
The period of bearing a child and excess body weight can also cause expansion of the diaphragmatic opening of the esophagus. A hernia often appears in patients suffering from flat feet and Marfan disease.
Clinical picture
The symptoms of a hiatal hernia can vary greatly depending on the extent of the disease.
At the early stage of development of the pathology, the clinical manifestations are mild and most often it is diagnosed accidentally during a medical examination or x-ray.
Depending on the type of hernia and its degree, various signs may be observed.
With a sliding hernia of the 1st degree, the following is noted:
- heartburn after eating, especially if the diet is violated;
- pain in the epigastrium when staying in a bent position for a long time.

One of the signs of a hiatal hernia is the appearance of pain in the epigastric region
Warning! One of the characteristic initial signs of pathology is the appearance of pain that radiates to the back. They intensify with physical activity and when taking a lying position.
When the disease progresses to stage 2, the following is observed:
- constant heartburn that appears regardless of food;
- belching, nausea, dysphagia, hiccups, abdominal pain;
- anemia;
- burning chest pain, similar to attacks of “angina pectoris”;
- painful sensations intensify when bending over and when taking a horizontal position;
- development of bleeding.
Warning! A 2nd degree hernia is dangerous because if left untreated it can cause a heart attack or stroke.
With a paraesophageal hernia, signs caused by gastric prolapse are observed:
- painful sensations after eating, especially if you bend your torso forward;
- burning sensation in the esophagus, belching, nausea;
- disorders of the heart and lungs are observed in cases of their compression by large formations: dyspnea, tachycardia, blue discoloration of the nasolabial triangle, especially after eating.
Warning! A hiatal hernia of the esophagus may be accompanied by bronchoesophageal syndrome, in which respiratory disorders develop: the patient suddenly develops inflammation of the lungs, bronchi and other respiratory tract diseases. The appearance of these symptoms requires emergency hospitalization, as they indicate a severe course of the hiatal hernia.
Diagnostics
Taking a history and examining the patient helps in making a diagnosis. Suspecting the development of a hiatal hernia, the doctor gives a referral for examination. He can assign:
- X-ray of the esophagus, thoracic and abdominal cavity, which is carried out in a lying position; to identify a small hernia, the study is carried out using
X-ray contrast agents (barium salts); - esophageal manometry, which allows assessing the functioning of the organ;
- examination of the gastrointestinal tract using an esophagoscope;
- tissue biopsy, which allows to exclude oncology;
- laboratory tests (stool test for occult blood, complete blood count to detect anemia);
- If chest pain develops, an electrocardiogram is prescribed to rule out angina.
Therapy
The treatment regimen is selected by the doctor depending on the clinical picture. If an asymptomatic course of pathology is observed, then a wait-and-see approach is indicated, that is, the patient should regularly visit the doctor at specific intervals to assess the dynamics of the disease.
If unpleasant symptoms appear, therapy is prescribed, which can be:
- conservative;
- surgical
With the development of a sliding hernia of 1st and 2nd degrees, they usually resort to conservative treatment, which includes diet therapy and medication.
Products that irritate the mucous membranes of the gastrointestinal tract should be excluded from the patient’s diet, namely:
- smoked meats;
- pickles;
- marinades;
- spicy and fermented dishes.
You need to eat little and often. Dishes should be warm and crushed to a homogeneous consistency.
Medicines prescribed:

It must be remembered that self-medication with these drugs is not acceptable, since each of them has its own contraindications and undesirable effects, and only a doctor can choose the right medication and its dosage.
Physiotherapy exercises are also indicated for hiatal hernia.
If conservative therapy is ineffective, surgery is performed.
With the development of paraesophageal and combined hernia, surgical treatment is prescribed more often, since with such development of pathology there is a high risk of complications. During the operation, the diaphragmatic opening is sutured and the stomach is fixed to the abdominal wall.
Consequences and prevention
Complications
Hiatal hernia can provoke pathologies such as:
- gastroesophageal reflux disease;
- peptic ulcer and narrowing of the esophagus;
- internal bleeding;
- strangulated hernia;
- protrusion of the gastric mucosa into the esophagus;
- violation of the integrity of the walls of the esophagus.
Patients with a hiatal hernia should be registered with a gastroenterologist. They need to undergo medical examination at least once every six months.